Case Number : Case 896 - 25th November Posted By: Guest
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
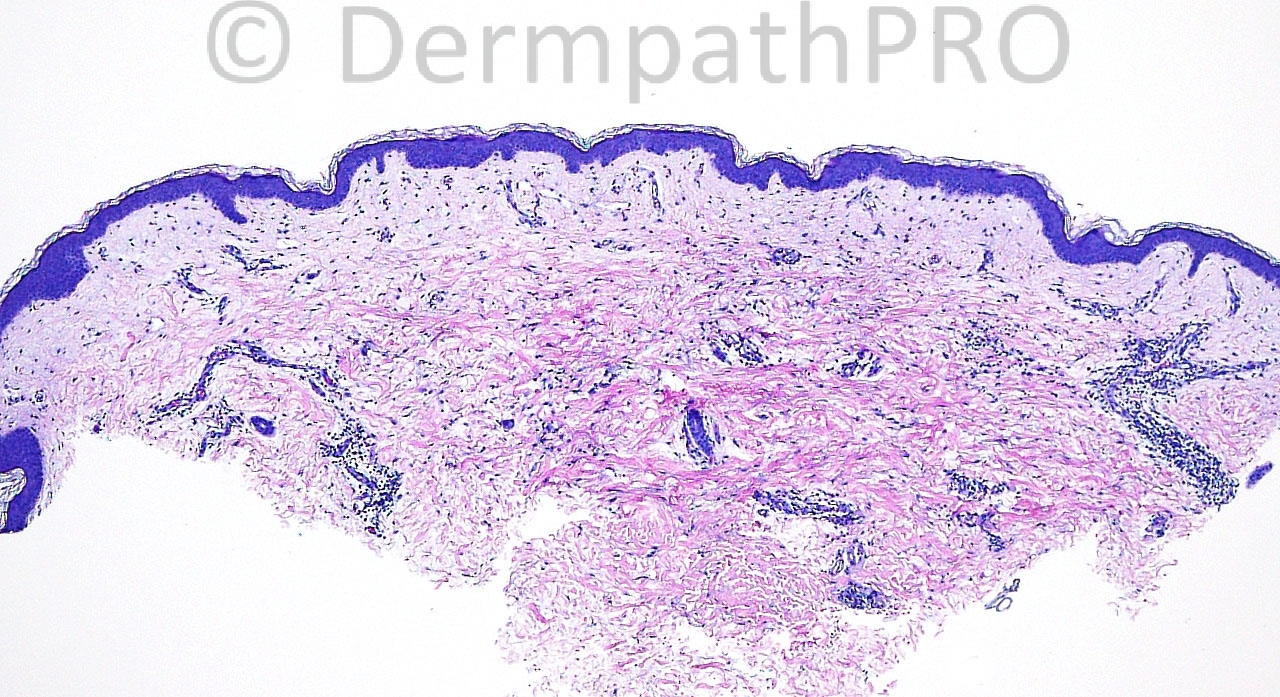
