Case Number : Case 1524 - 27 April Posted By: Guest
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
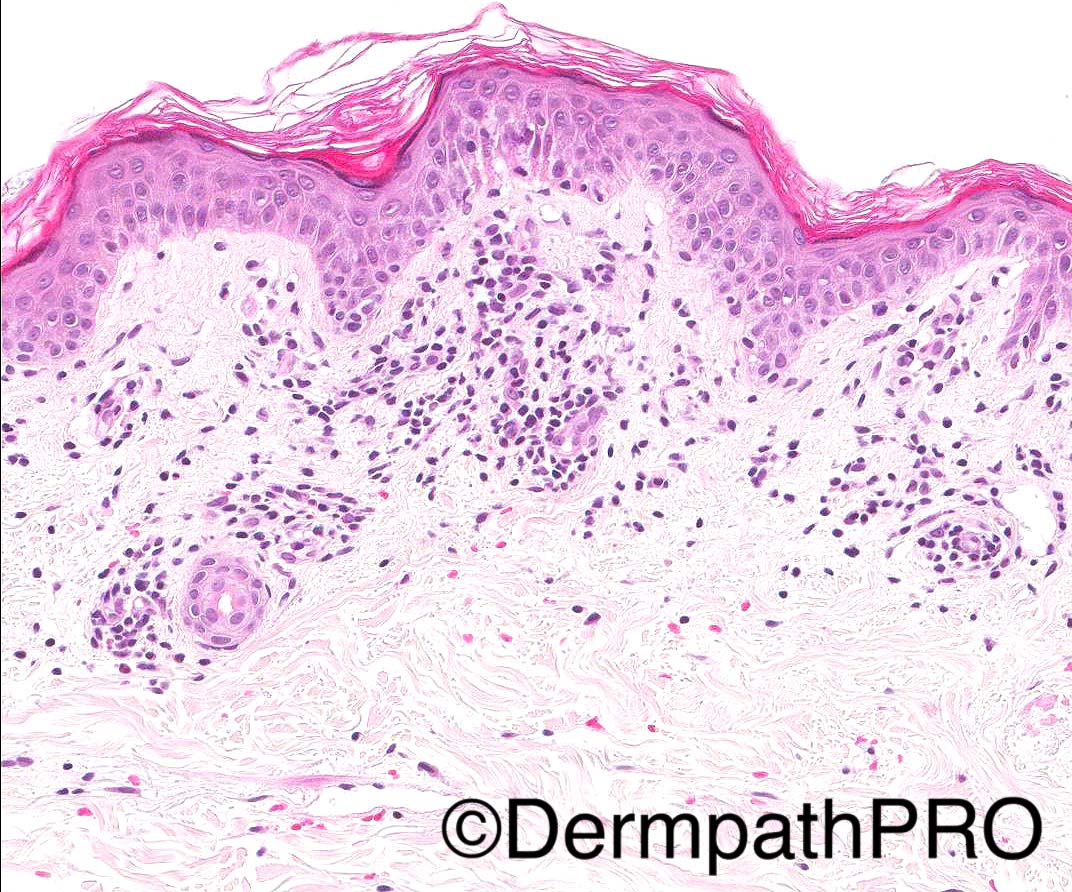
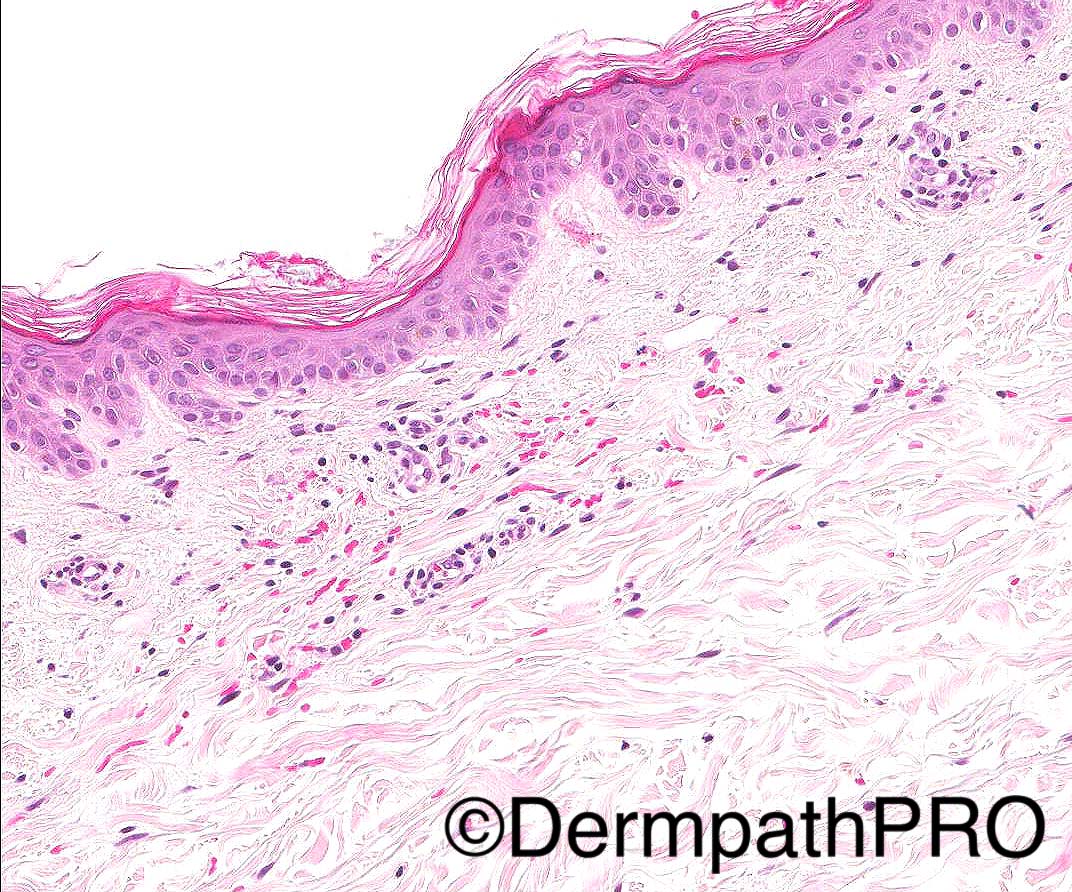
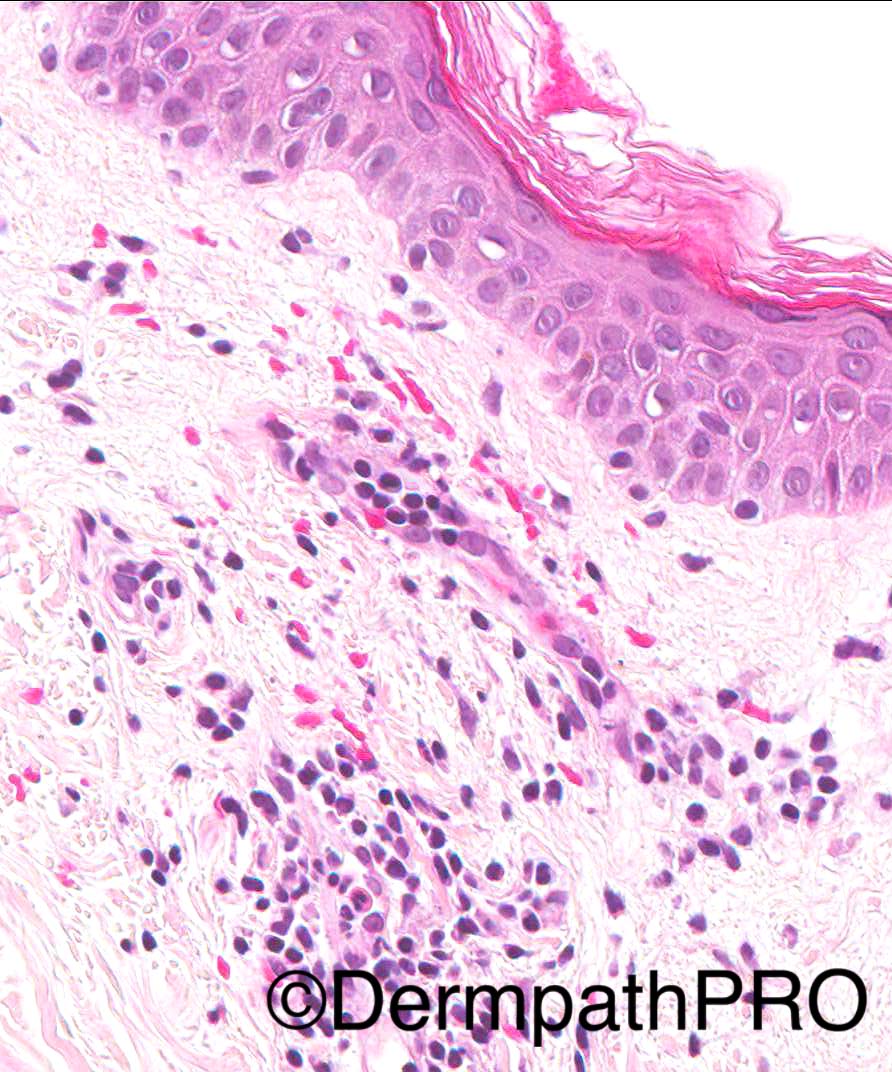
