Case Number : Case 856 - 27th September Posted By: Guest
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
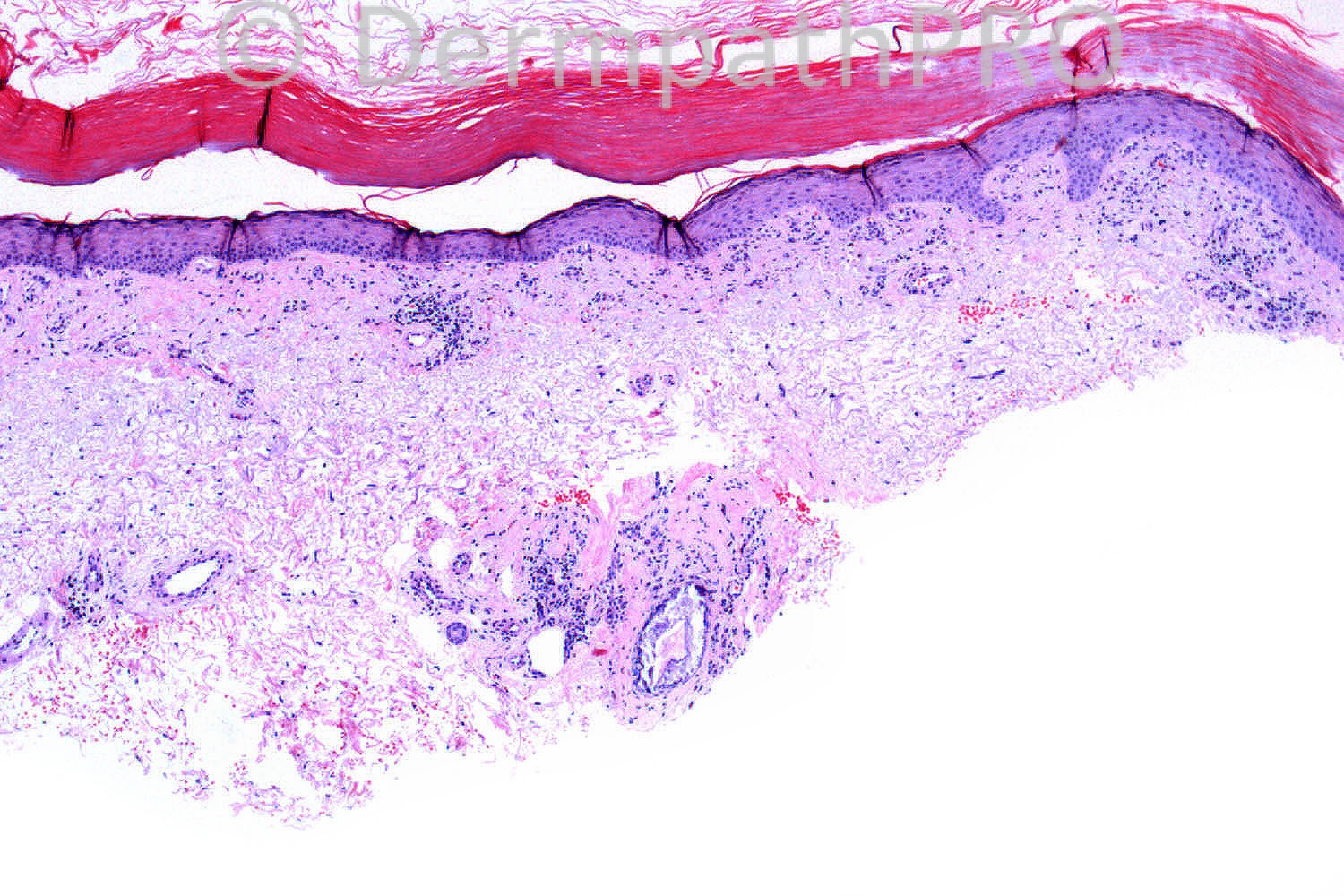
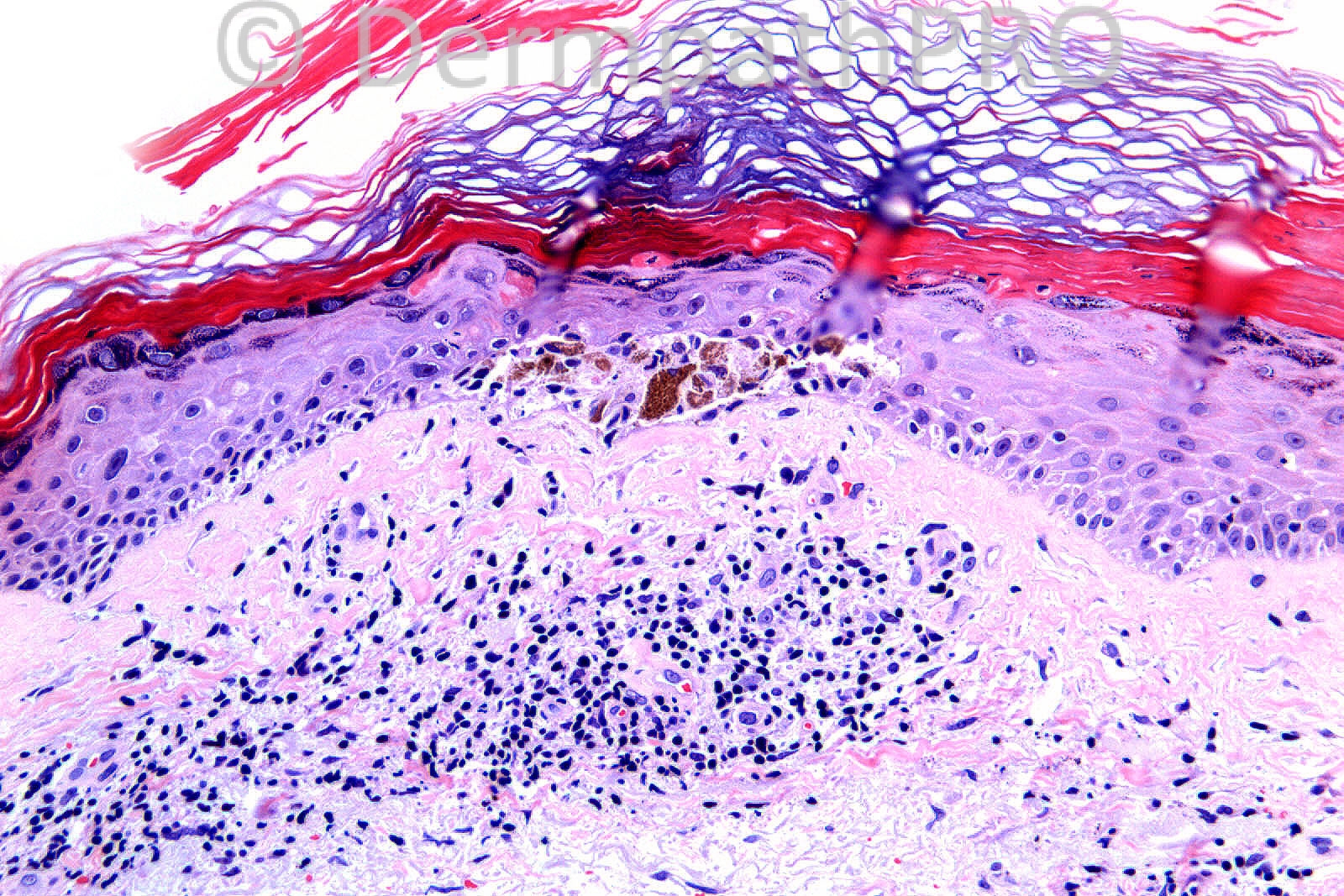
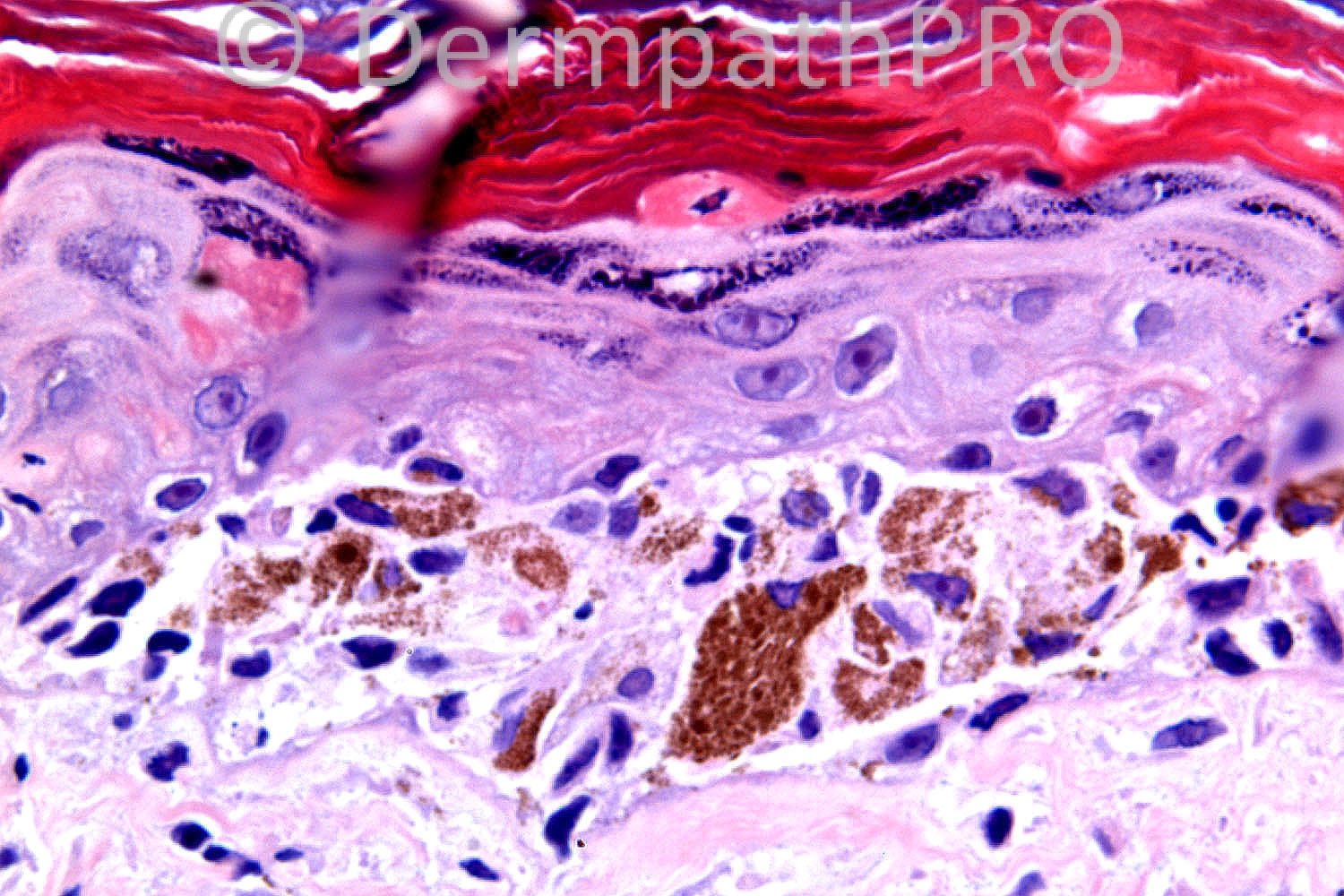
