Case Number : Case 1946 - 14 Nov Posted By: Uma Sundram
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
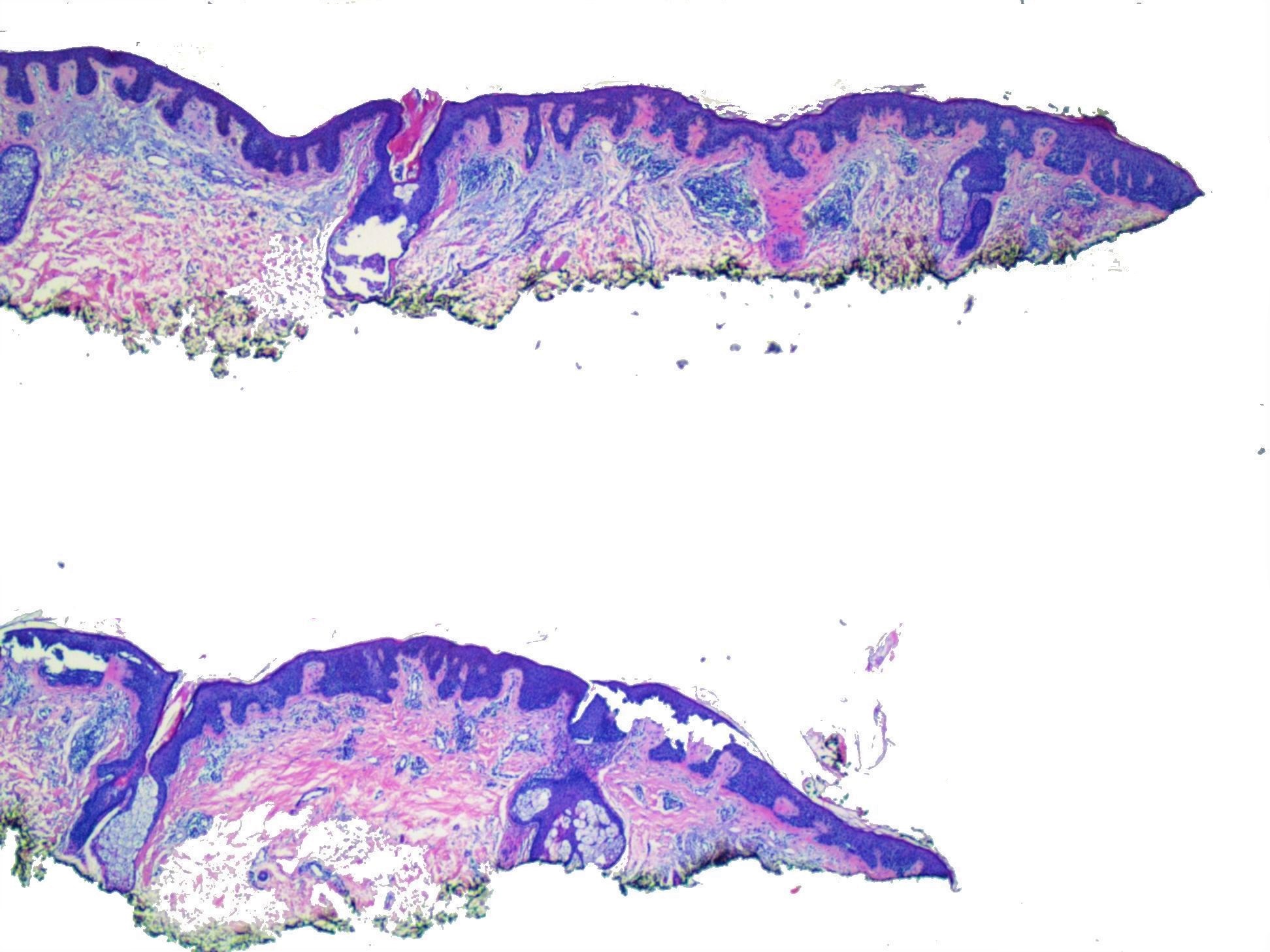