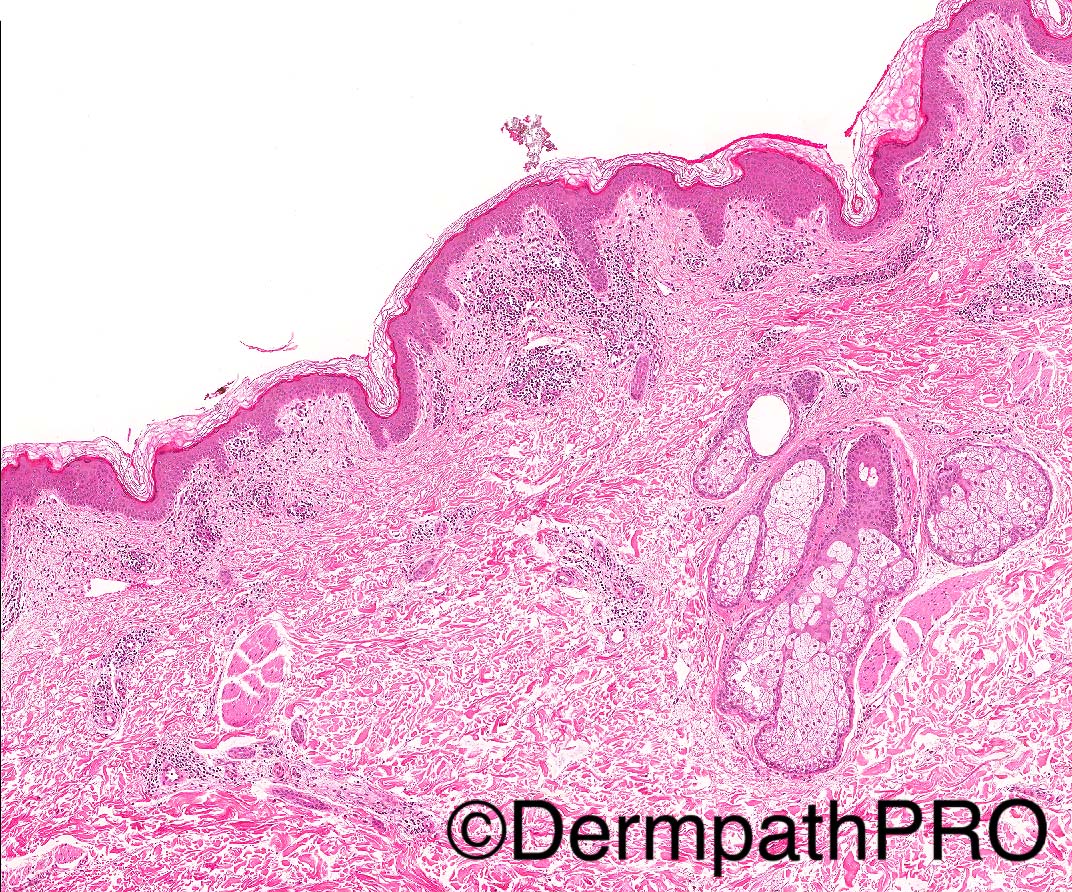
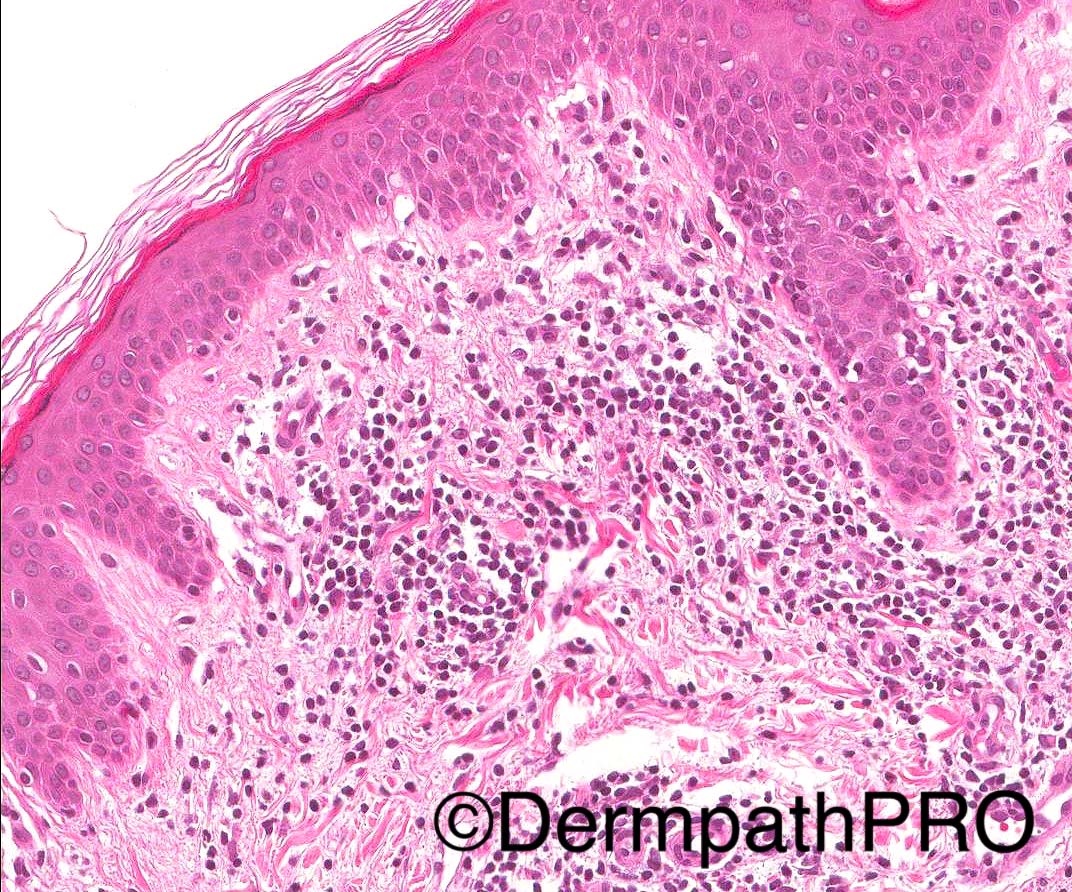
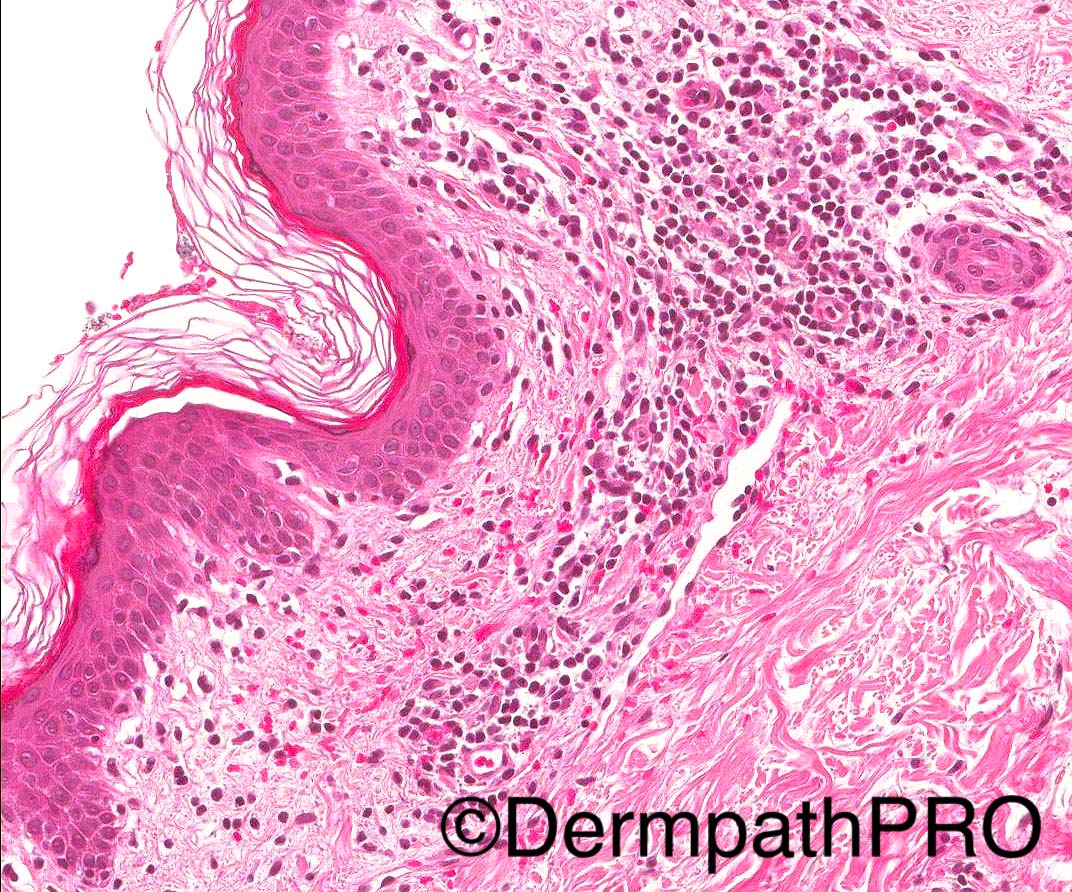
