Case Number : Case 1414- 24 November Posted By: Guest
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
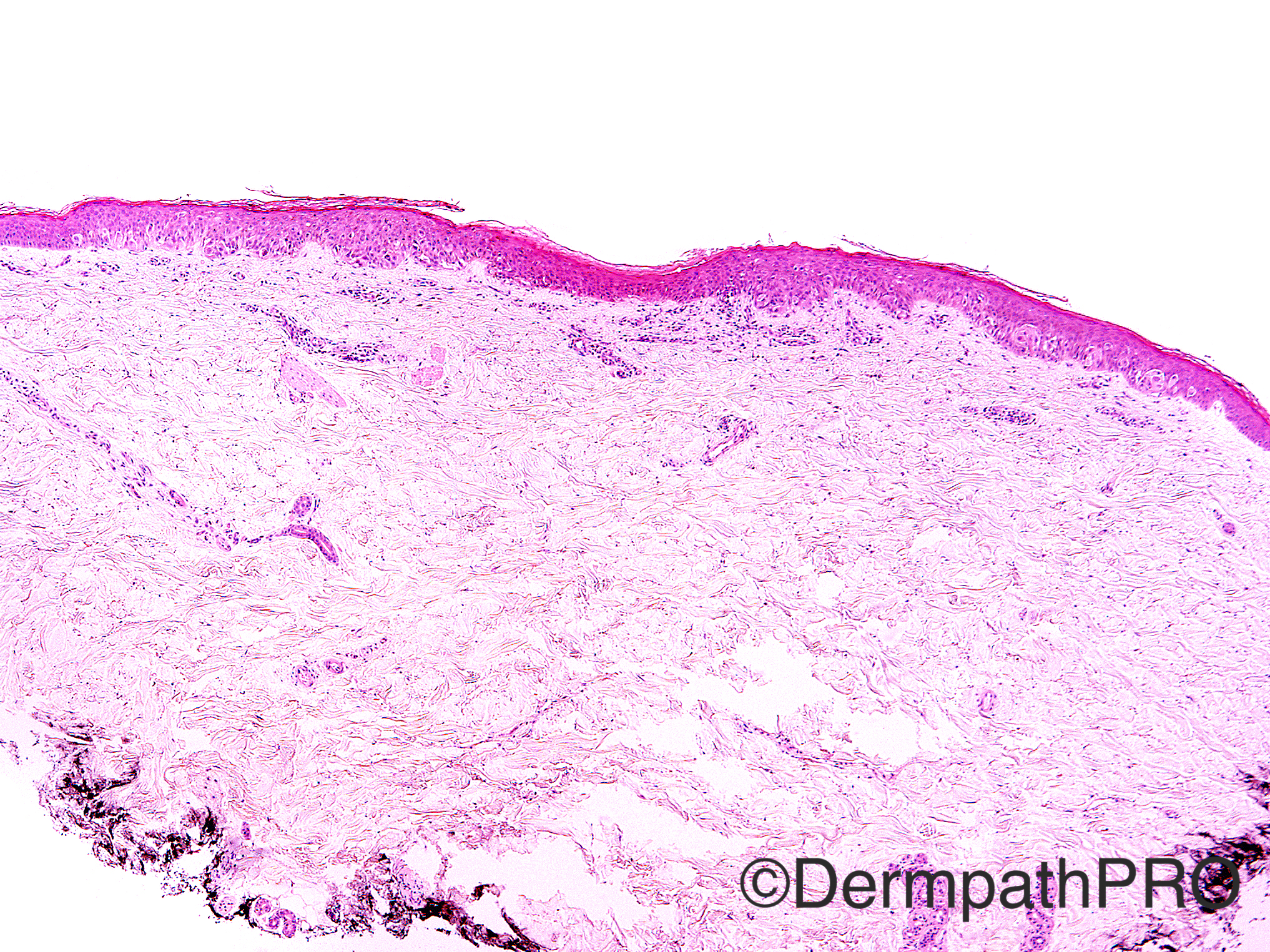
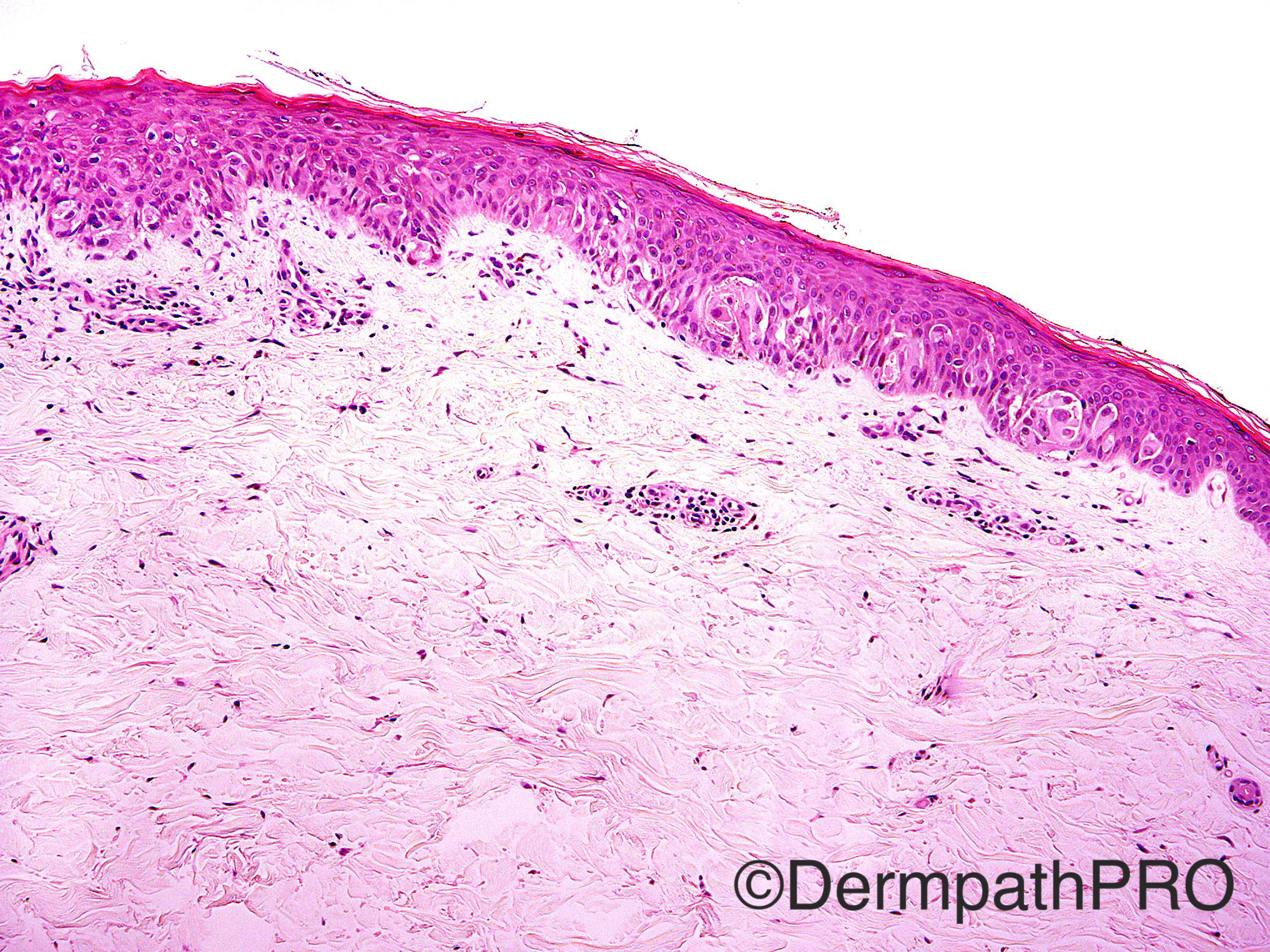
