Case Number : Case 687 - 1 Feb Posted By: Guest
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
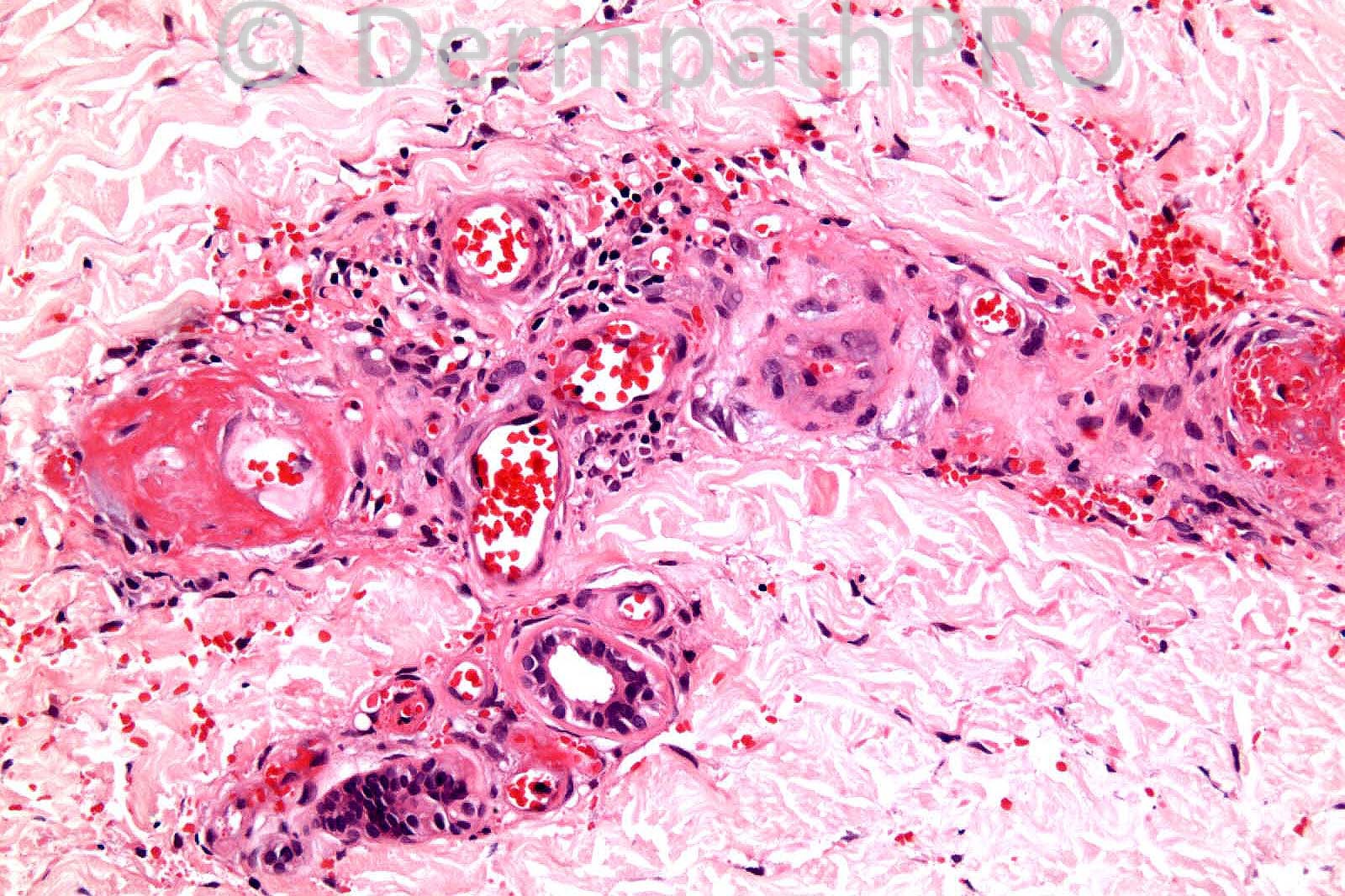