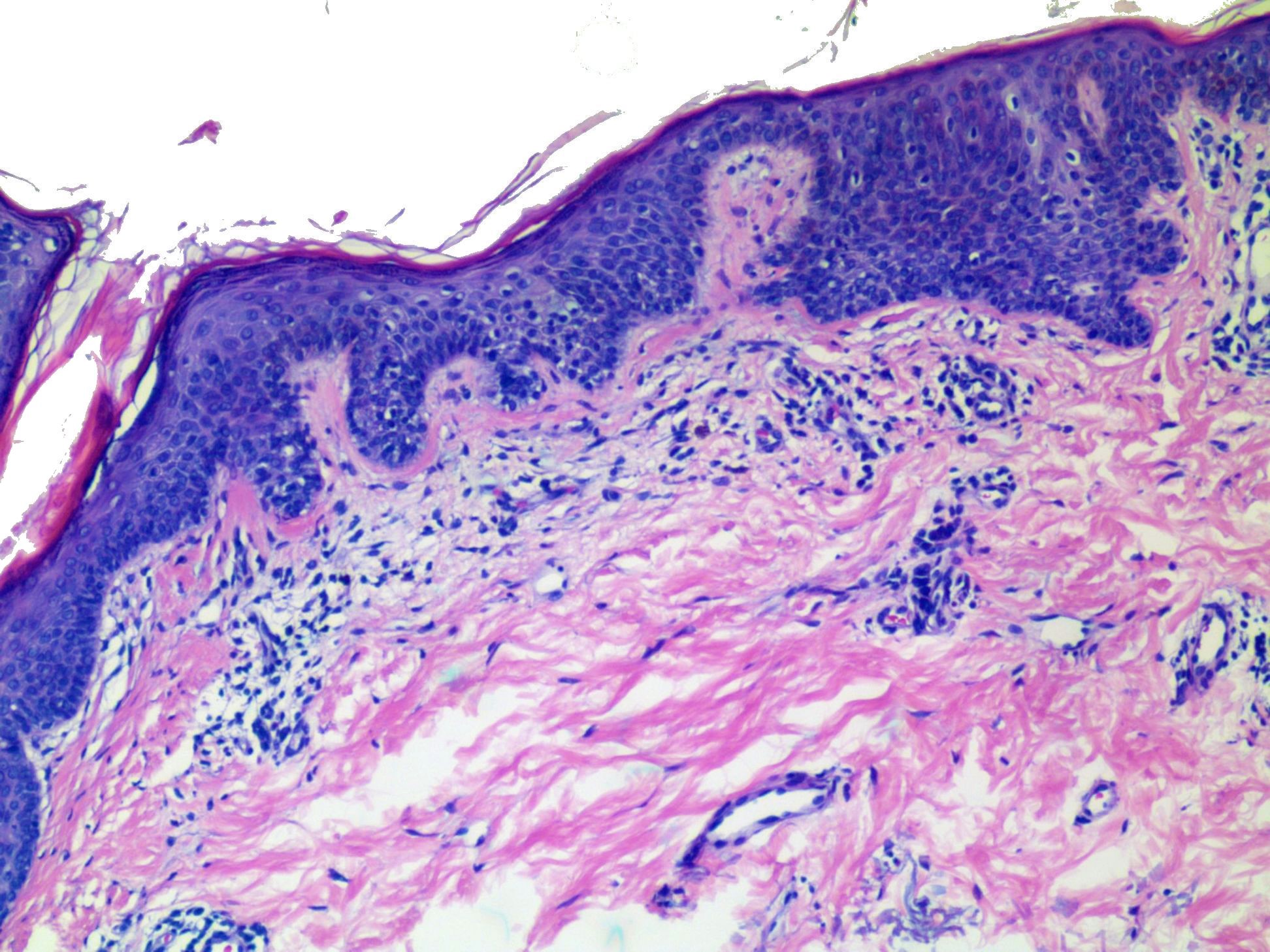
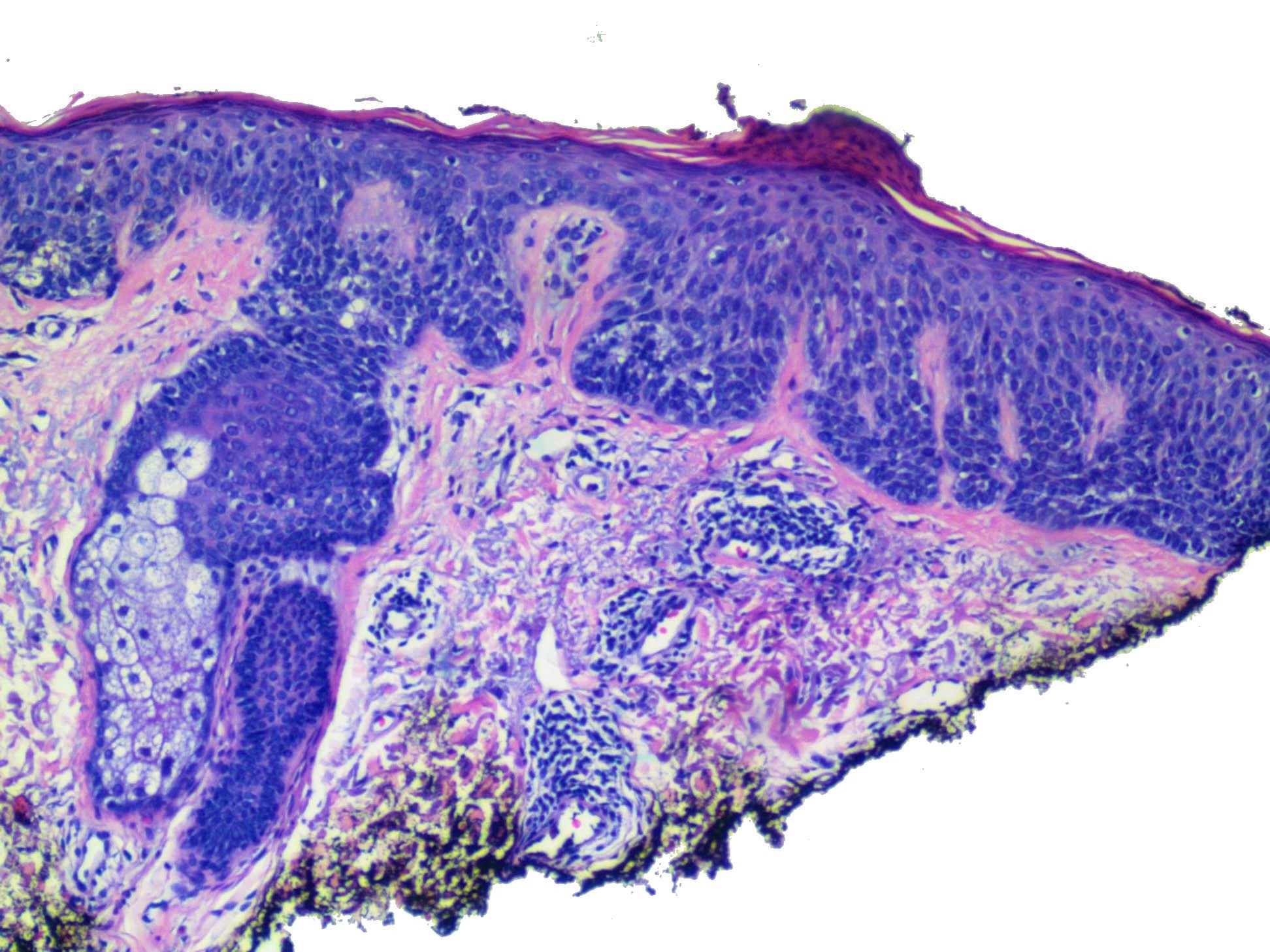
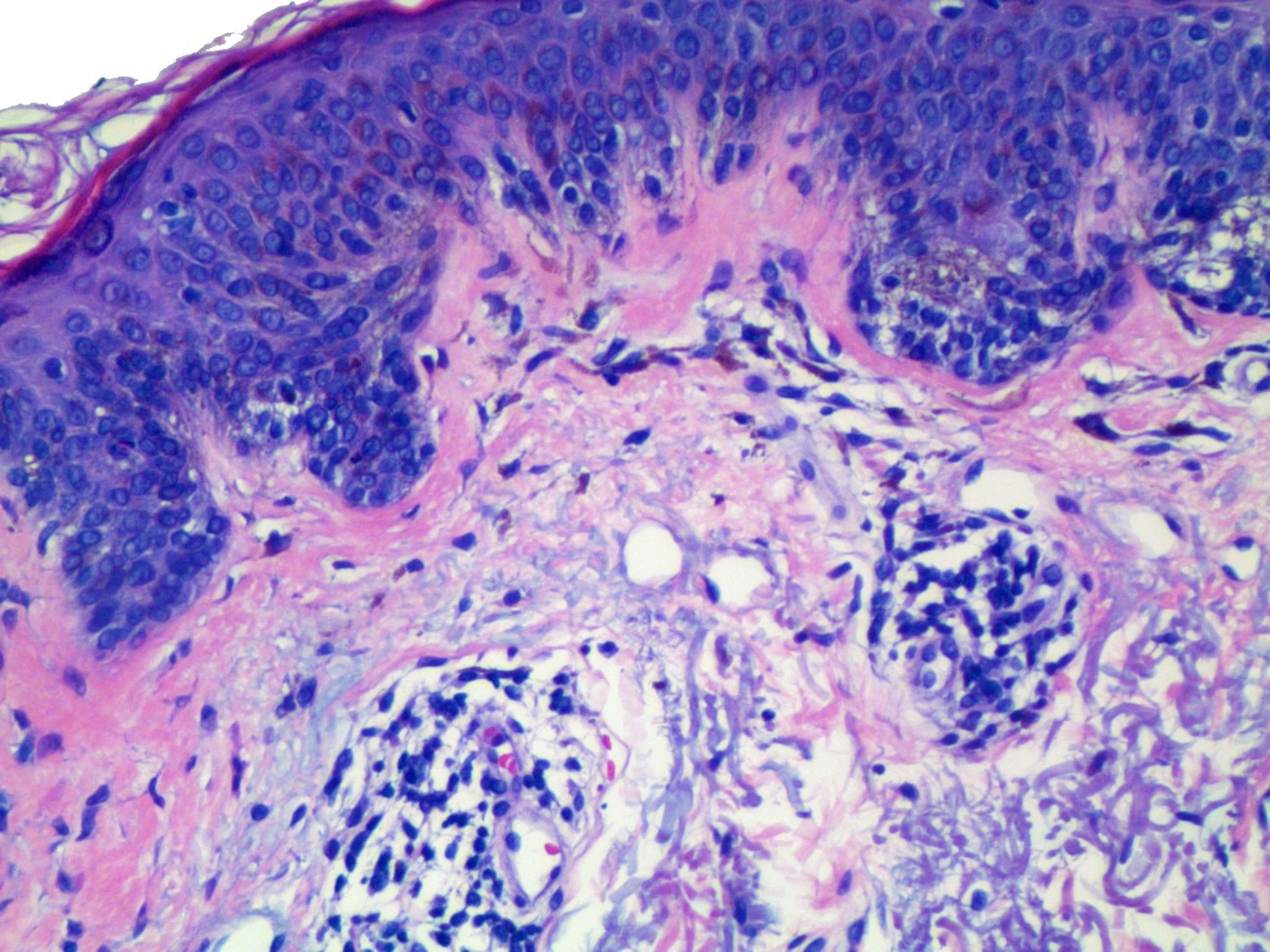
