Case Number : Case 863 - 8th October Posted By: Guest
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
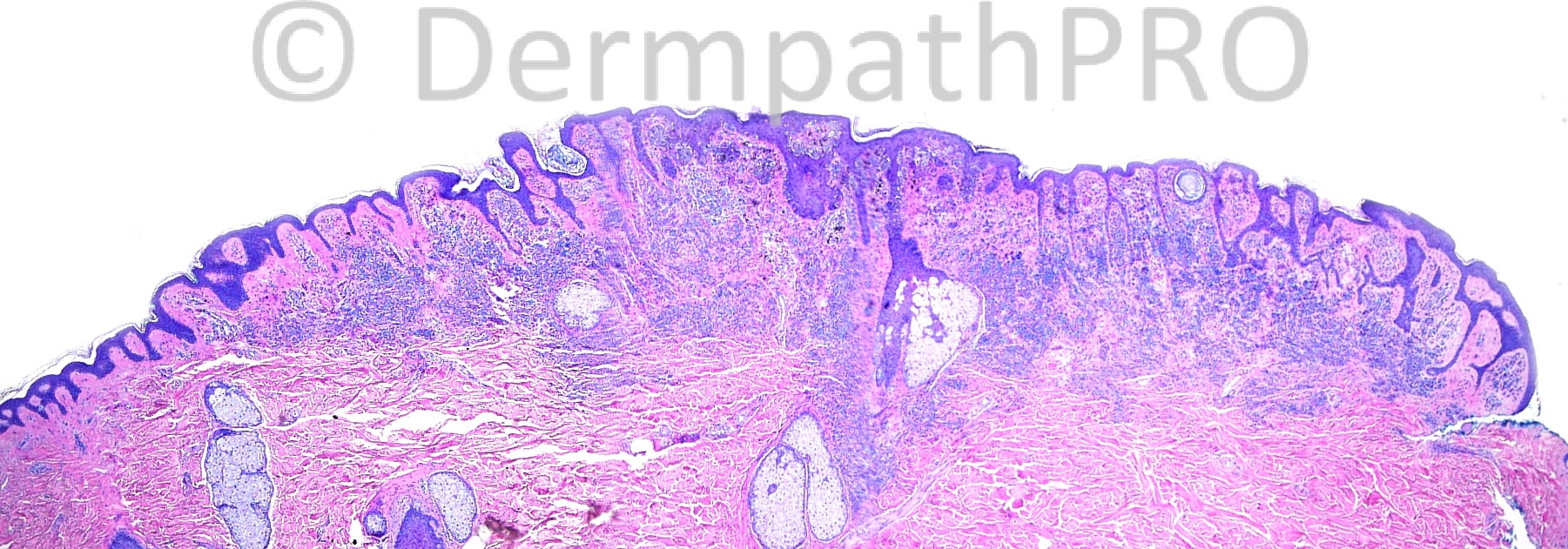
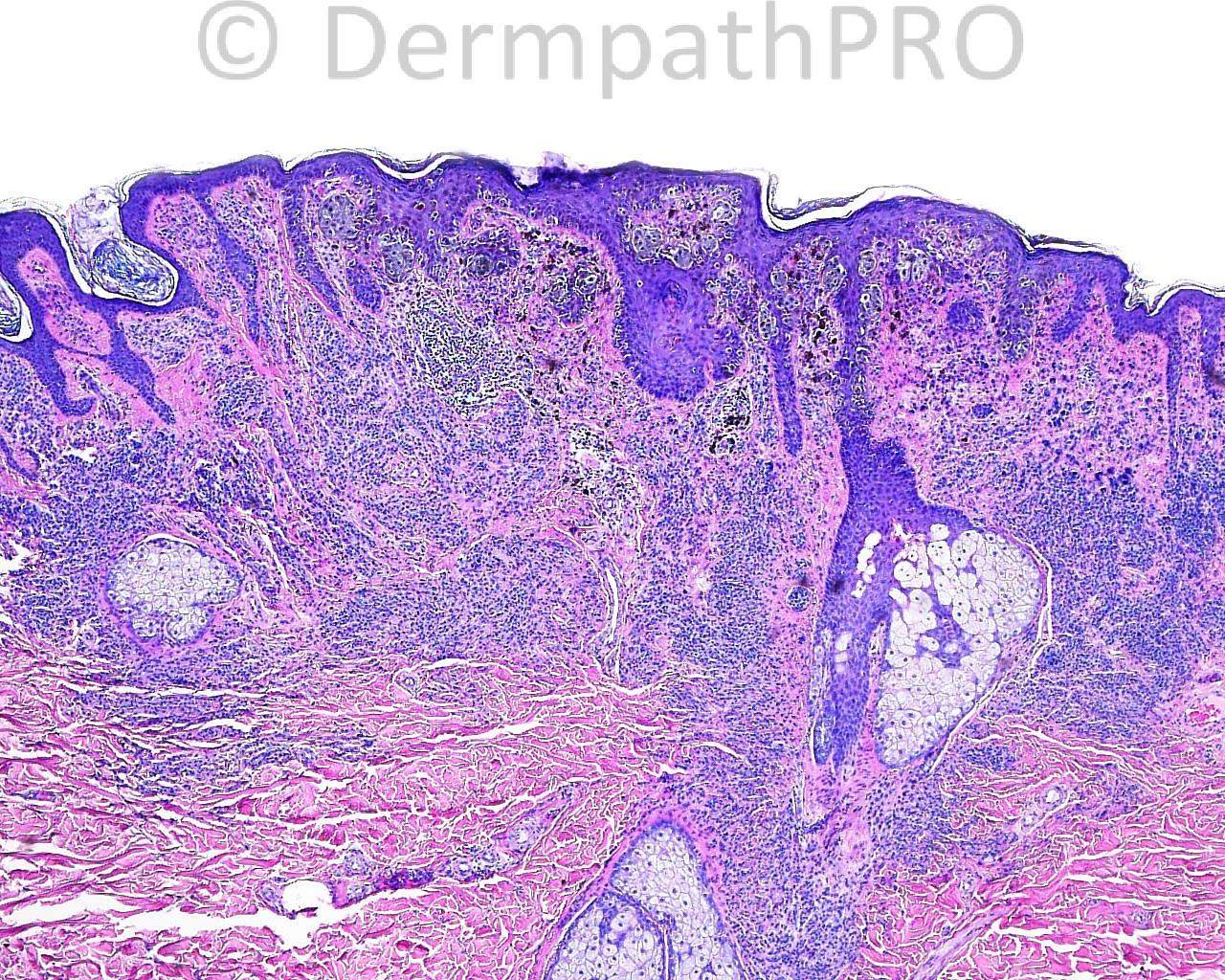
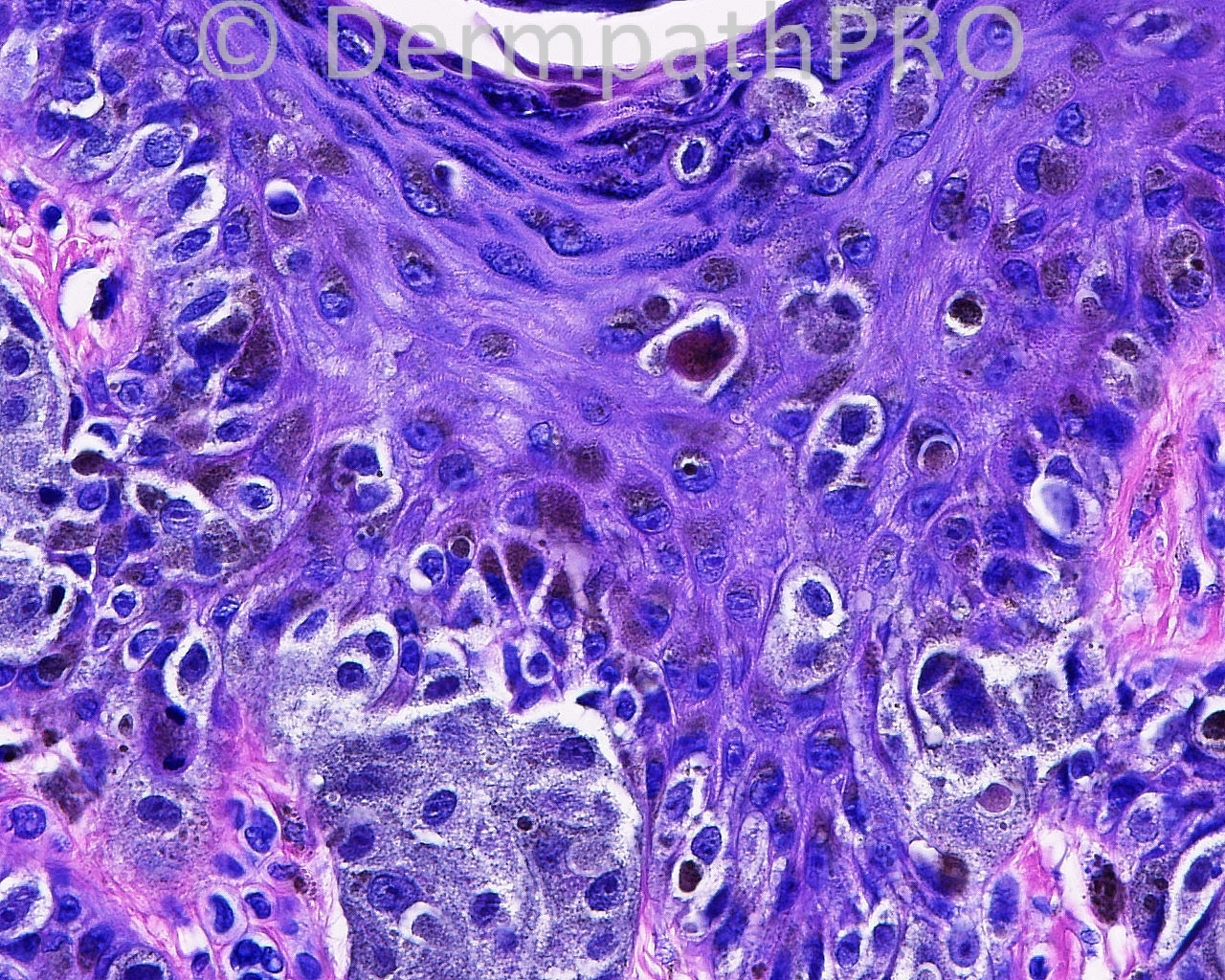
The patient is a 53 year old man with an excision with margin exam of an irregular brown papule taken from the right trapezial neck.
Case posted by Dr. Mark Hurt.
Case posted by Dr. Mark Hurt.



Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.