Case Number : Case 918 - 27th December Posted By: Guest
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
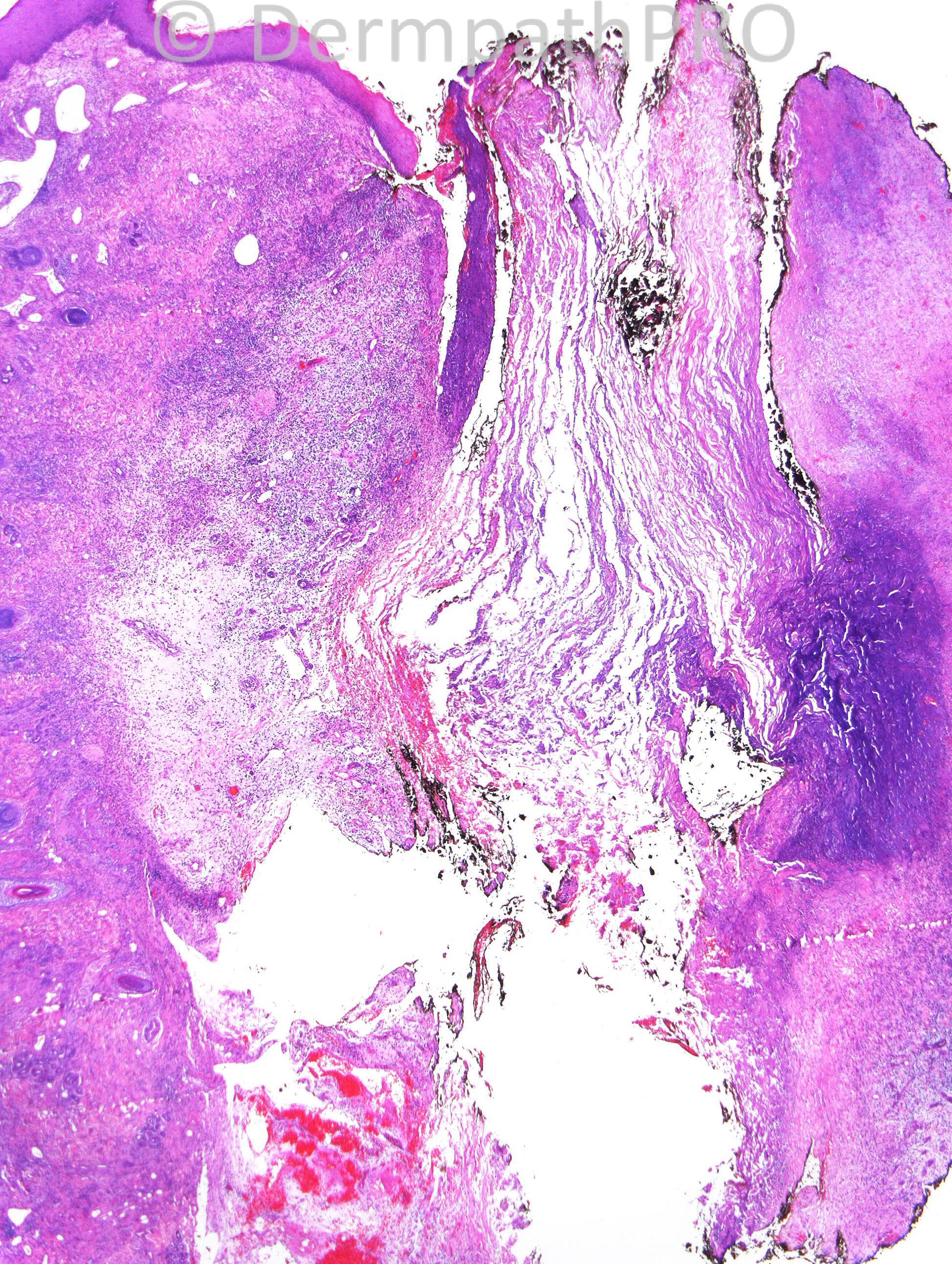
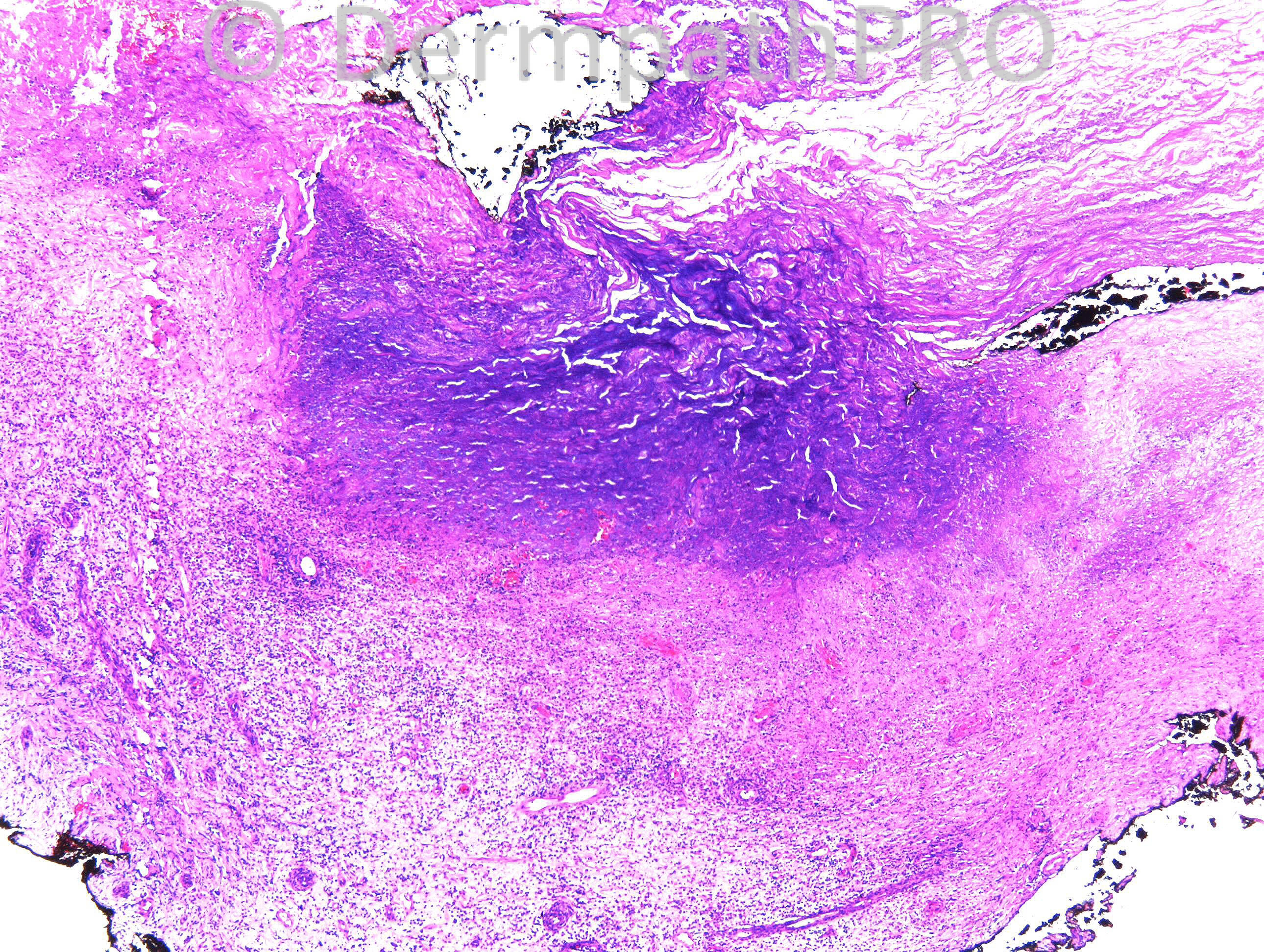
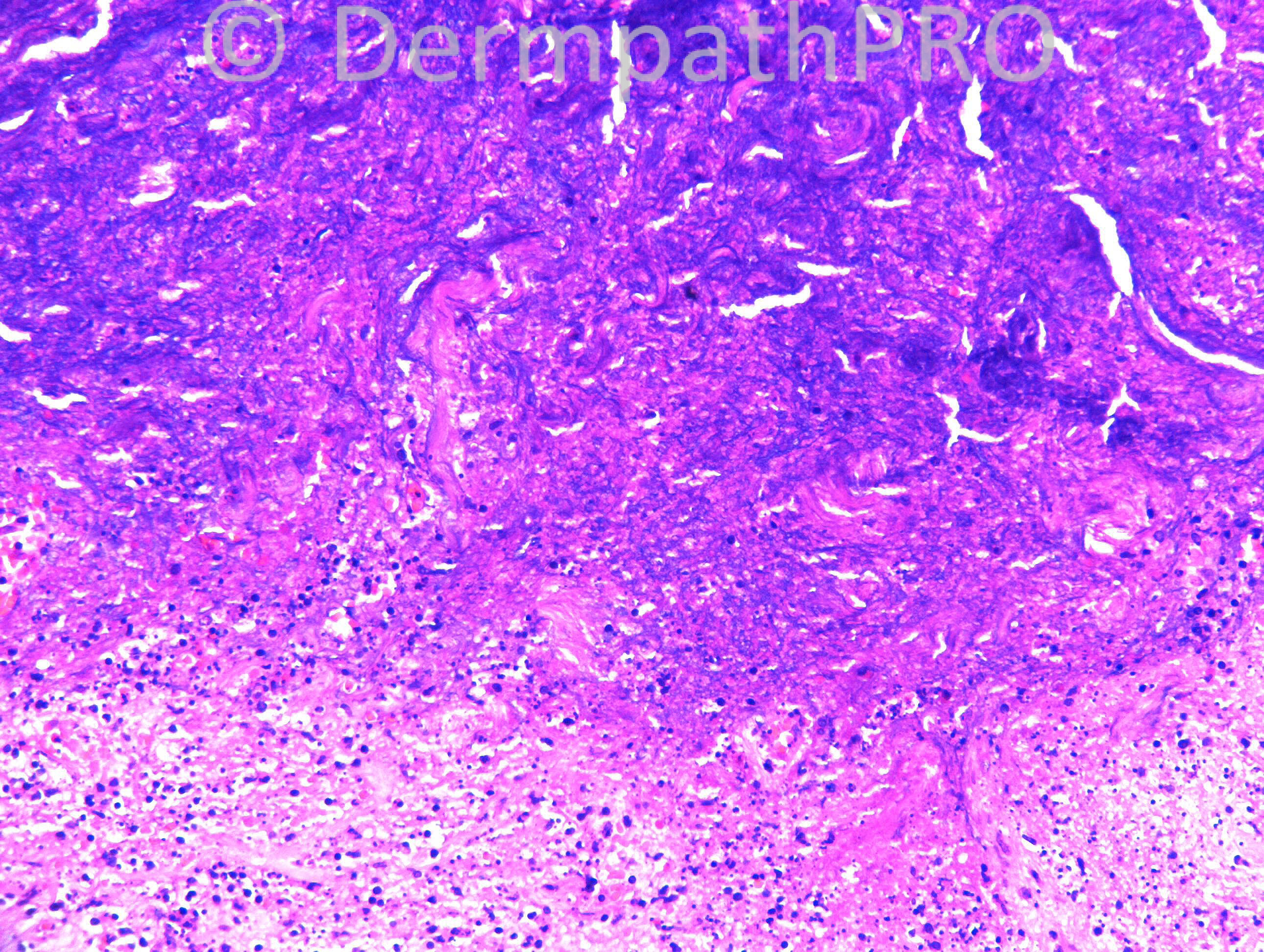