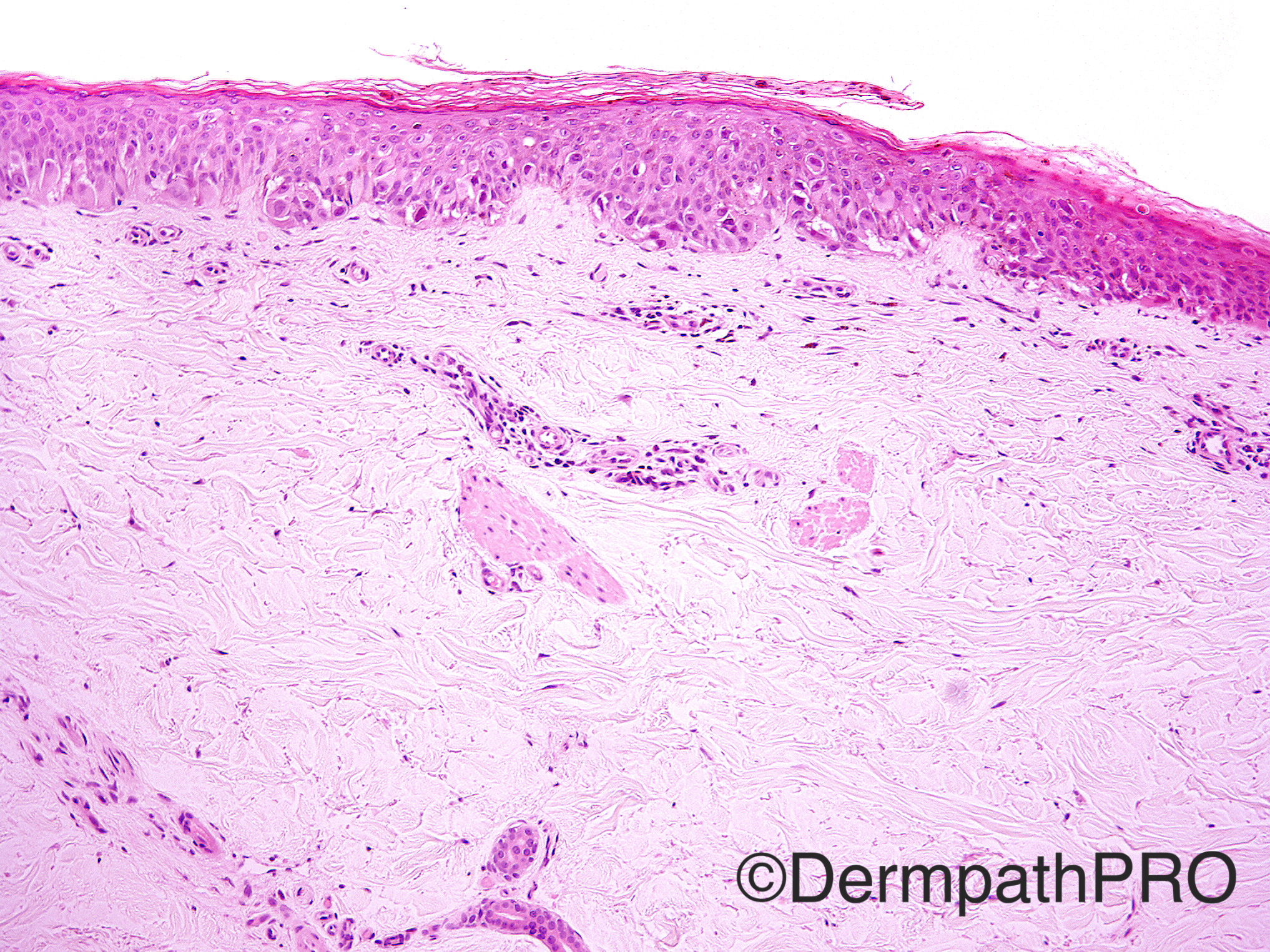
Case History: 29 year old female with nevus on left medial lower leg. Family history of melanoma and multiple atypical nevi. Fifth micrograph-MiTF; Sixth micrograph-p16.
Case posted by Dr Uma Sundram
Case posted by Dr Uma Sundram




Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.