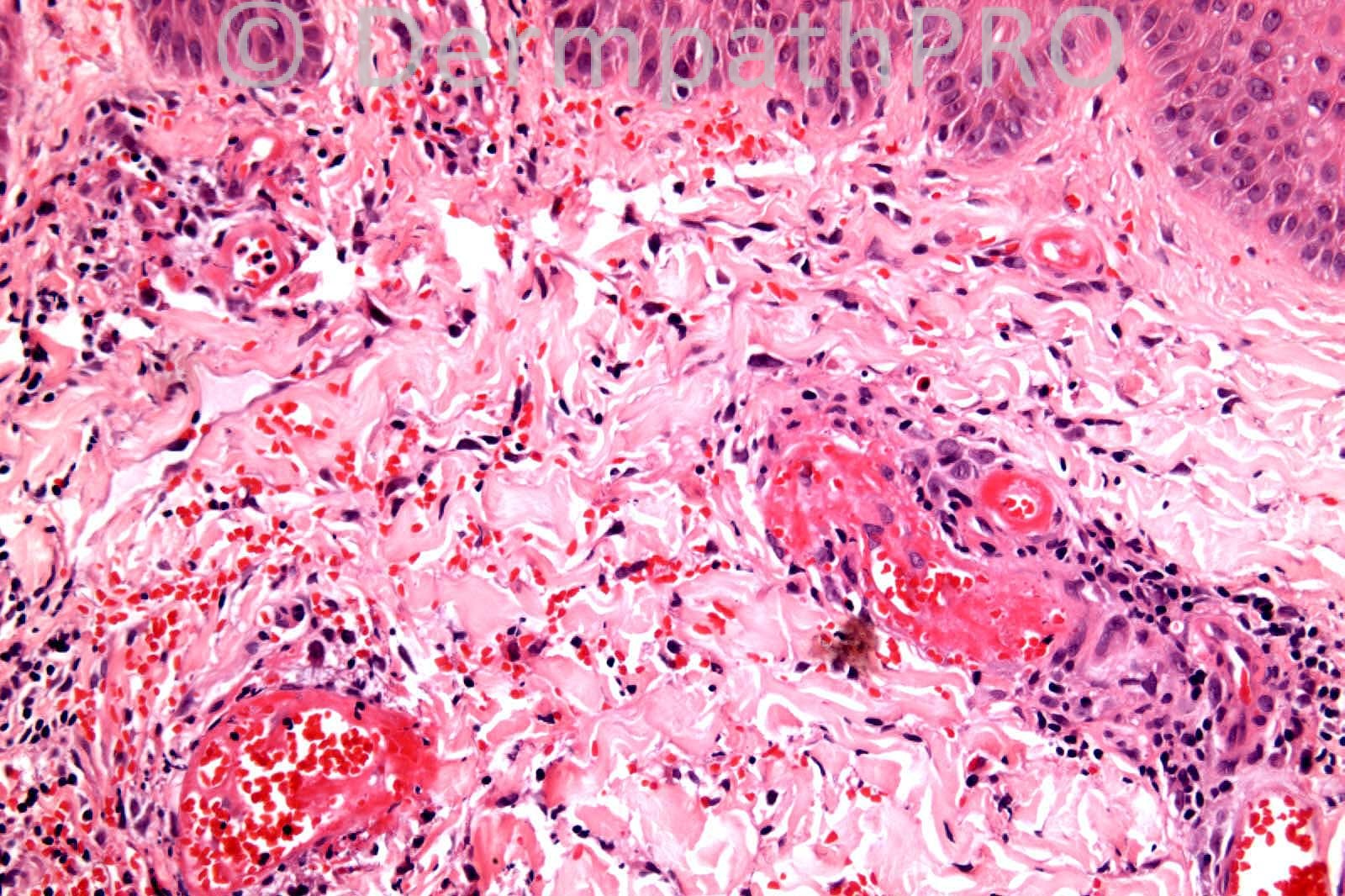
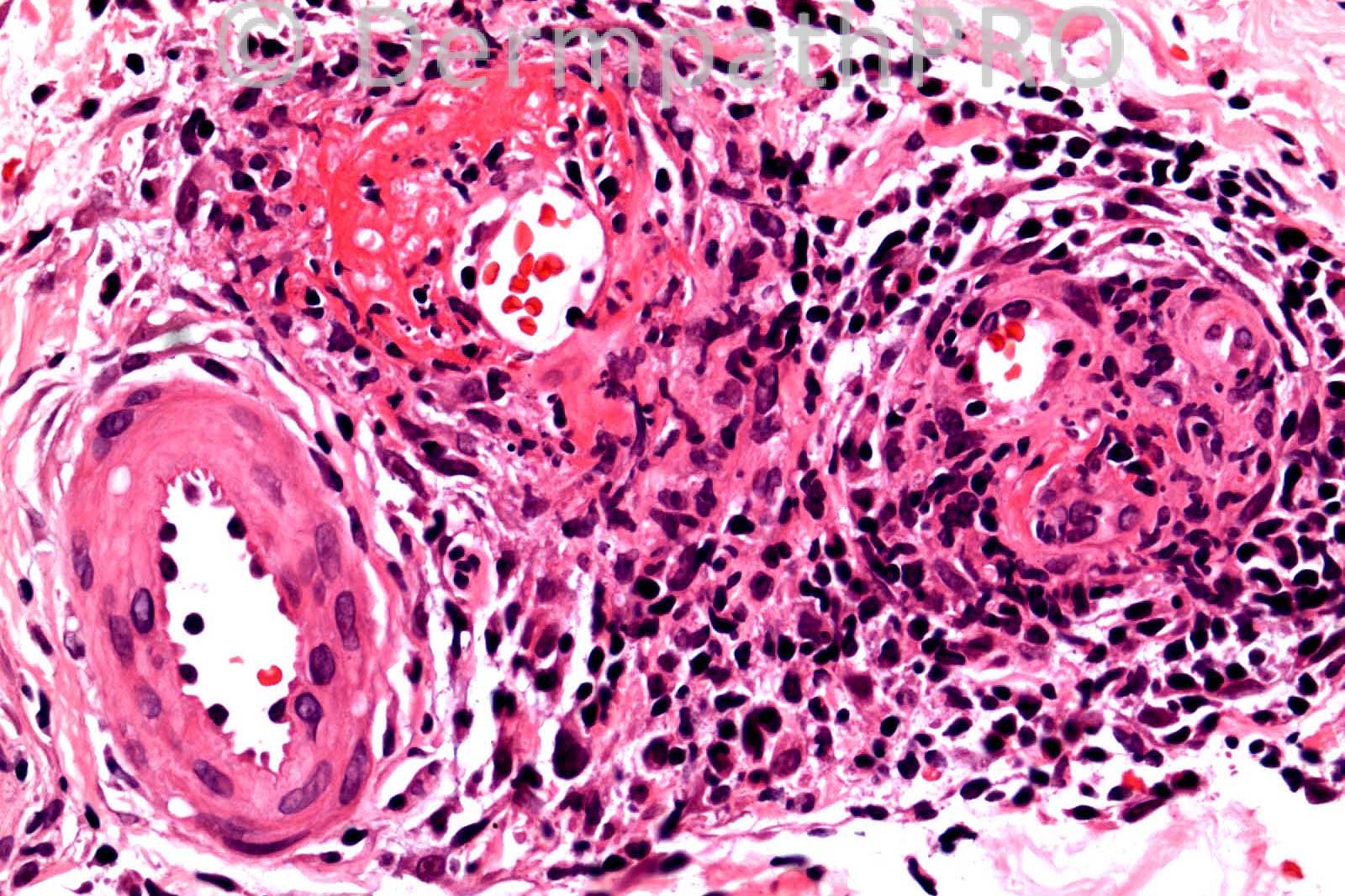
26 years-old female. Necrotic and purpuric lesions on lower legs.
Case posted by Dr. Richard Carr.
Case posted by Dr. Richard Carr.


User Feedback