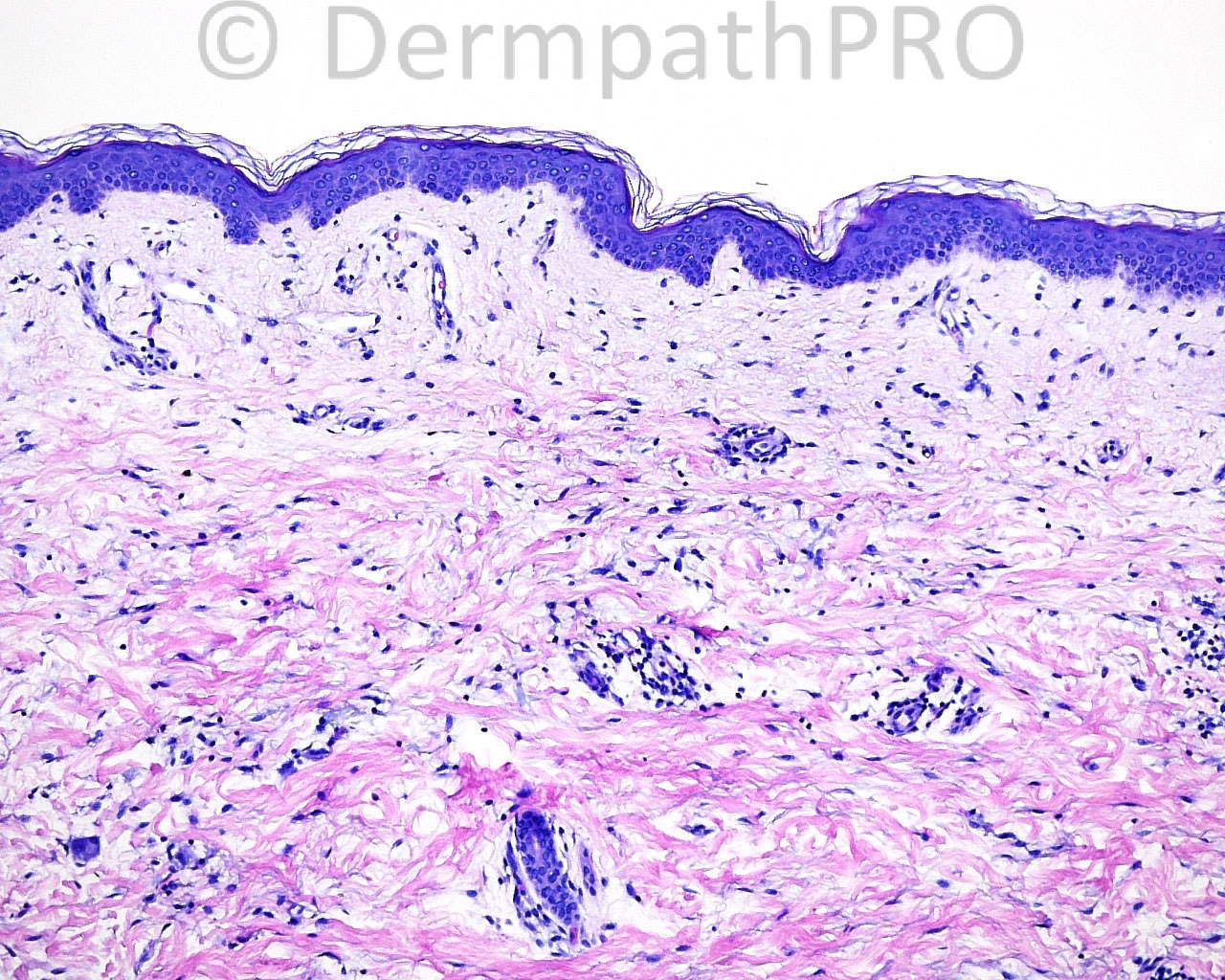
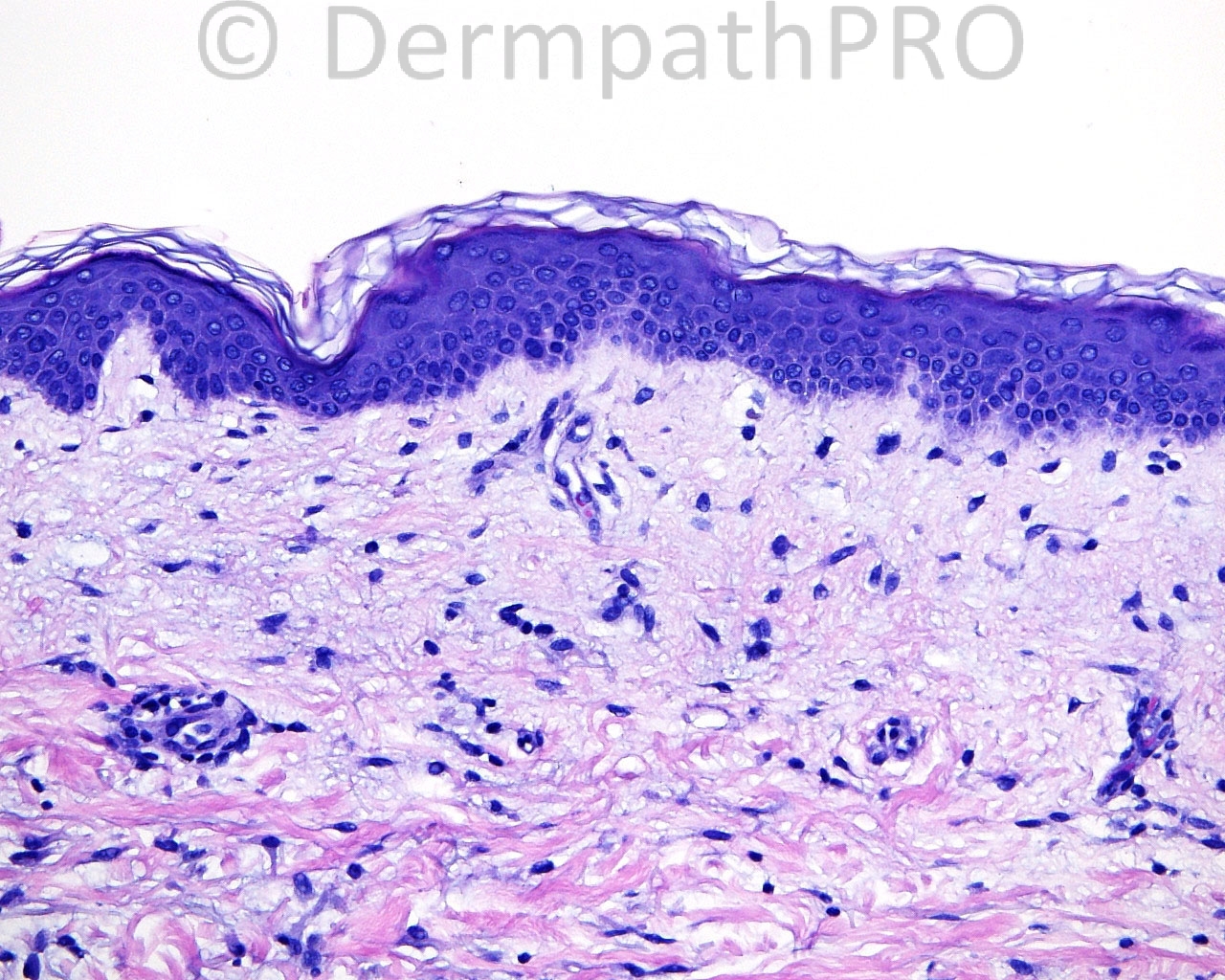
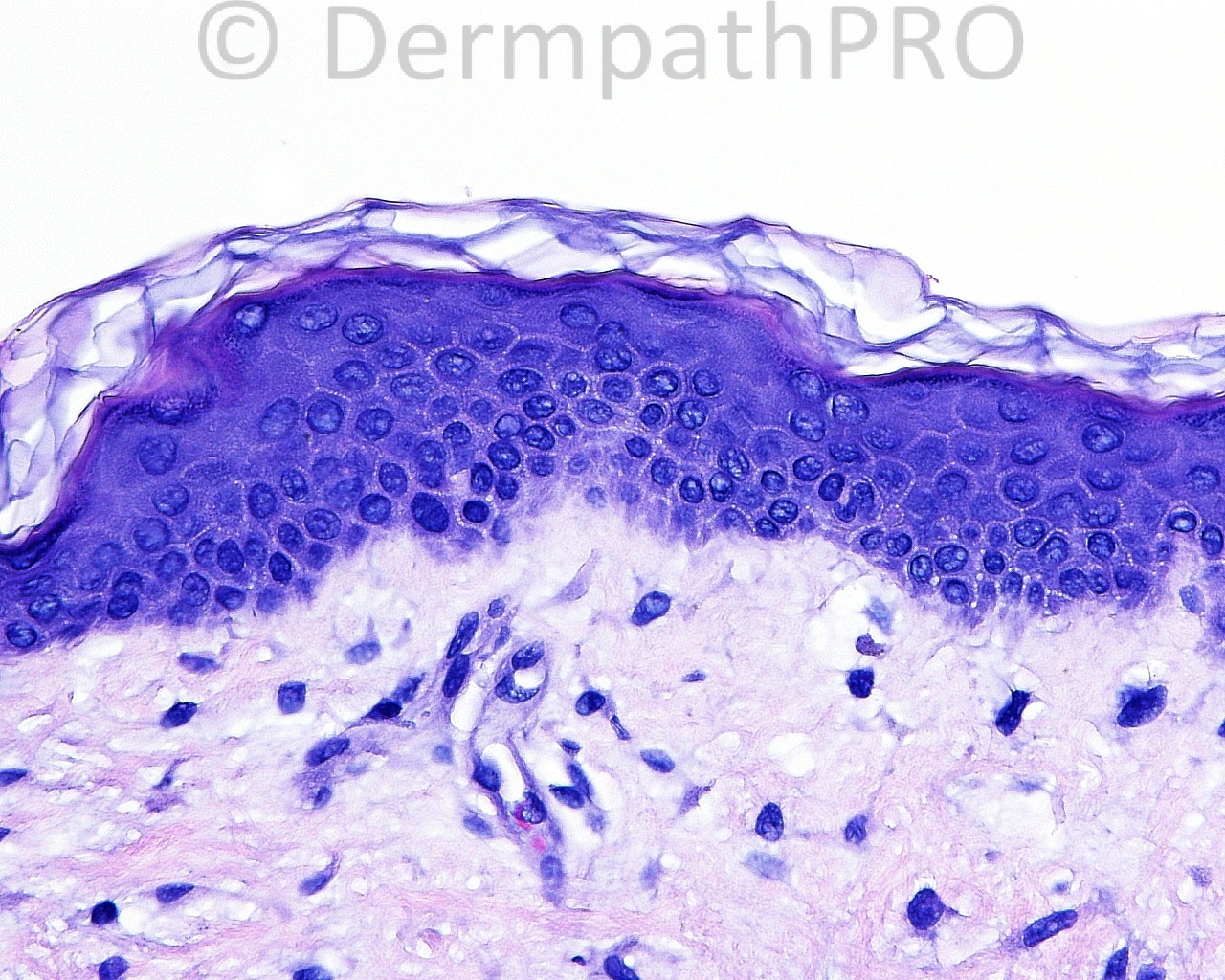
The patient is a 59 year old woman with punch biopsies taken from the right groin fold.
Case posted by Dr. Mark Hurt
Case posted by Dr. Mark Hurt

Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.