Case Number : Case 1033 - 9th June Posted By: Guest
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
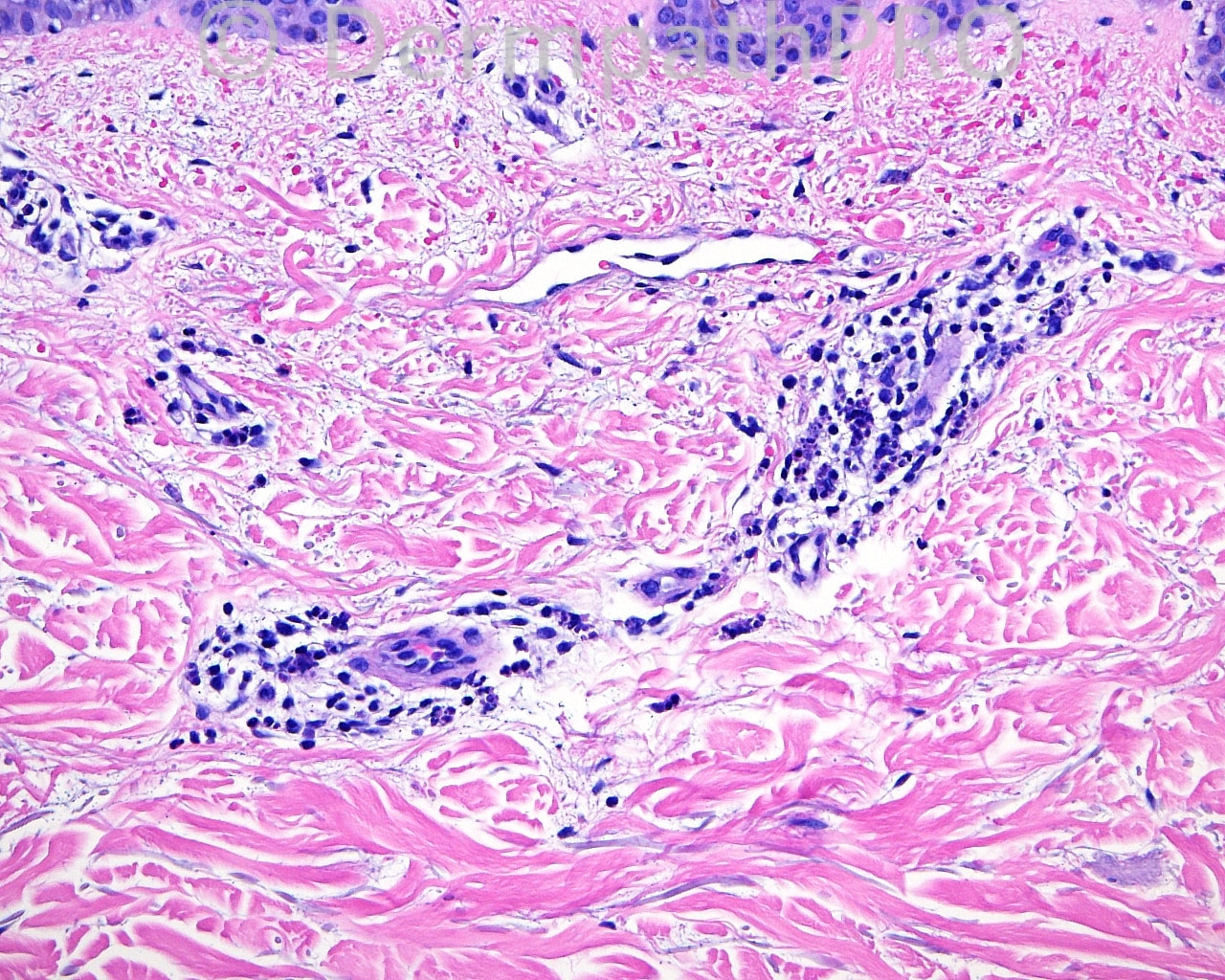
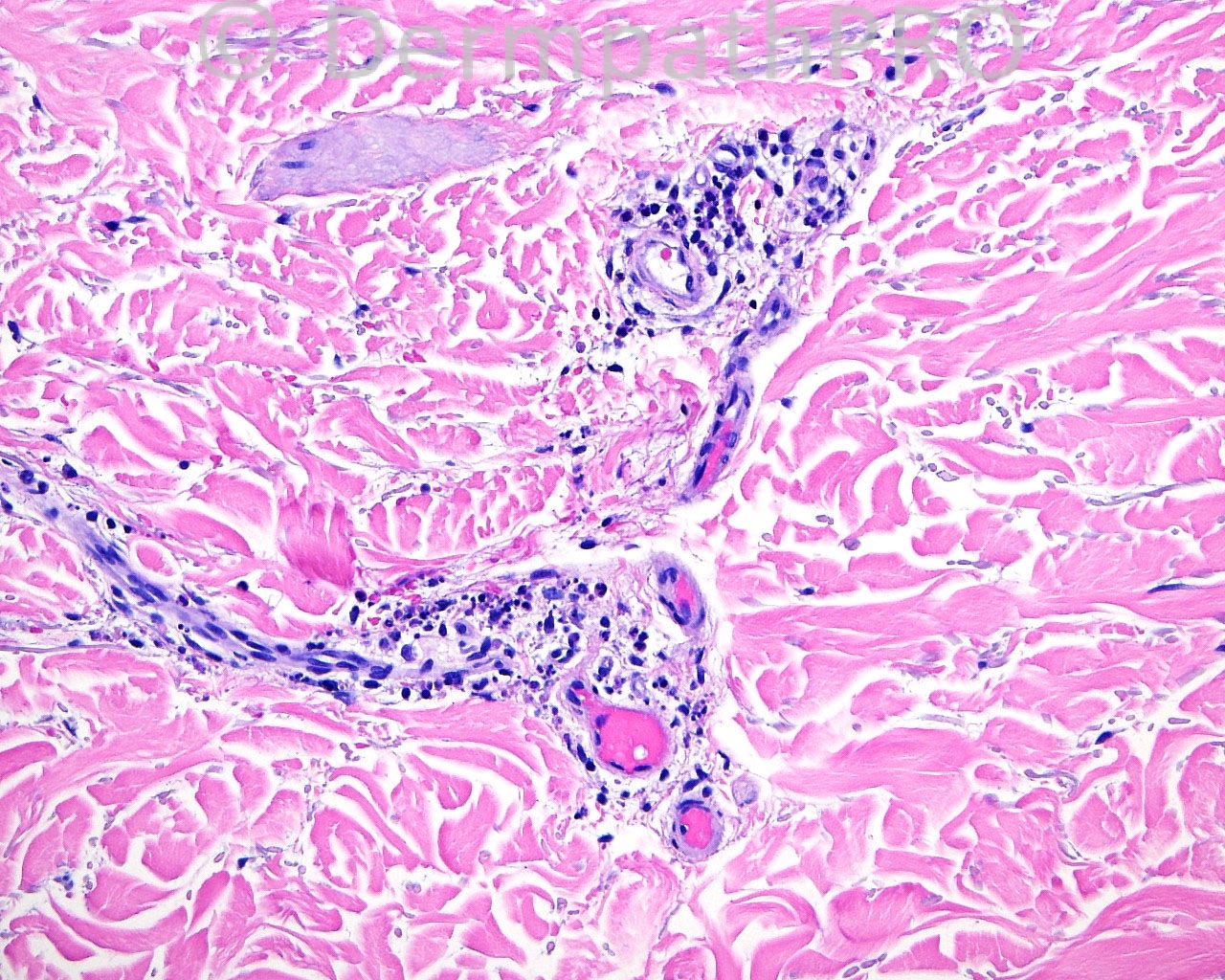
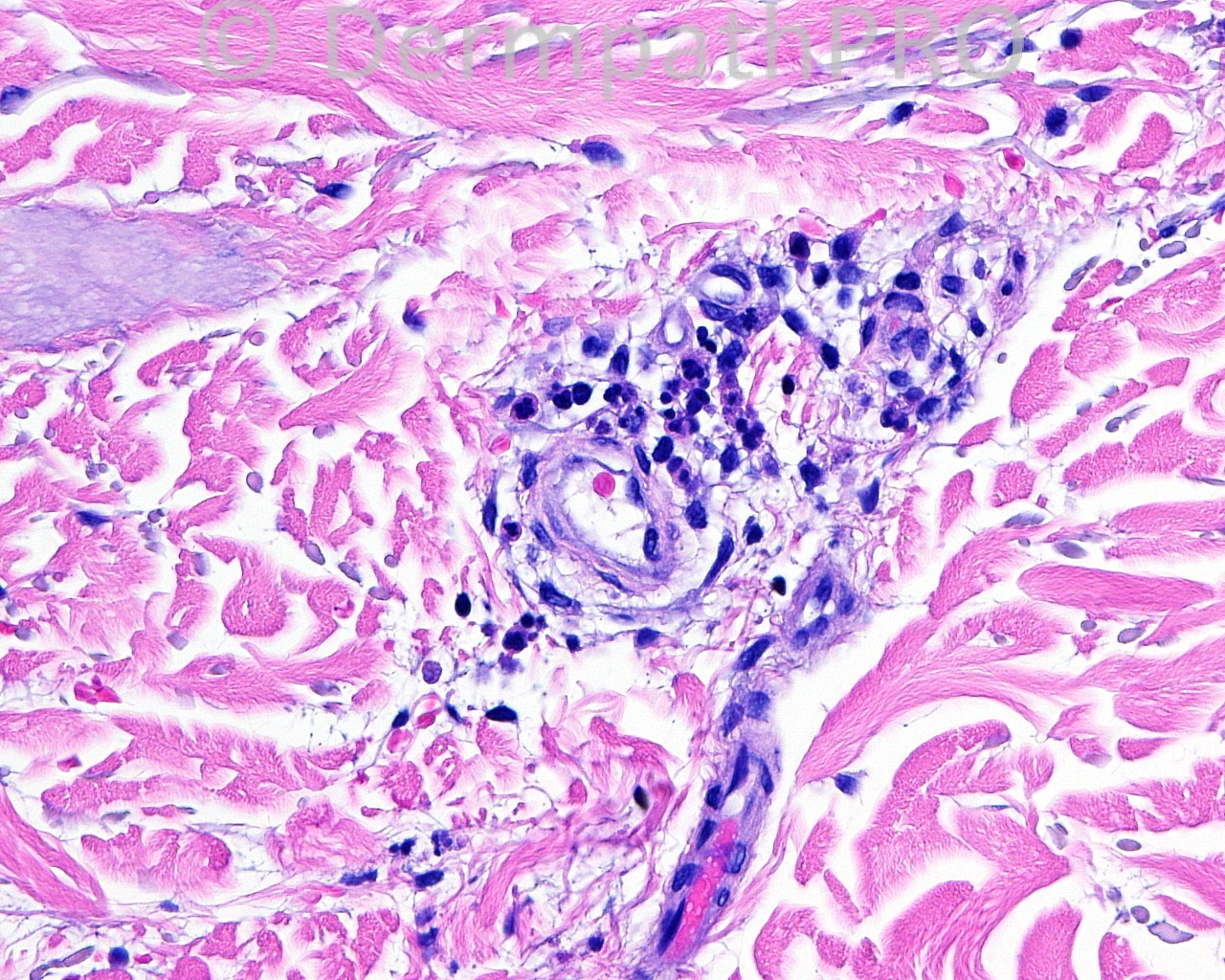