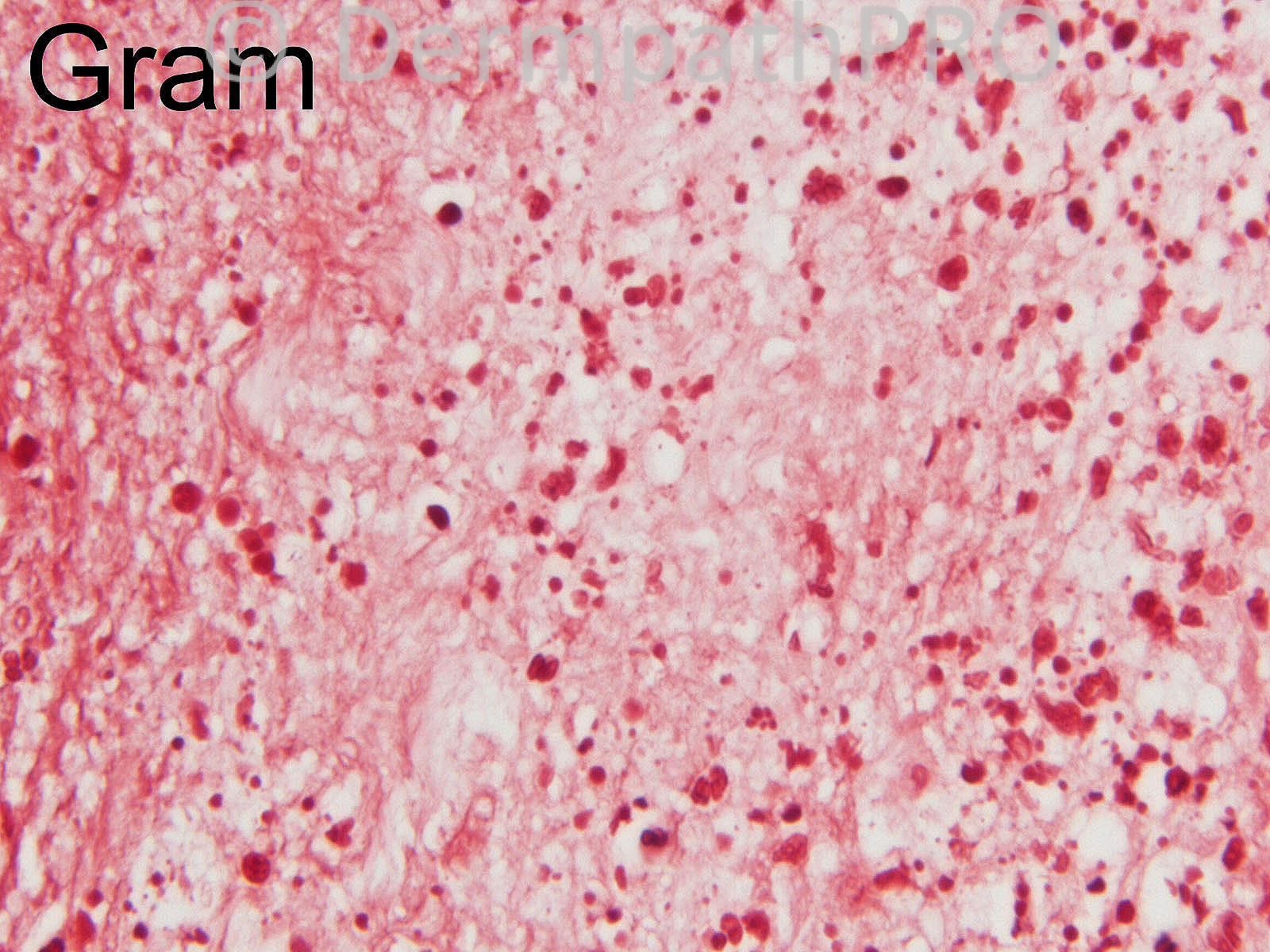
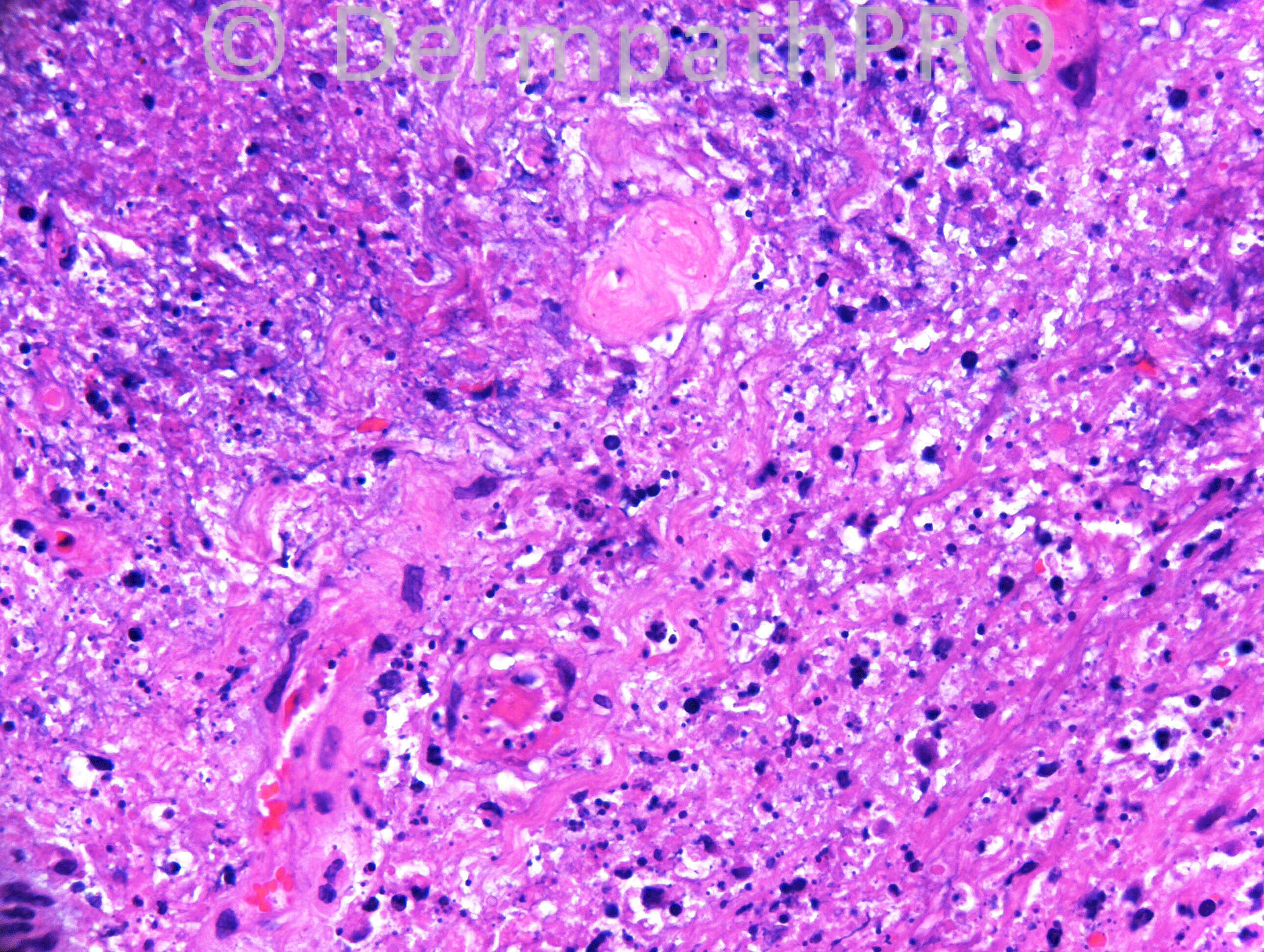
F69. Has CLL. Scalp vesicles Rx’d by GP as Zoster but developed large unilateral area of black ulcerated scalp. Swabs growing pseudomonas.
Case posted by Dr. Richard Carr.
Case posted by Dr. Richard Carr.

Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.