Case Number : Case 1247 - 3 April Posted By: Guest
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
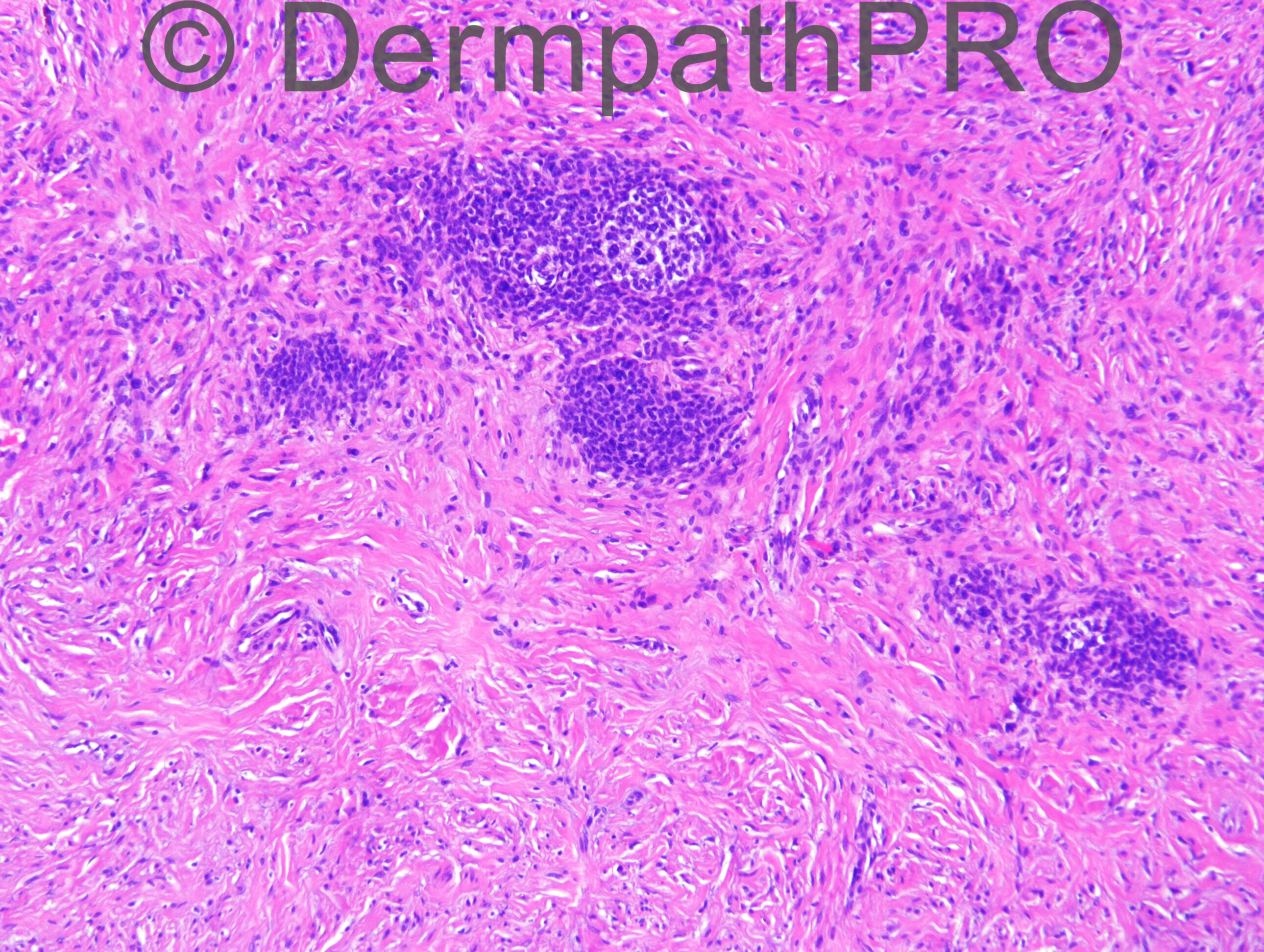