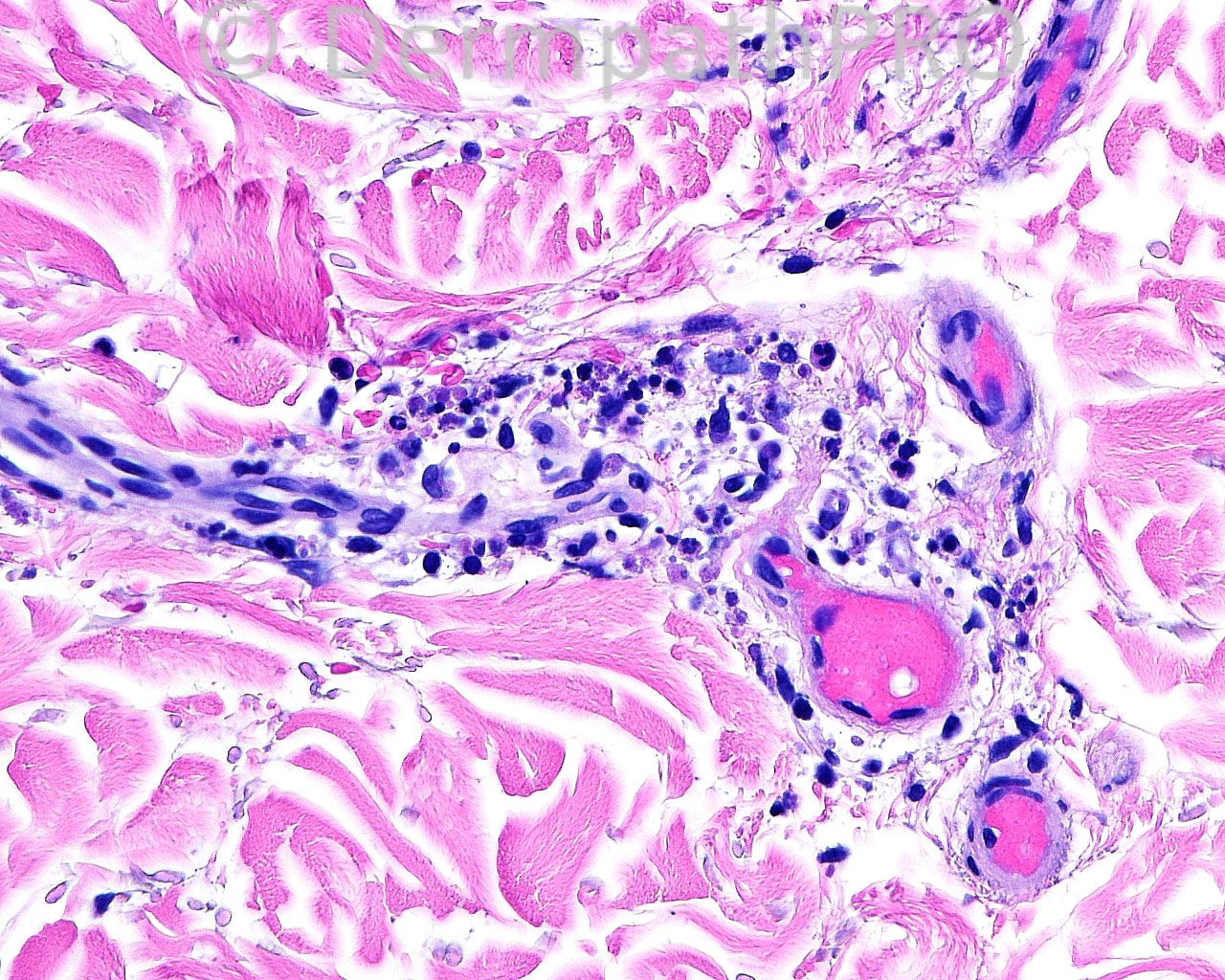
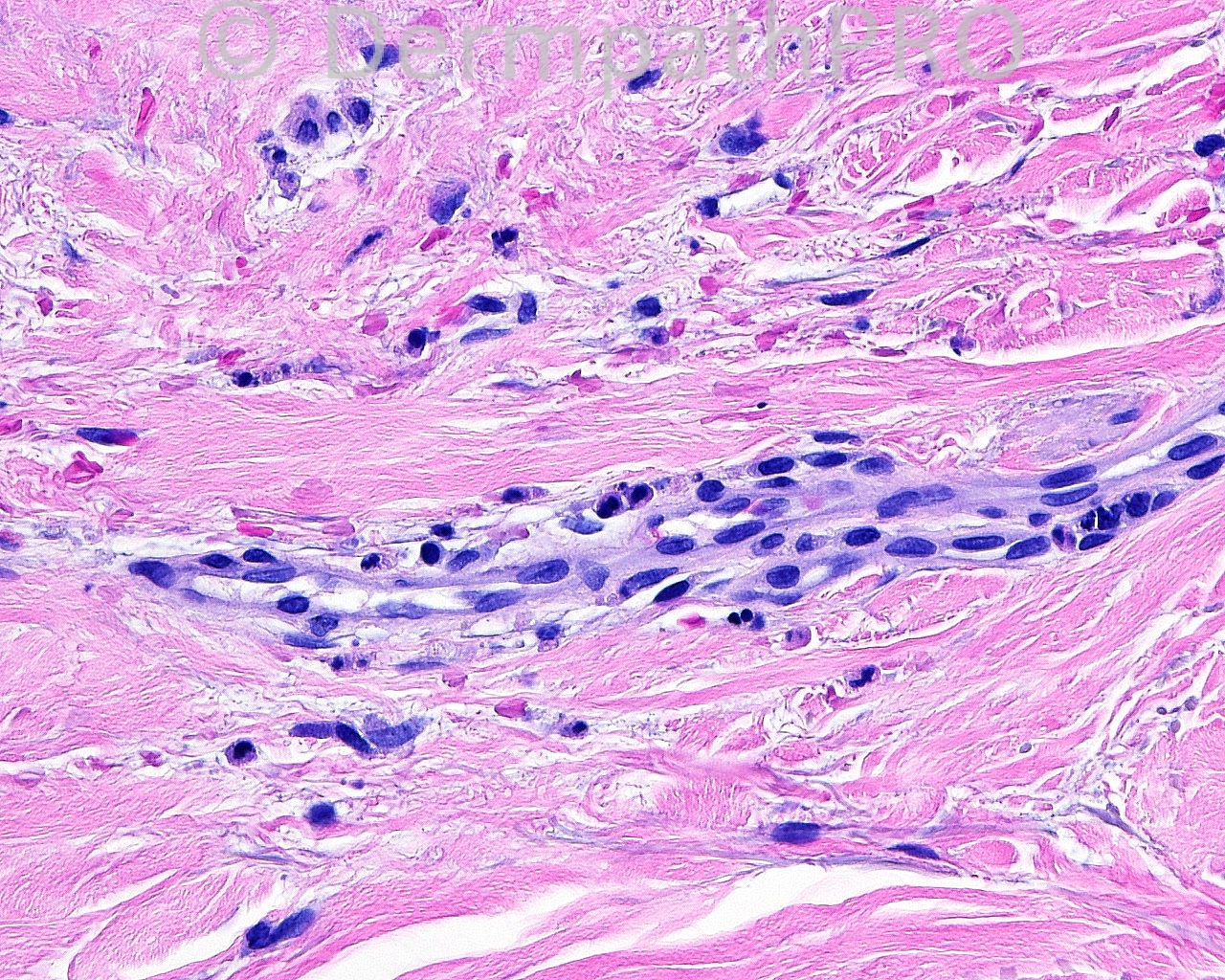
The patient is a 65 year old white man with a biopsy taken from the right ulnar mid volar forearm for direct immunofluorescence.
Case posted by Dr. Mark Hurt.
Case posted by Dr. Mark Hurt.


Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.