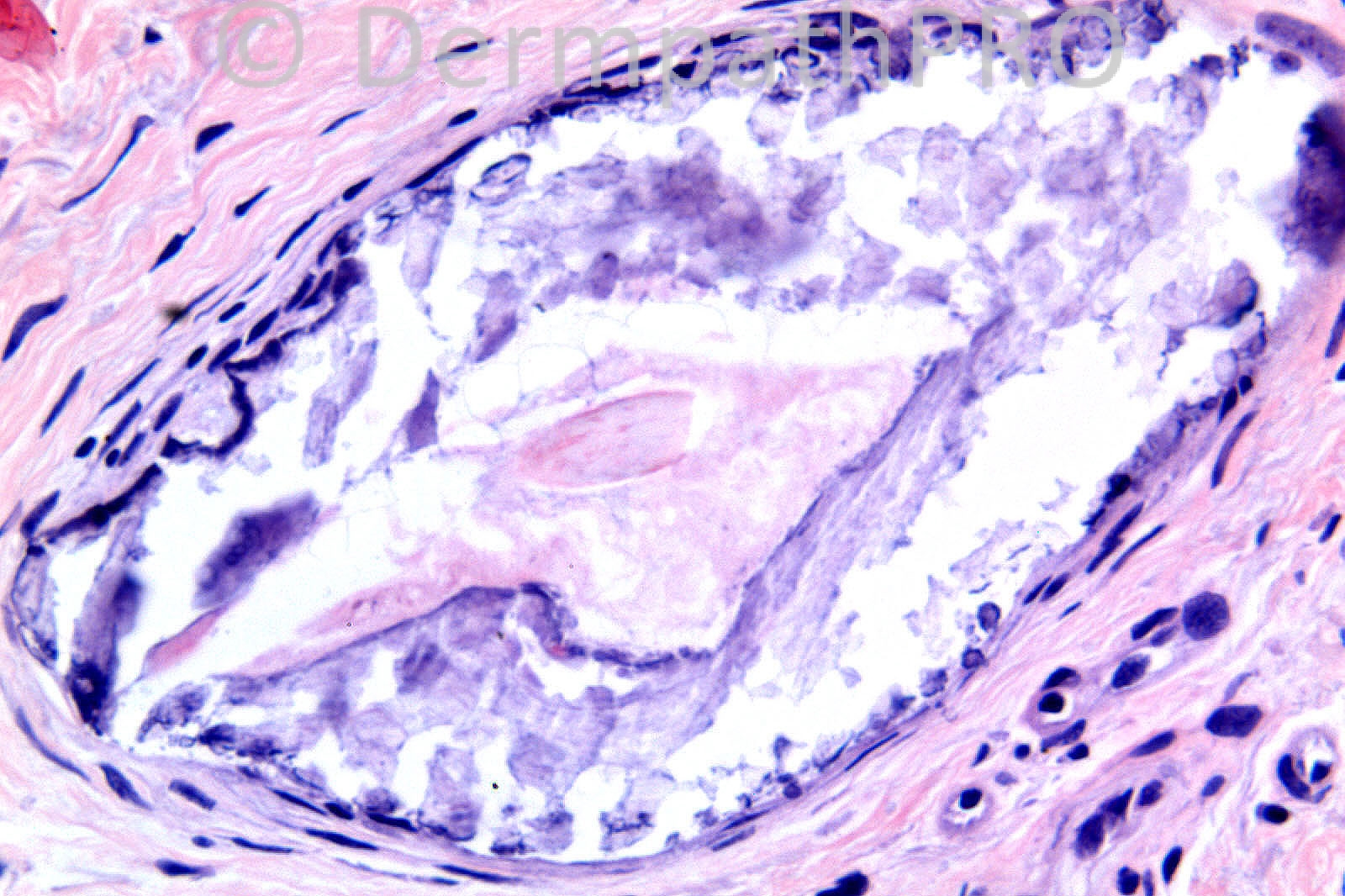
85 year old female with an erythematous scale measuring 10mm on the leg.
Case posted by Dr. Richard Carr.
Case posted by Dr. Richard Carr.

Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.