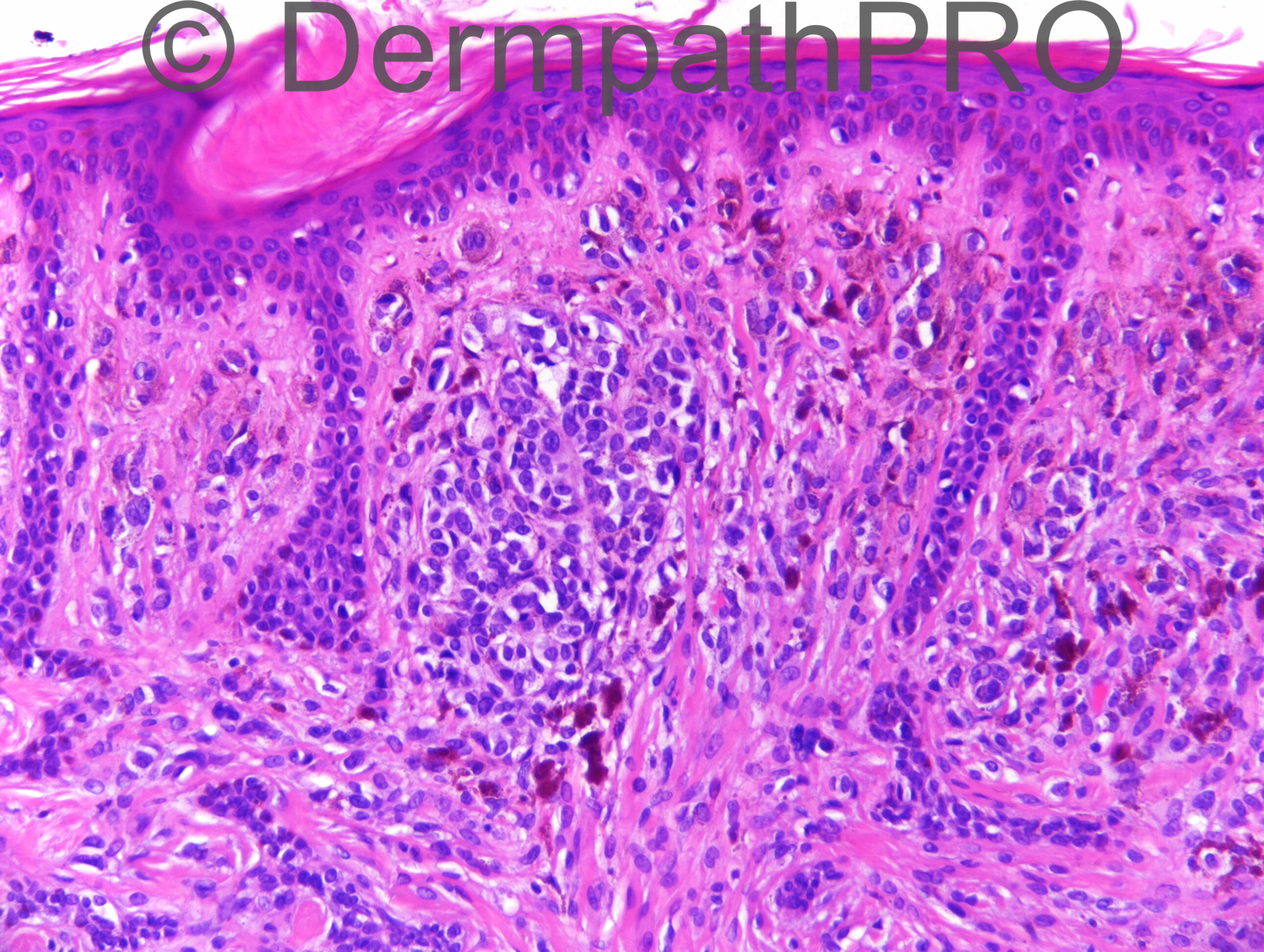
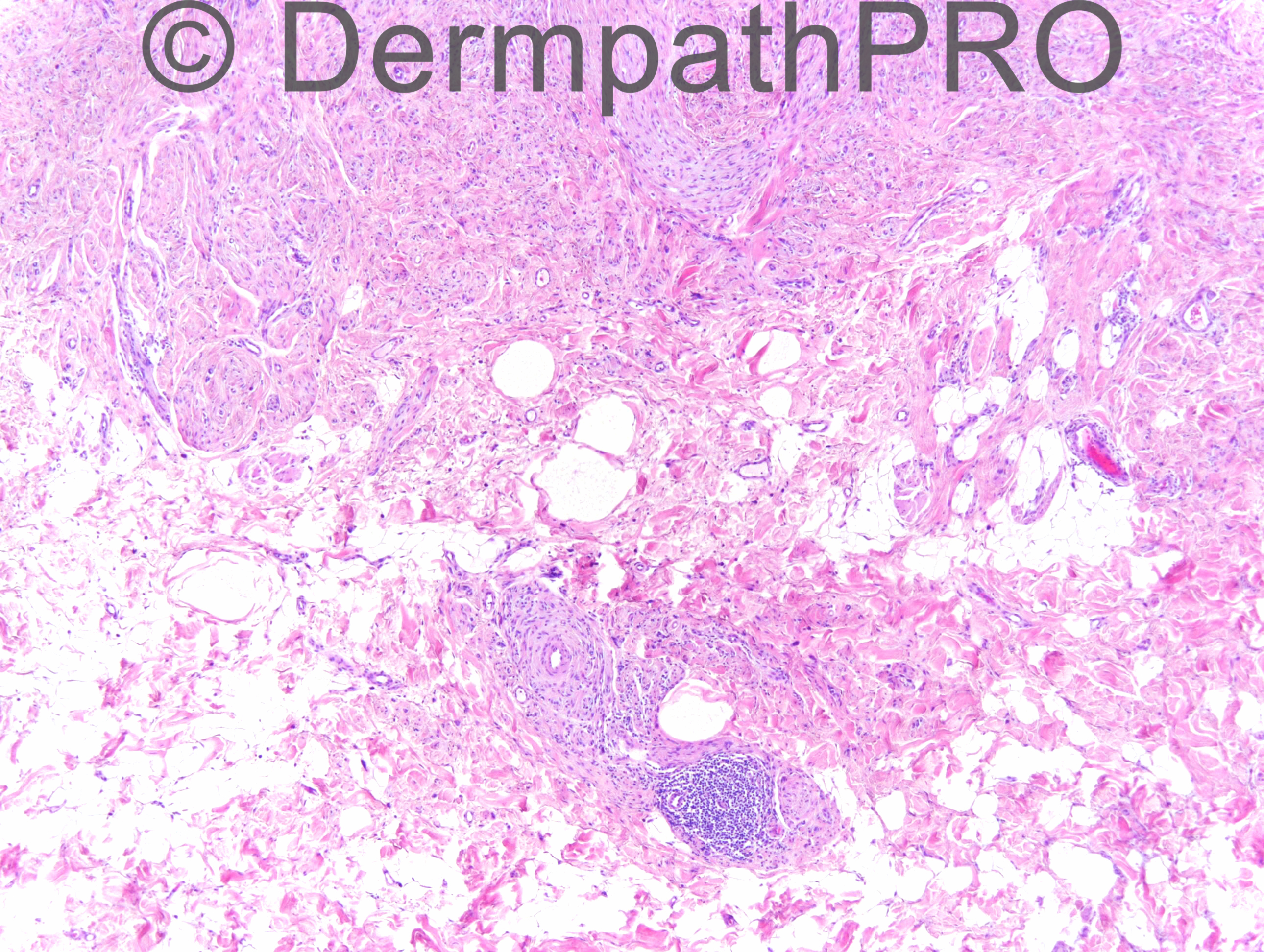
