Case Number : Case 875 - 25th October Posted By: Guest
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
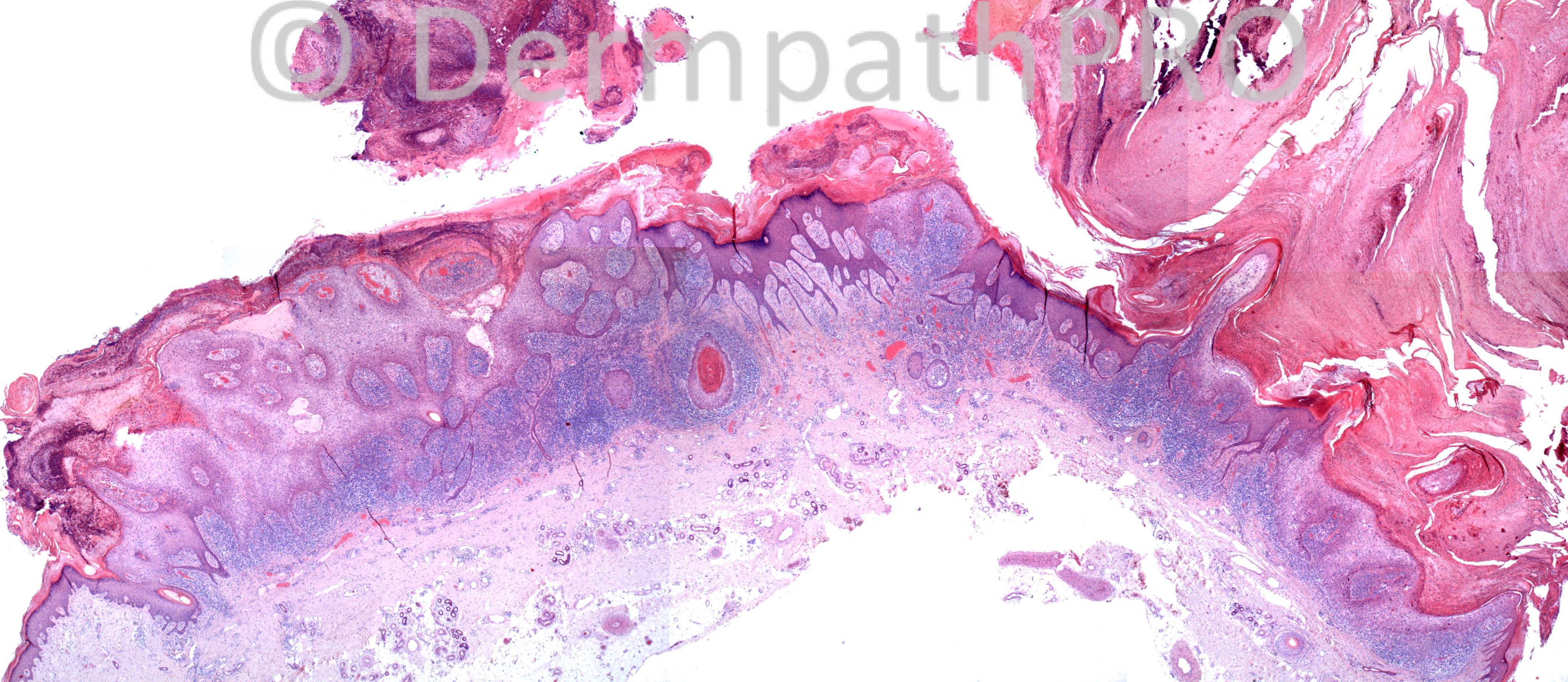
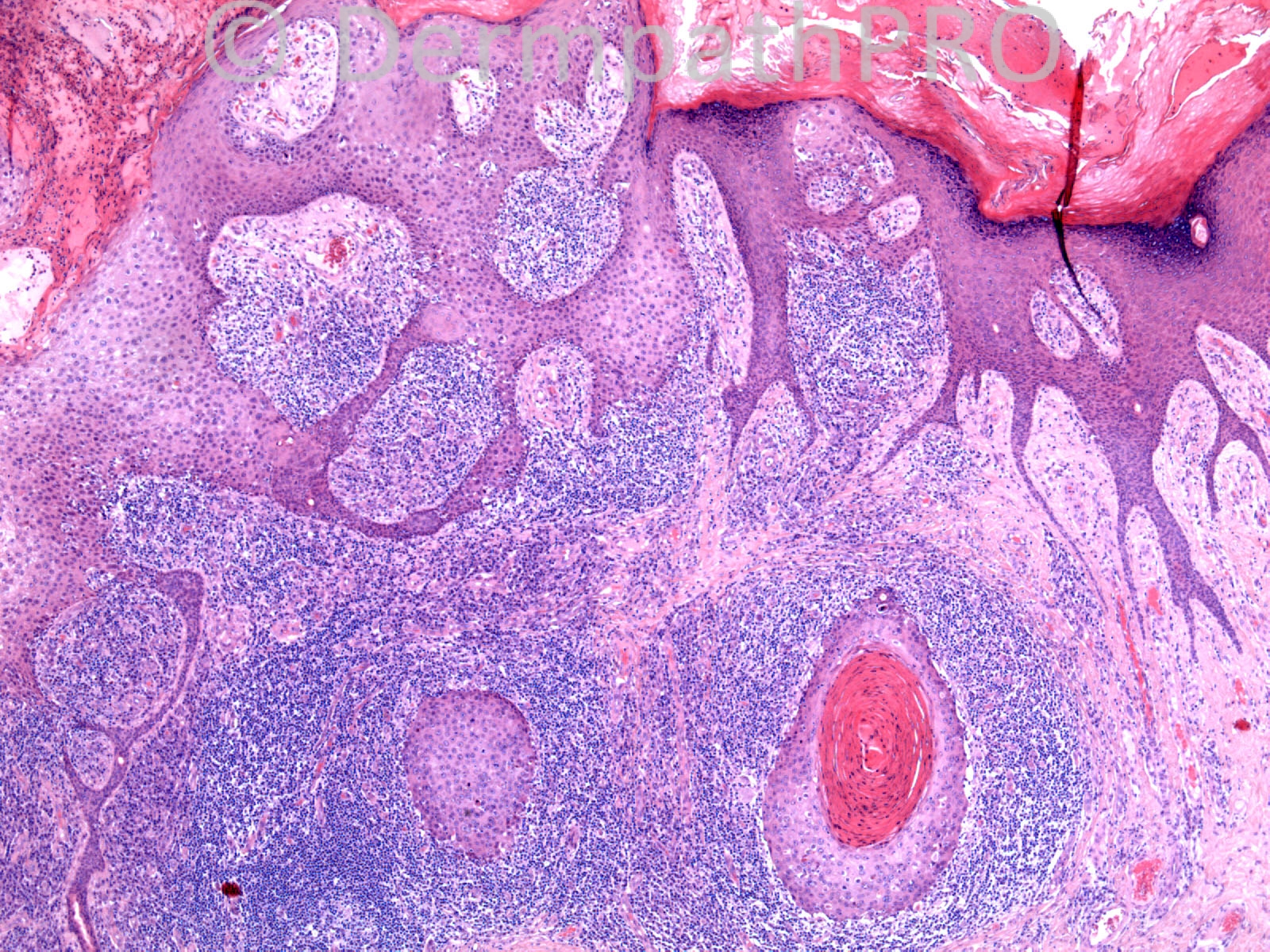