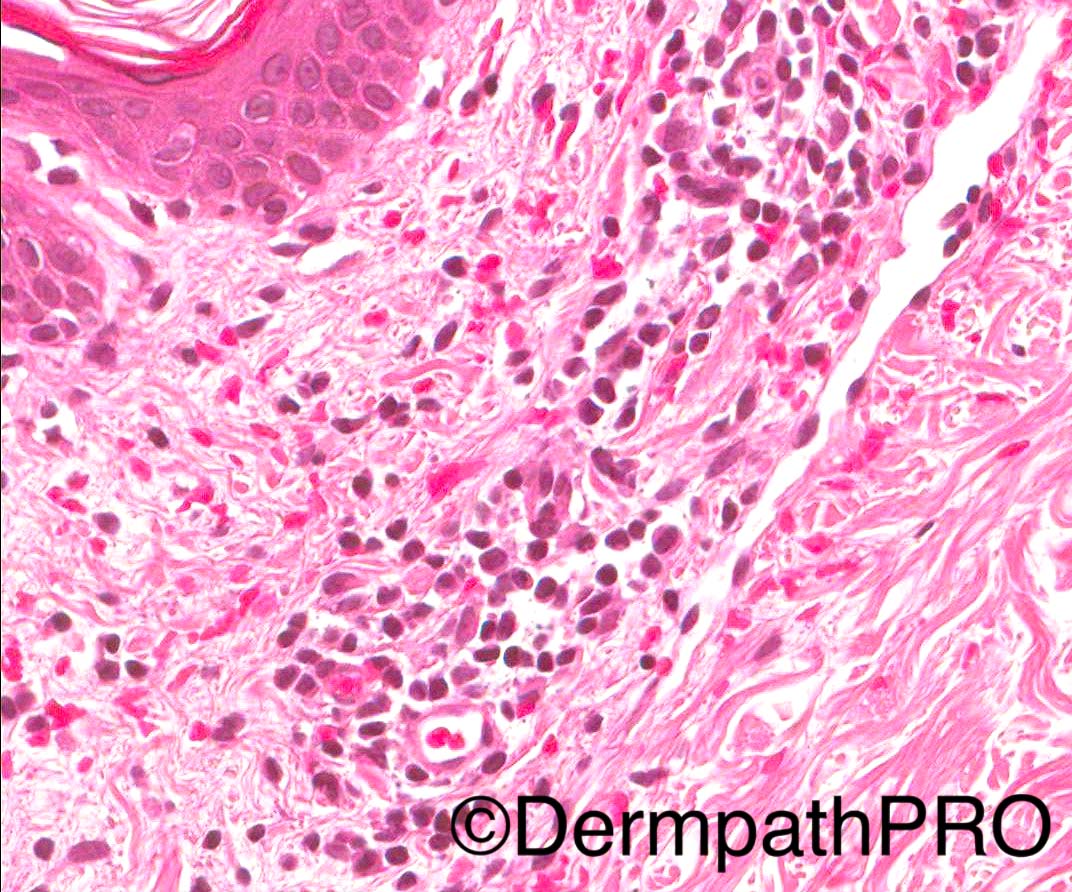
60/M with a symmetrical erythematous rash in groins, upper thigh and axilla (started nearly 20 years ago). Flares up every 6-12 months, sore and occasionally itchy. Clinical d/d- ?erythrasma, ?eczema.