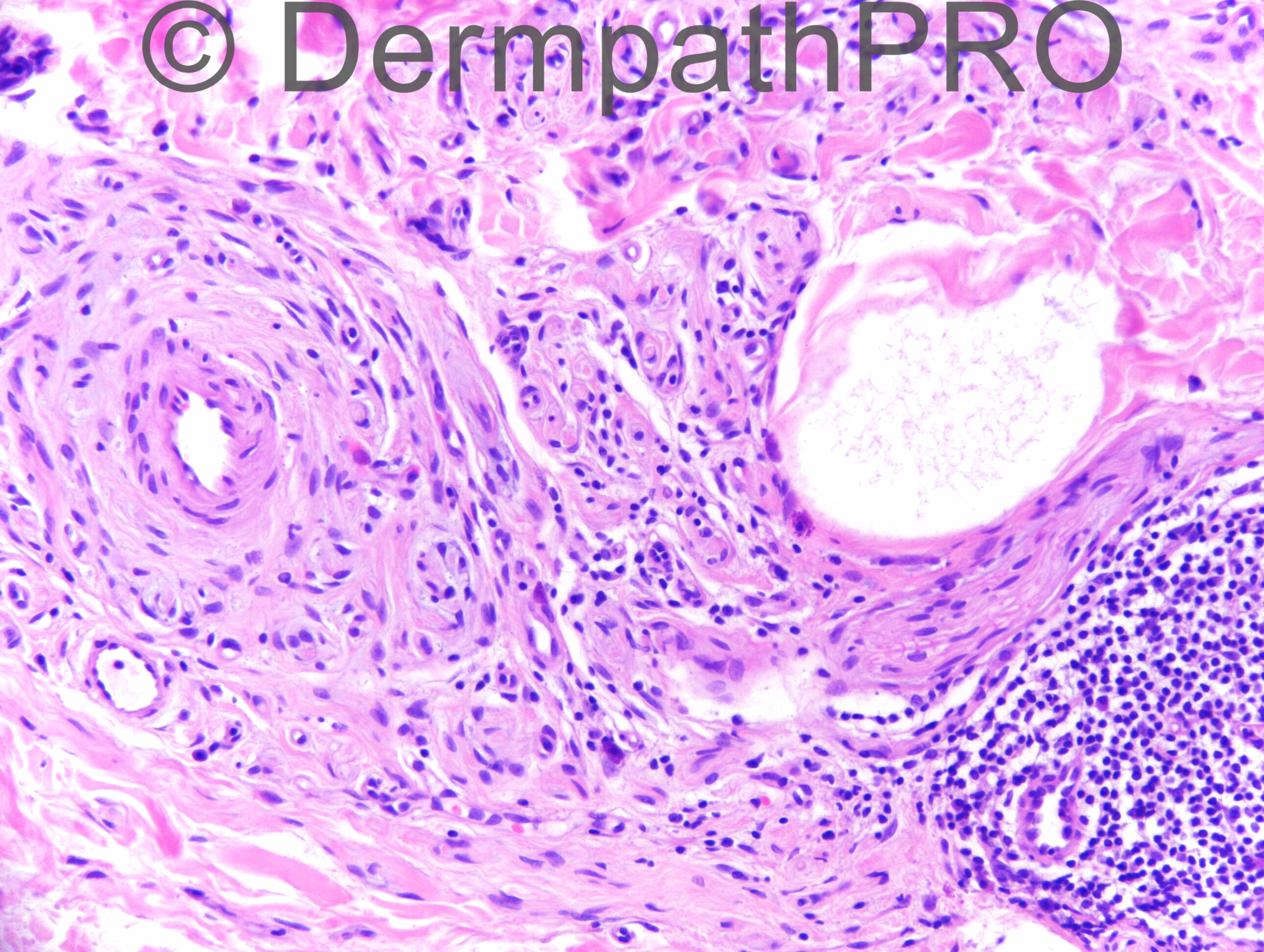
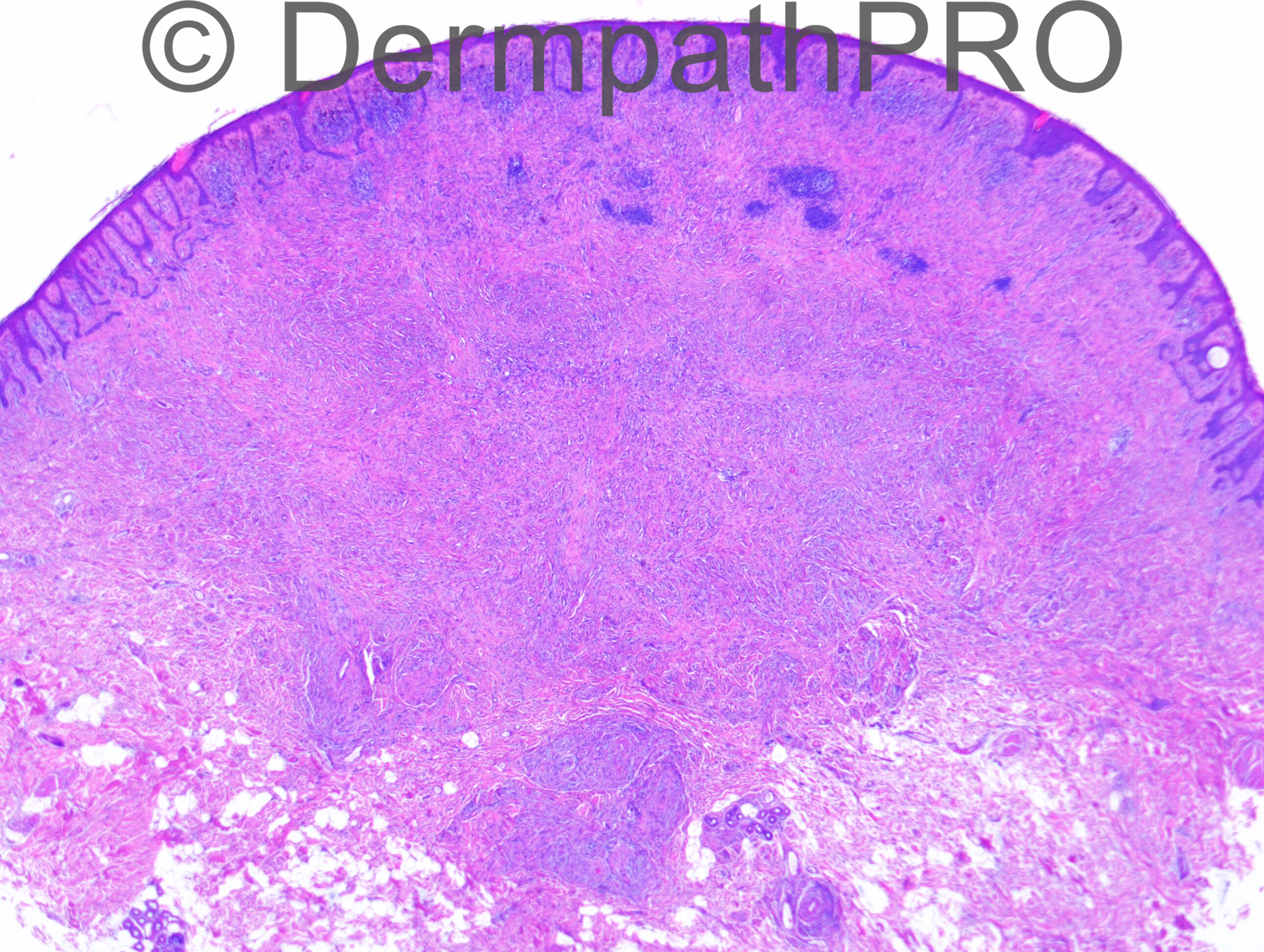
