Case Number : Case 766 - 24th May Posted By: Guest
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
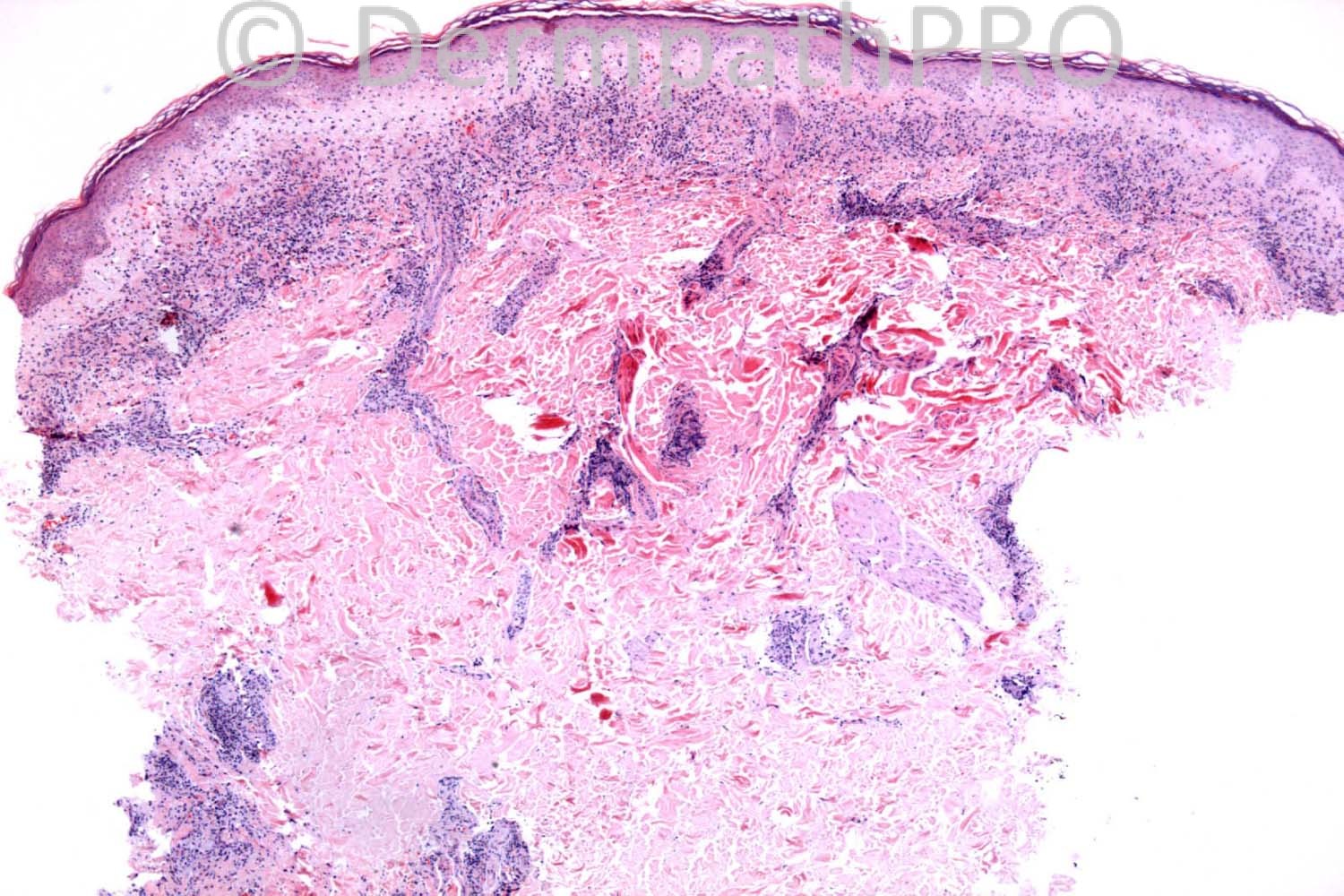
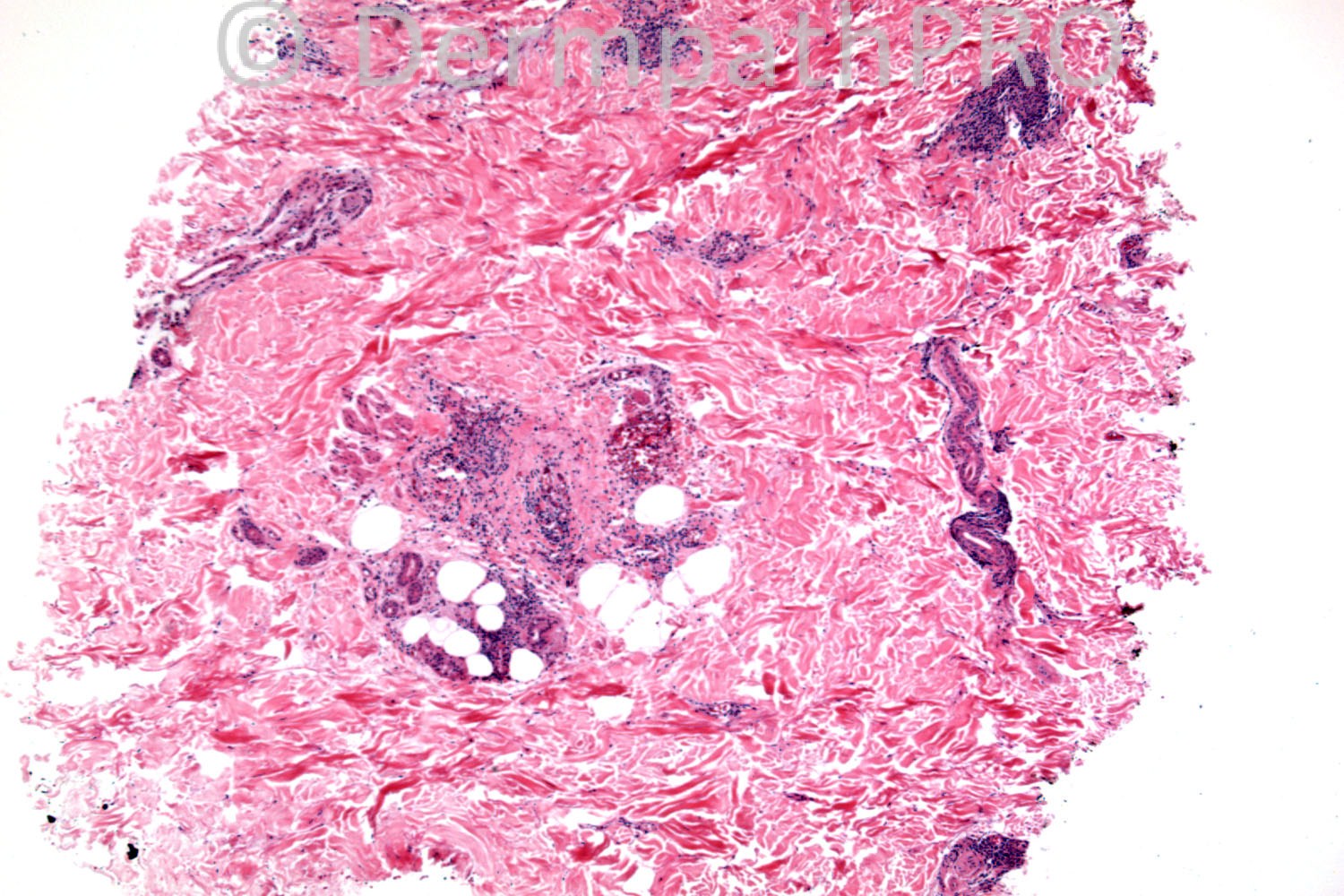