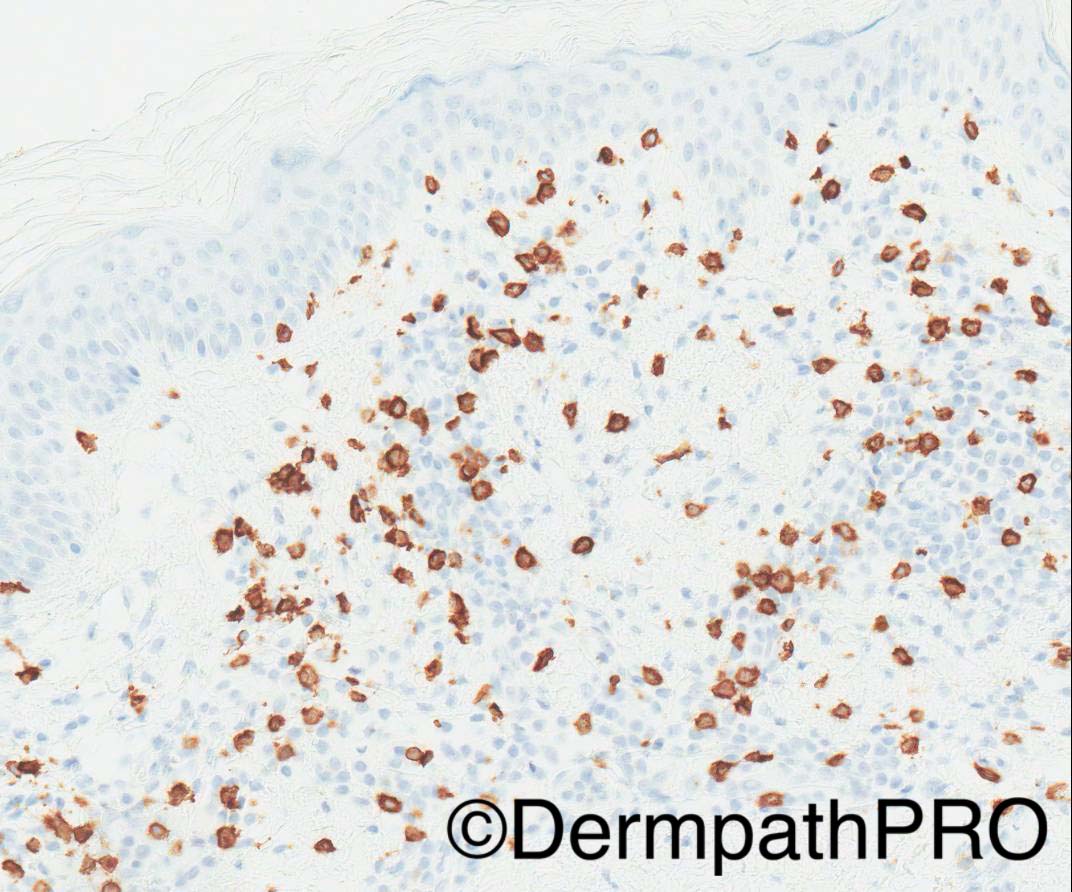
2 biopsies, 1st punch bx , from axilla, done in 2013 (images 1-4) and 2nd incisional bx from thigh, 2014 (images 5-10). Image 9- CD4, image 10- CD8
Case posted by Dr Arti Bakshi
2 biopsies, 1st punch bx , from axilla, done in 2013 (images 1-4) and 2nd incisional bx from thigh, 2014 (images 5-10). Image 9- CD4, image 10- CD8
Case posted by Dr Arti Bakshi



Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.