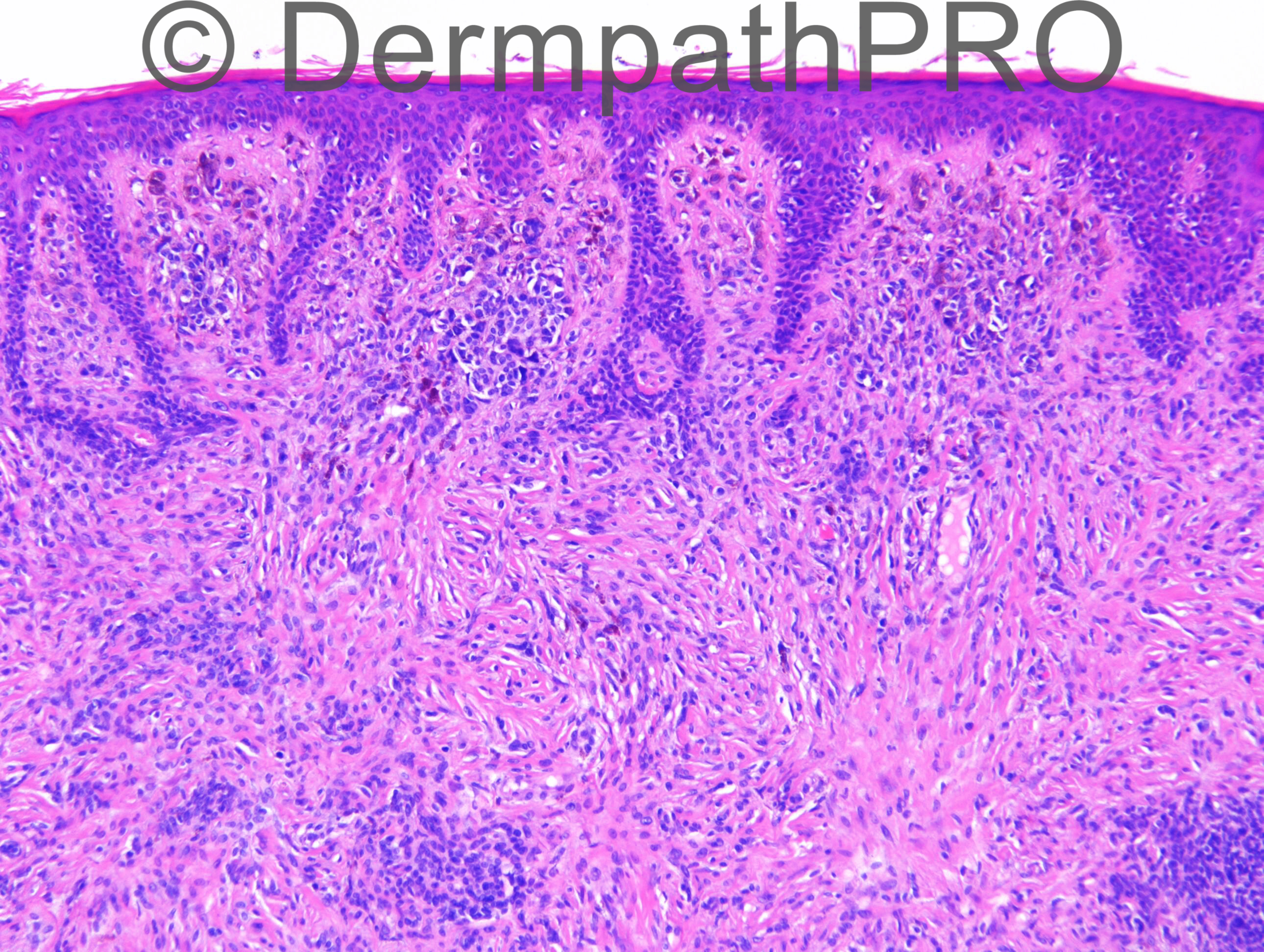