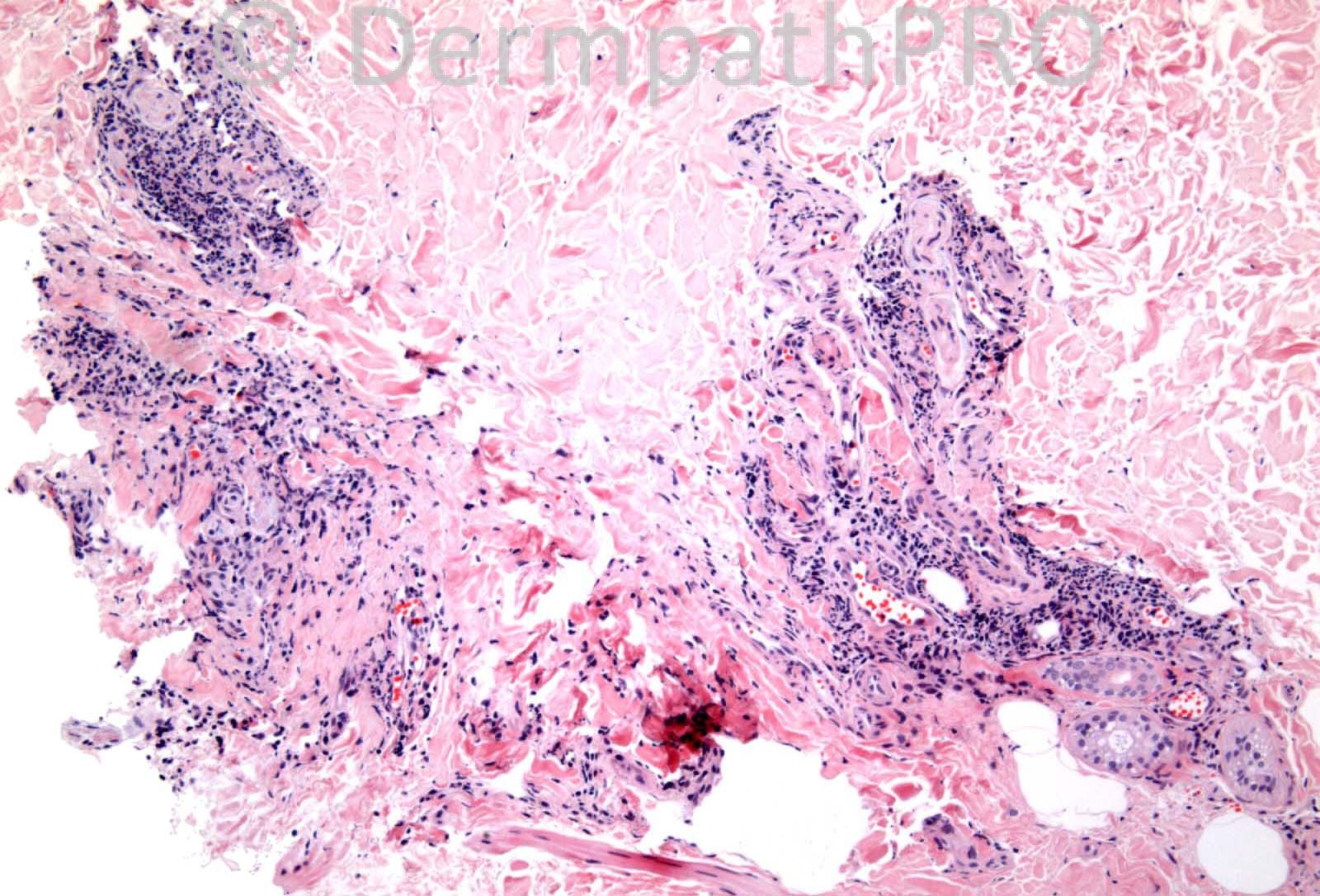
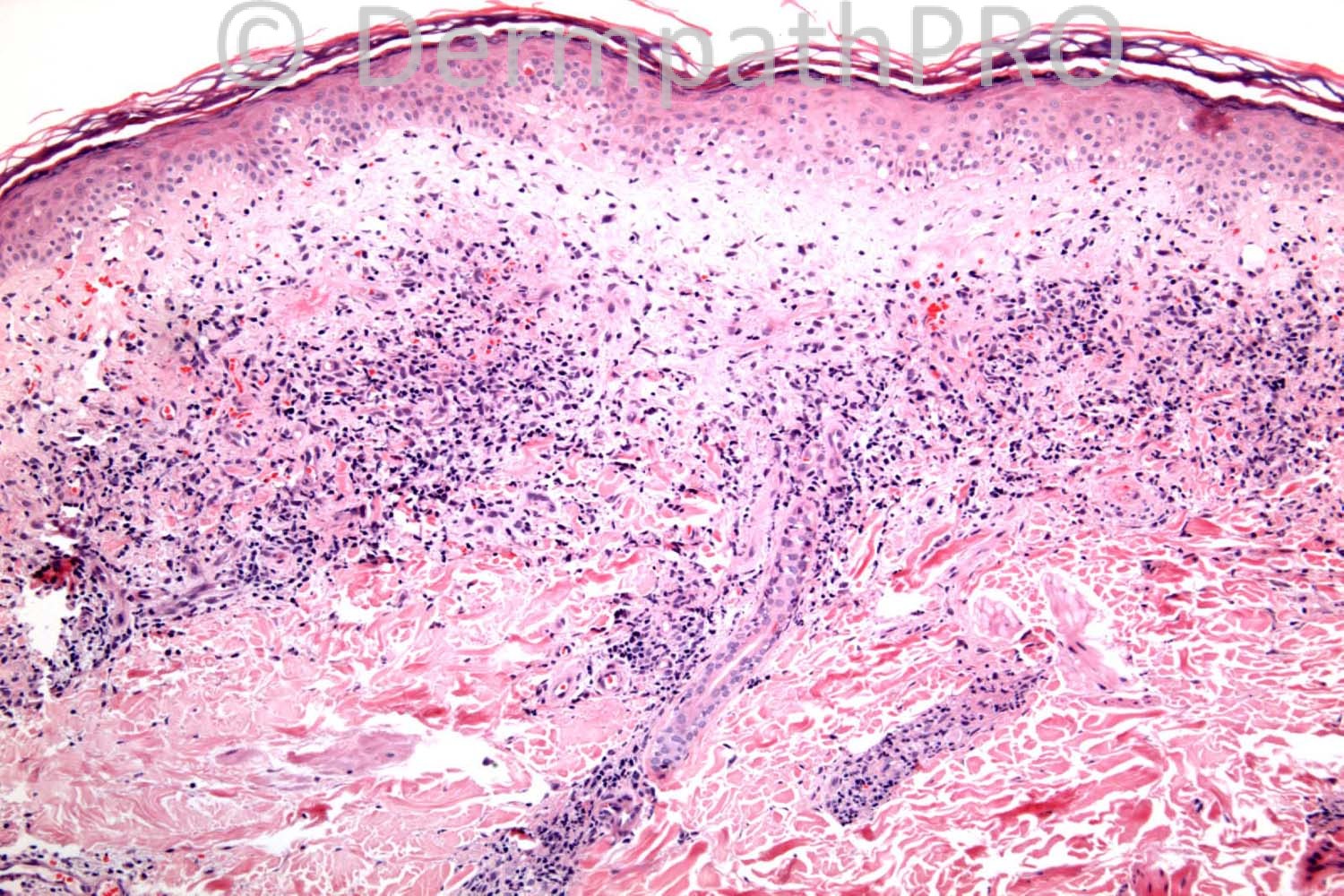