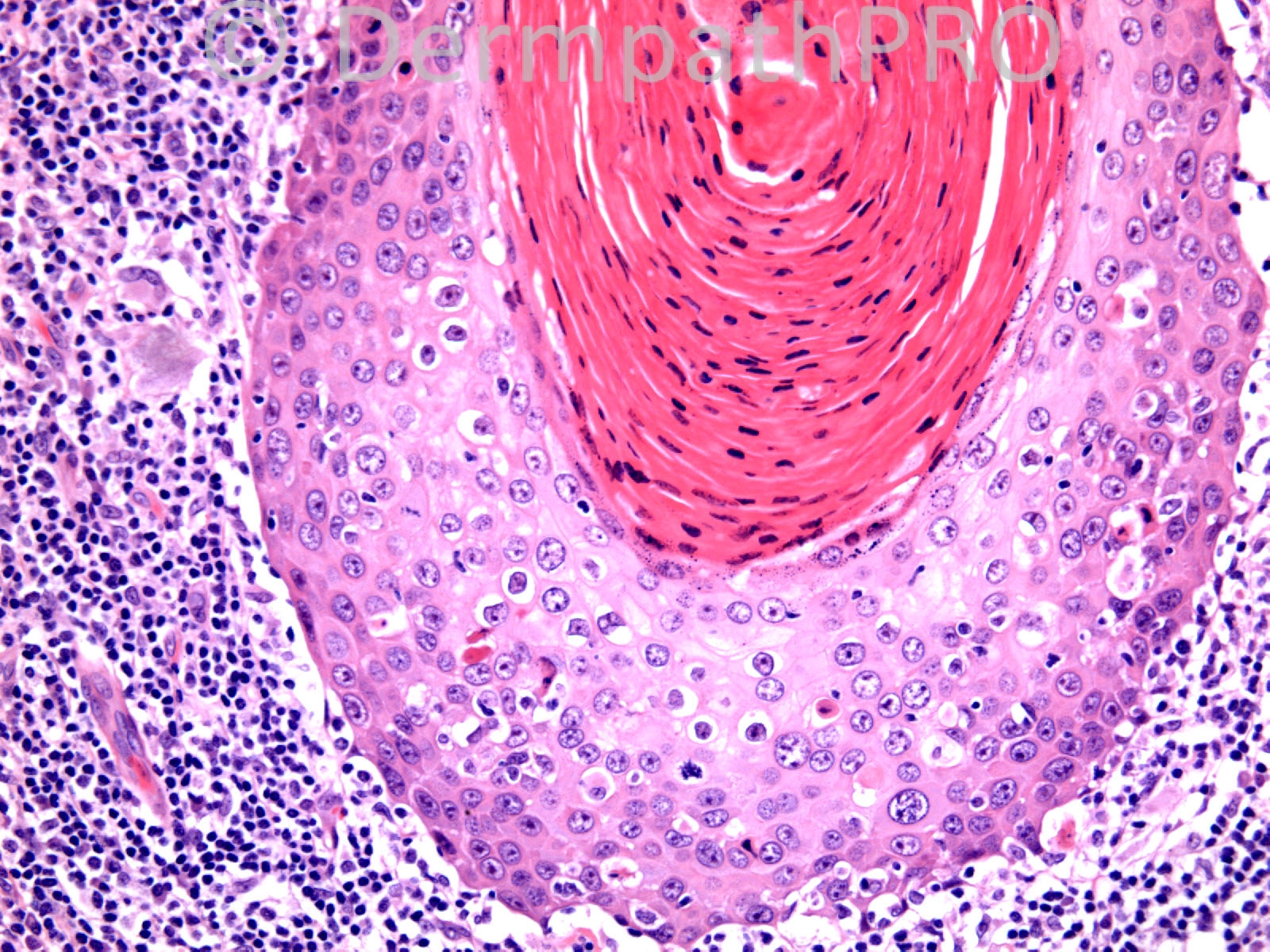
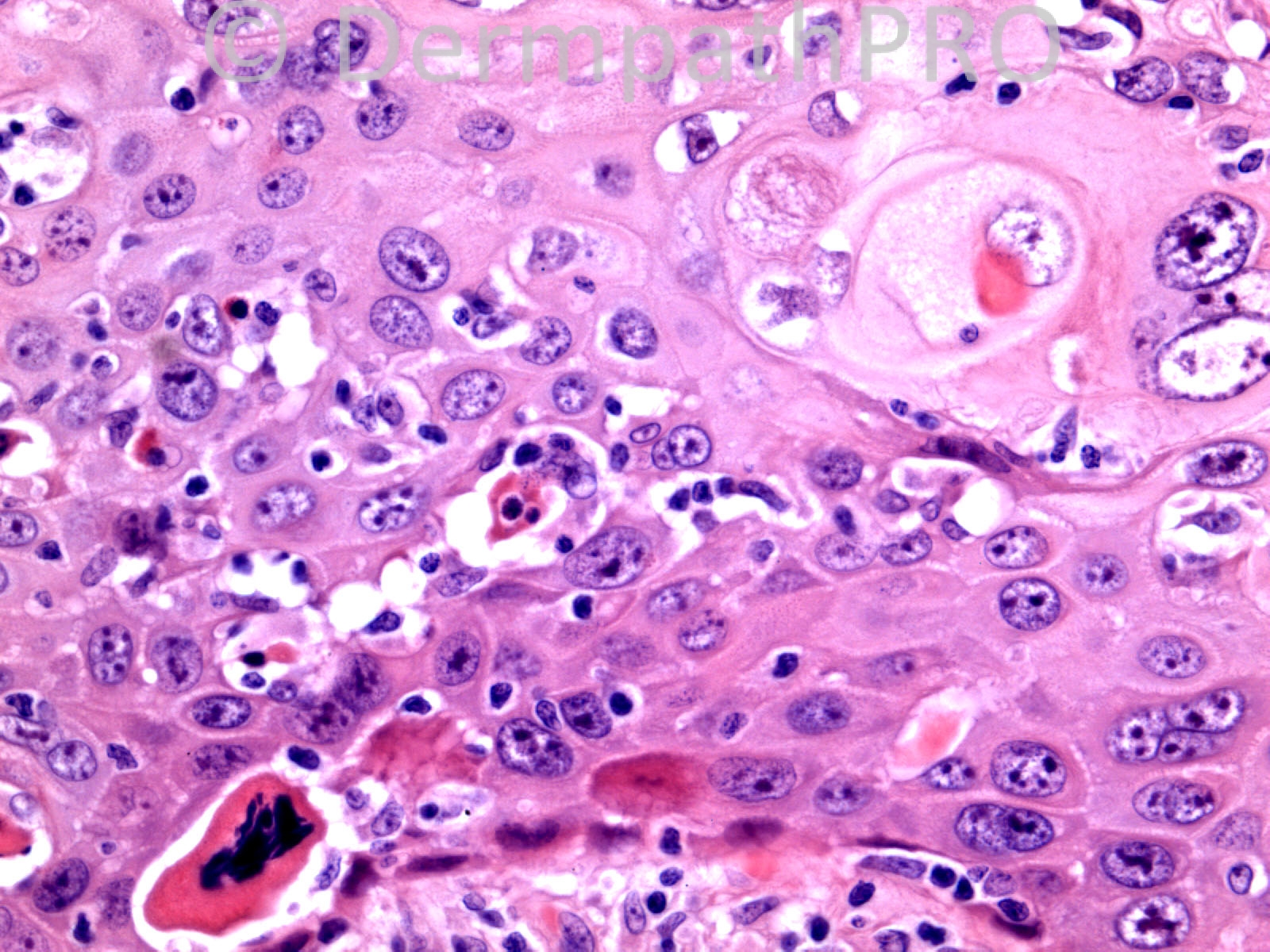