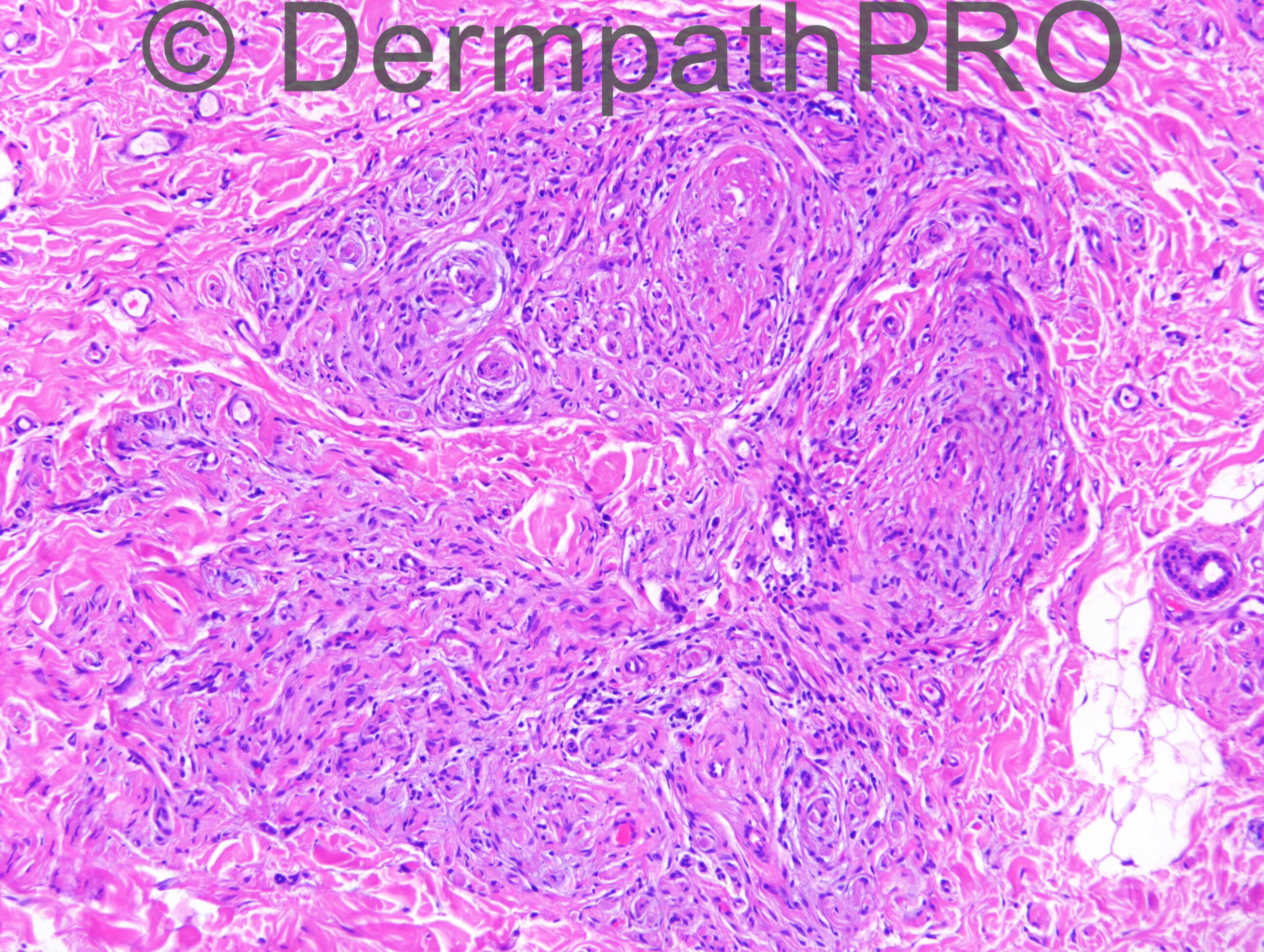
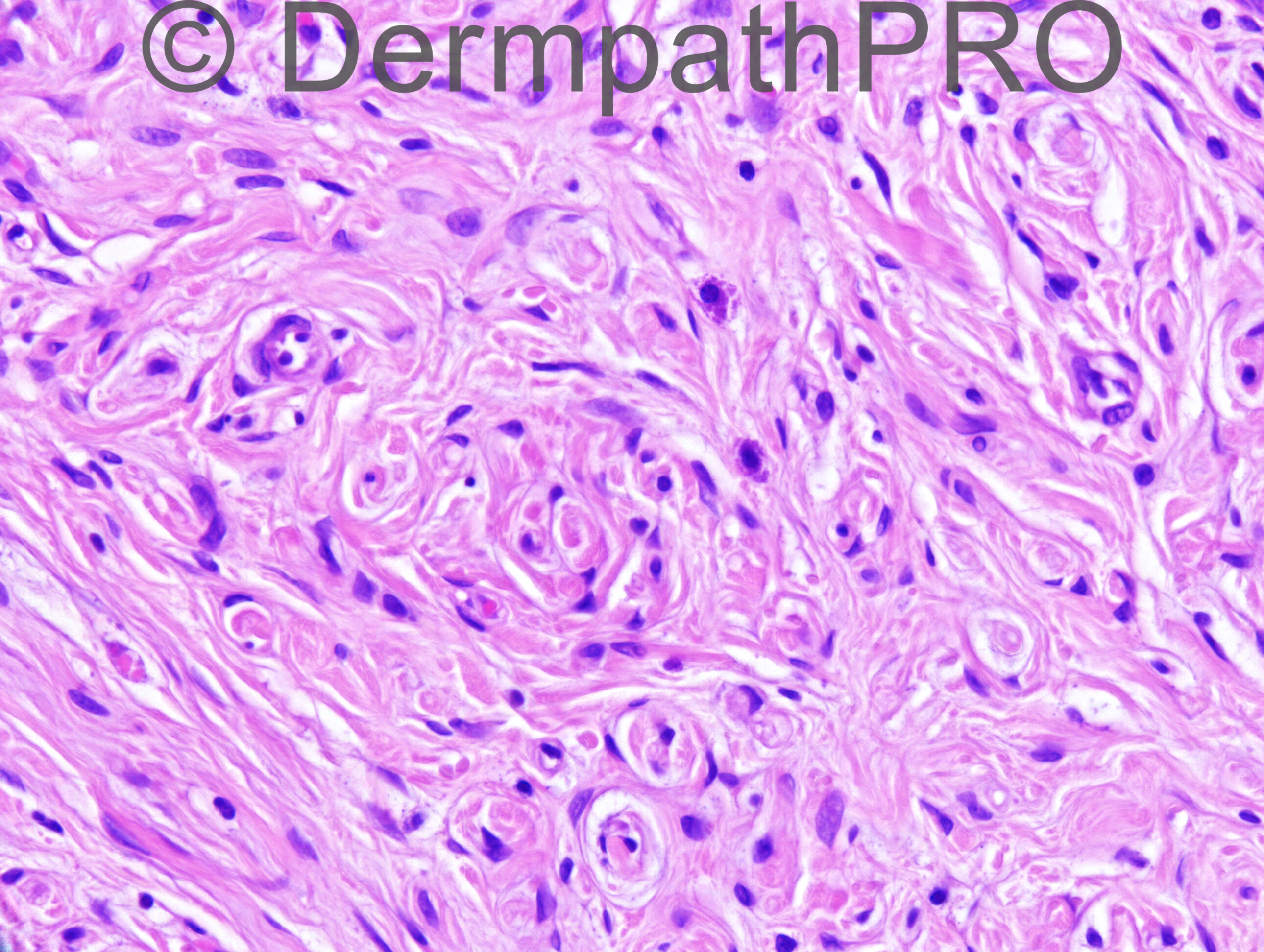
M65. Altered naevus on back.
Case posted by Dr Richard Carr
Case posted by Dr Richard Carr

Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.