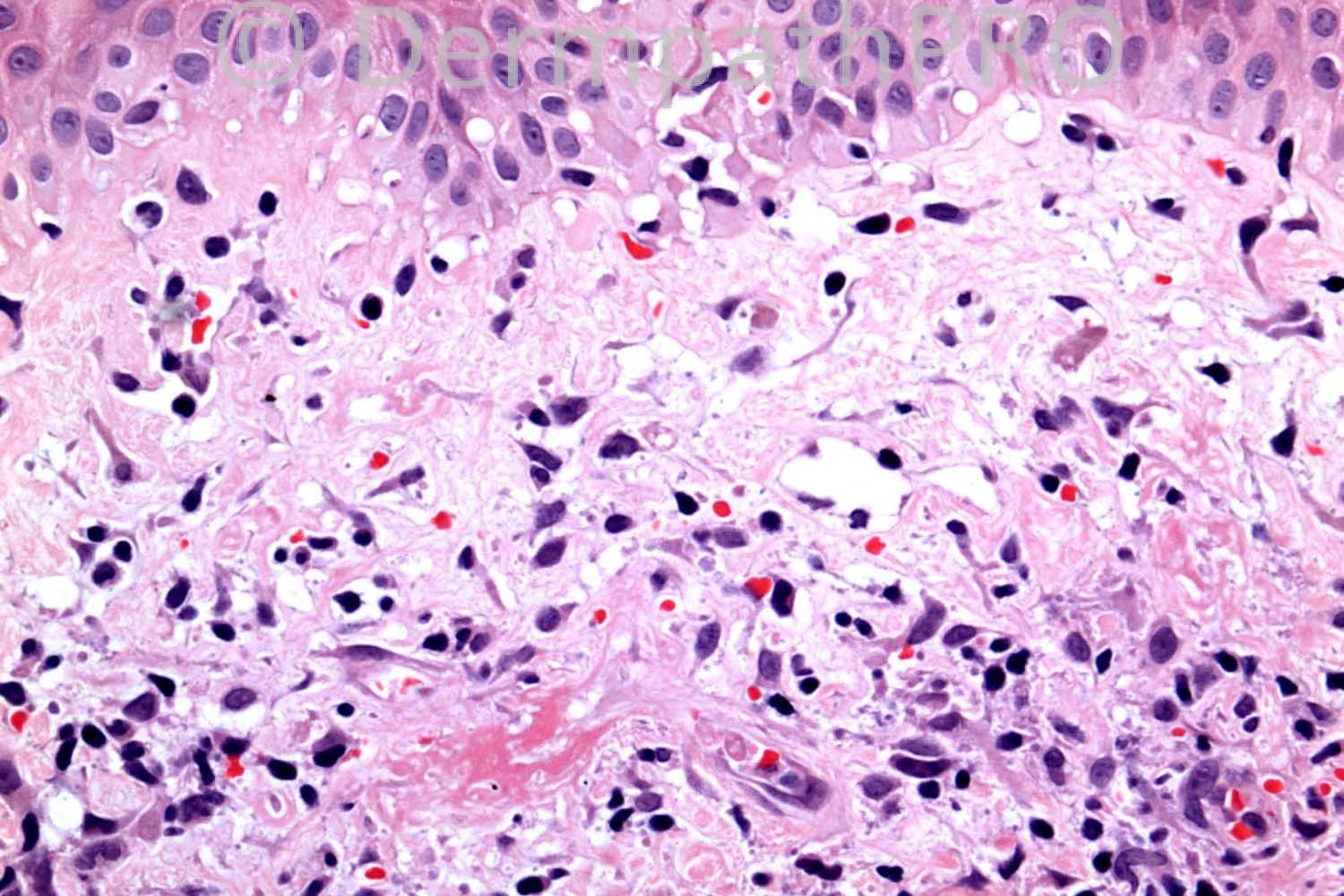
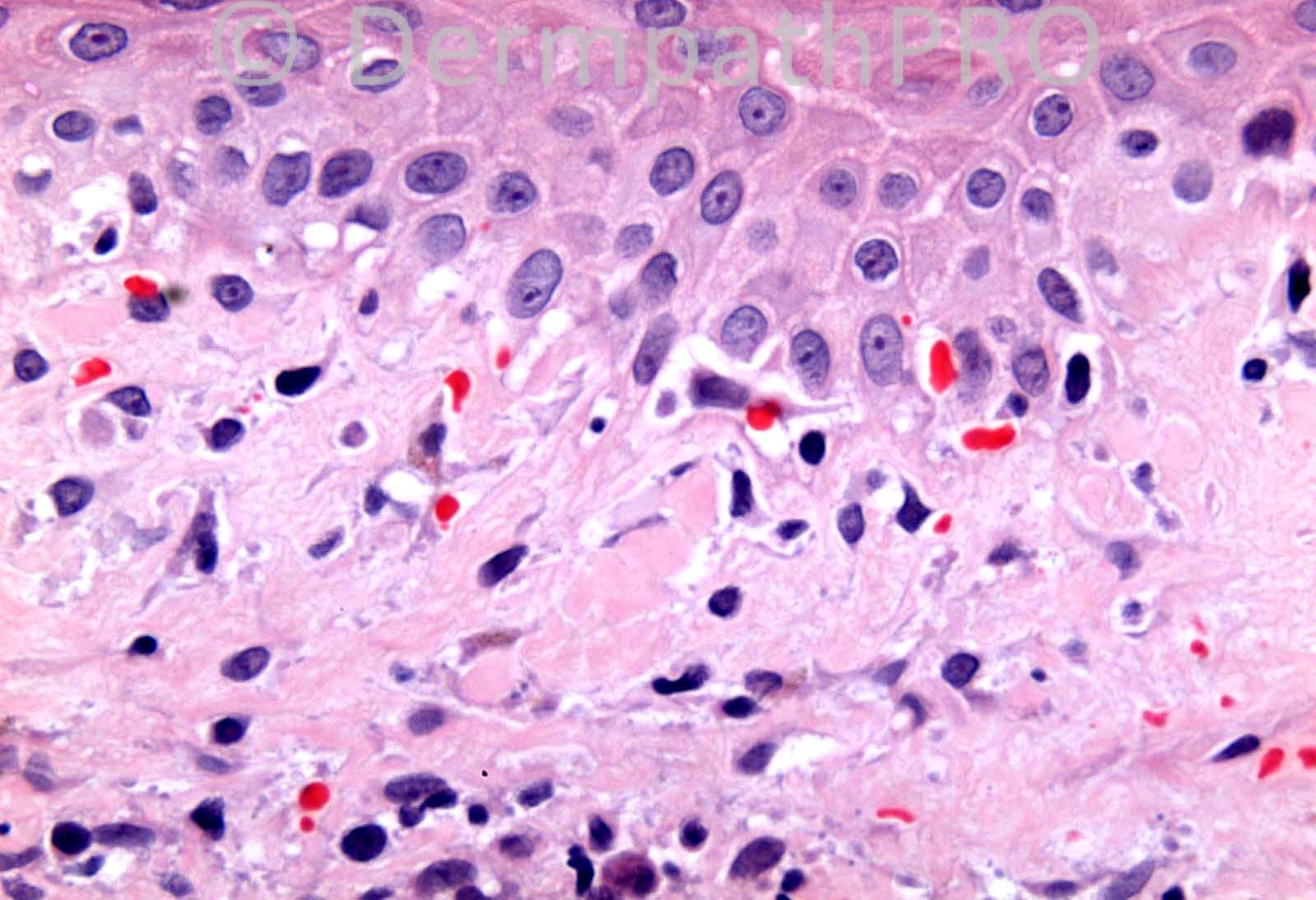
55 years-old male. Diabetic. Rash on right buttock. ?Necrobiosis lipoidica.
Case posted by Dr. Richard Carr.
Case posted by Dr. Richard Carr.

User Feedback