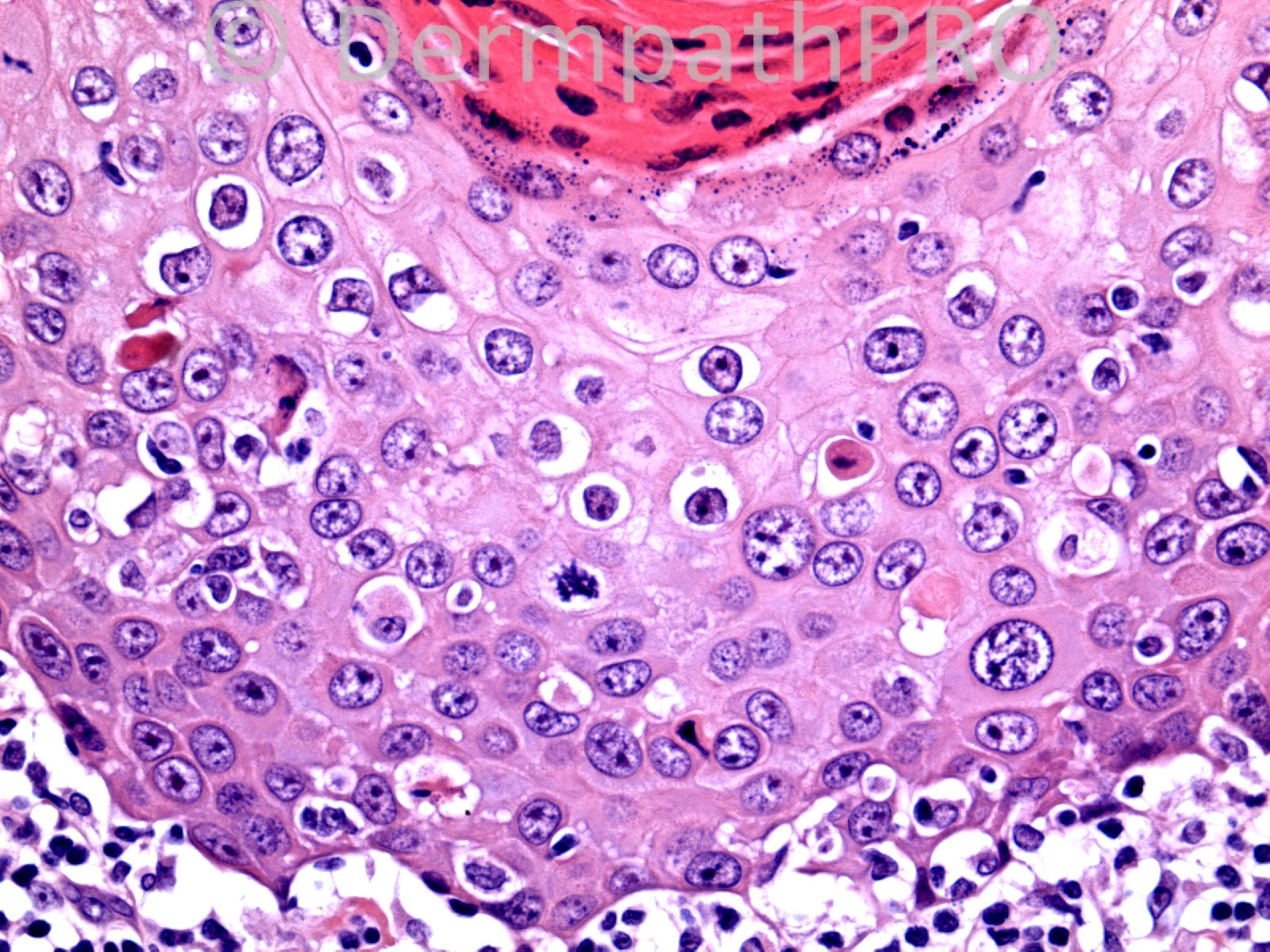
74 years old male. 3cm keratotic nodule right hand.
Case posted by Dr. Richard Carr.
Case posted by Dr. Richard Carr.

Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.