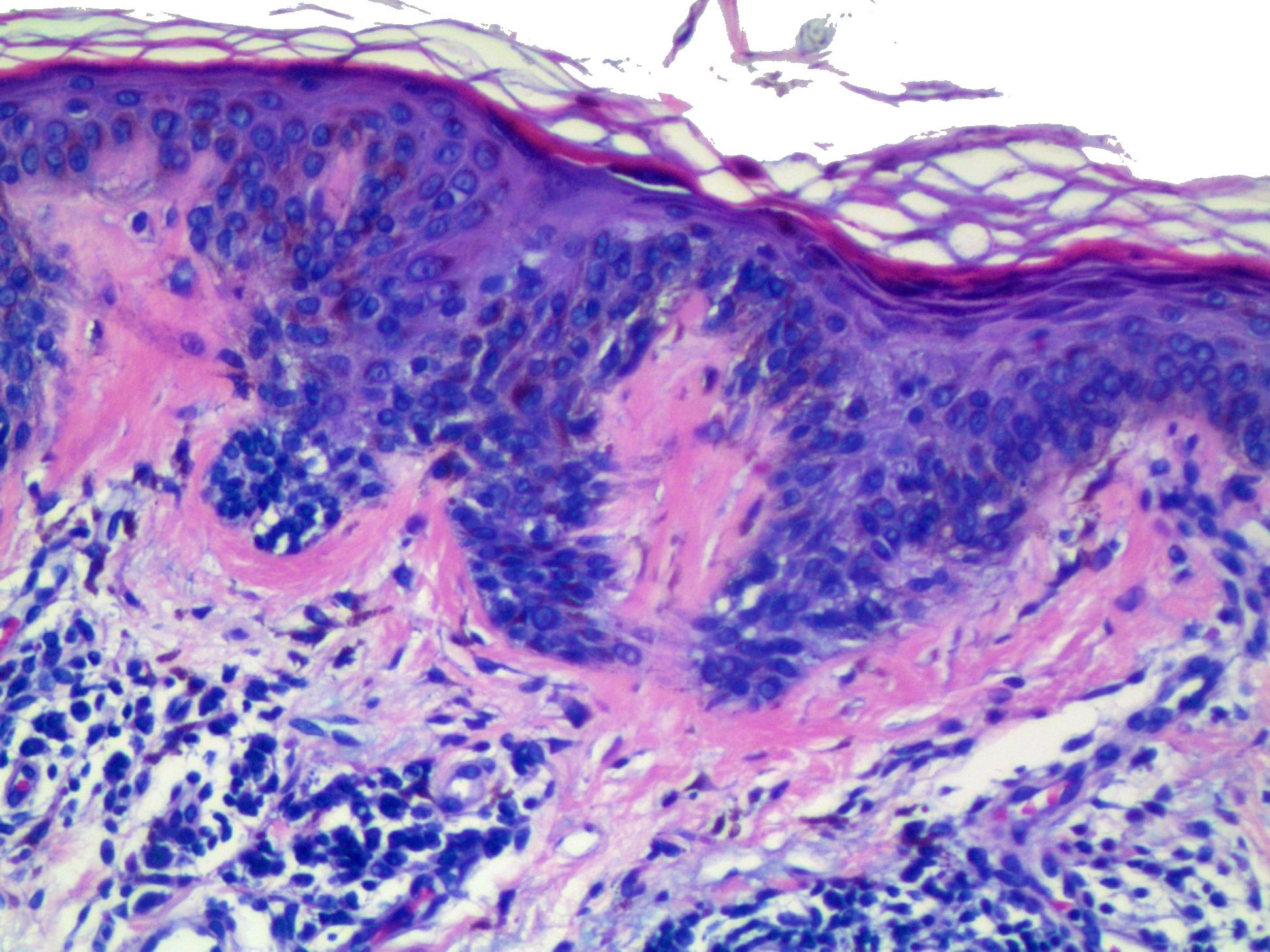
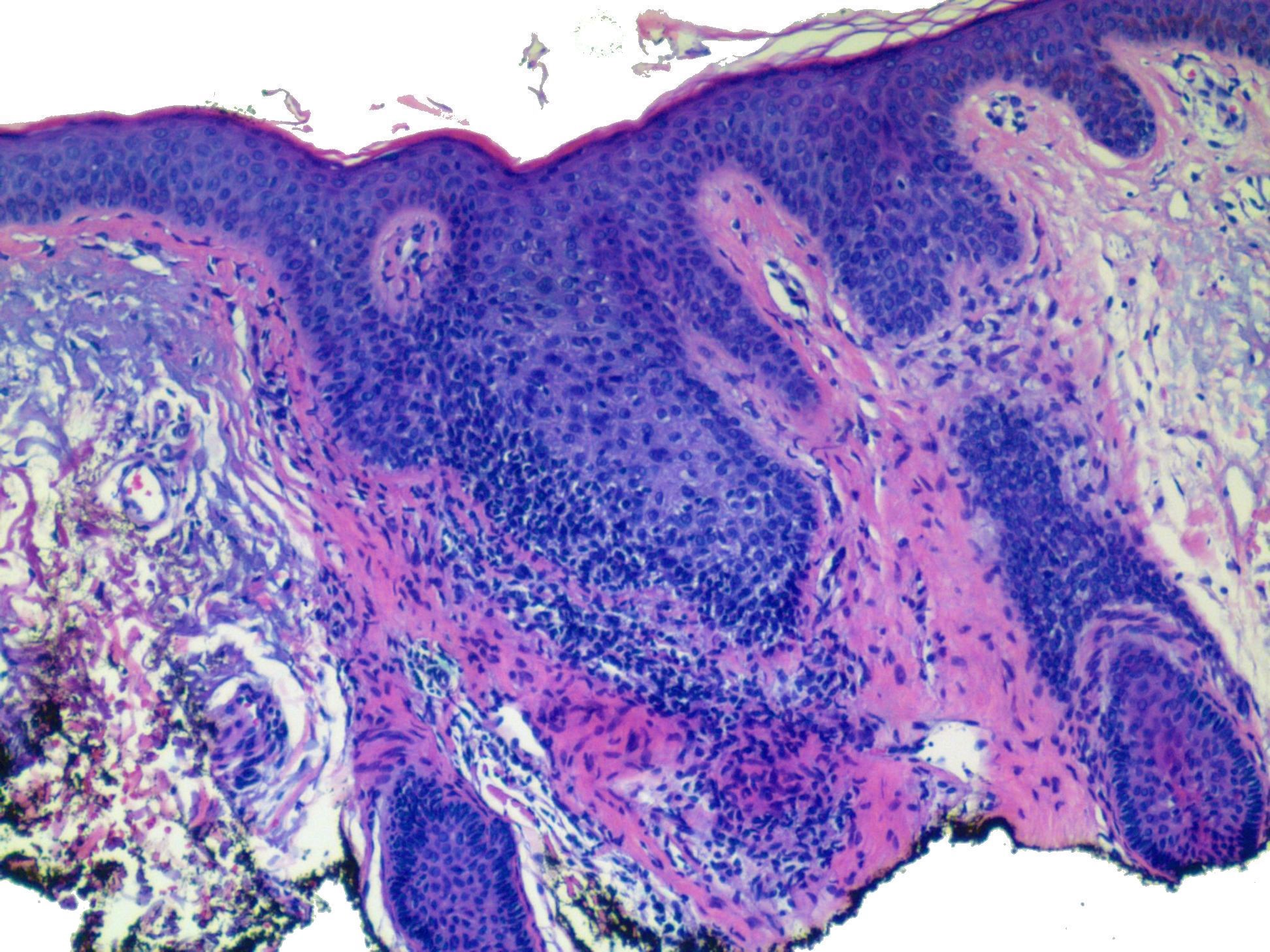
55 year old man with pigmented lesion on the left arm. What are your treatment recommendations?

Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.