Case Number : Case 2212 - 30 November 2018 Posted By: Dr. Richard Carr
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
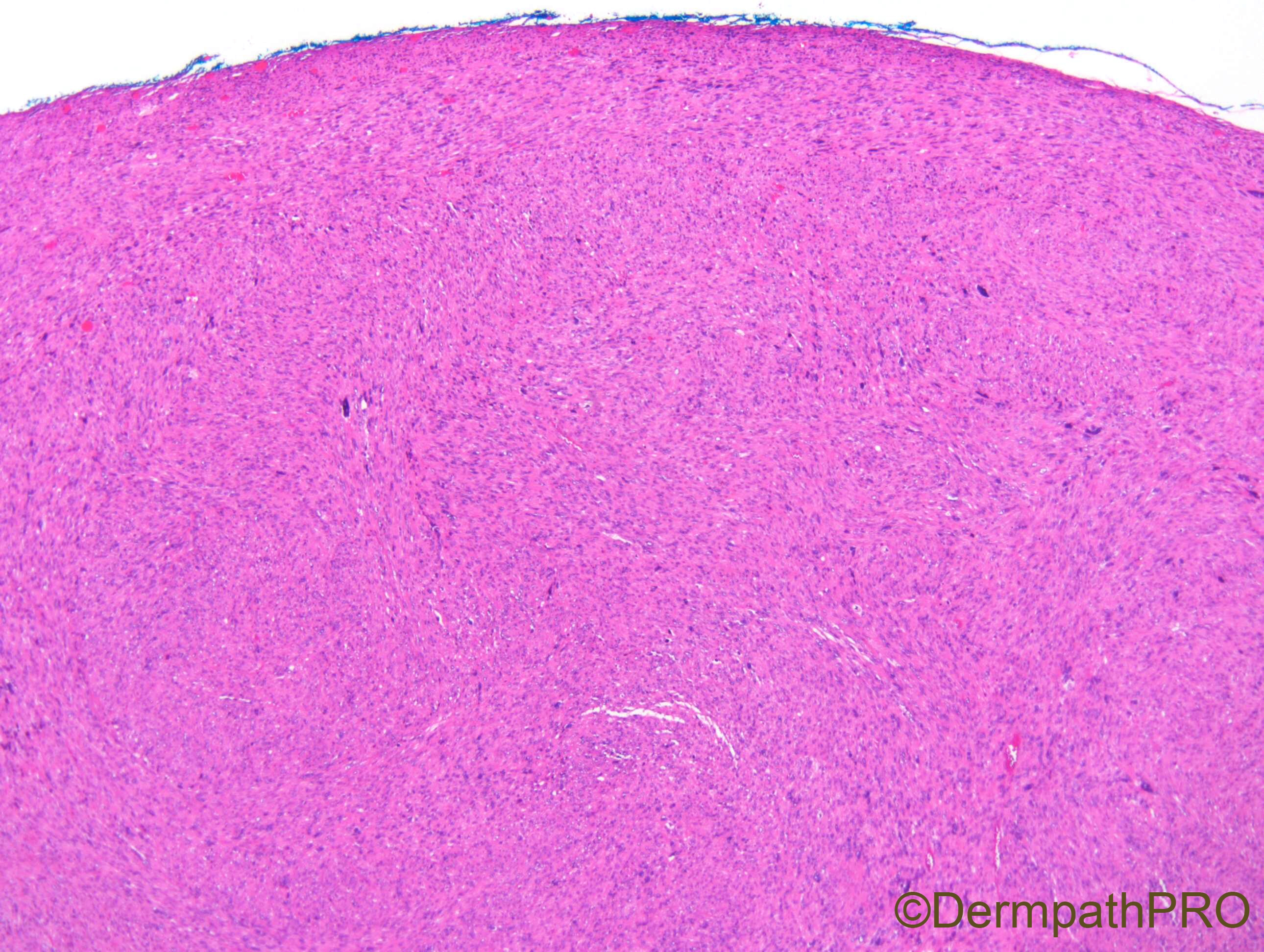
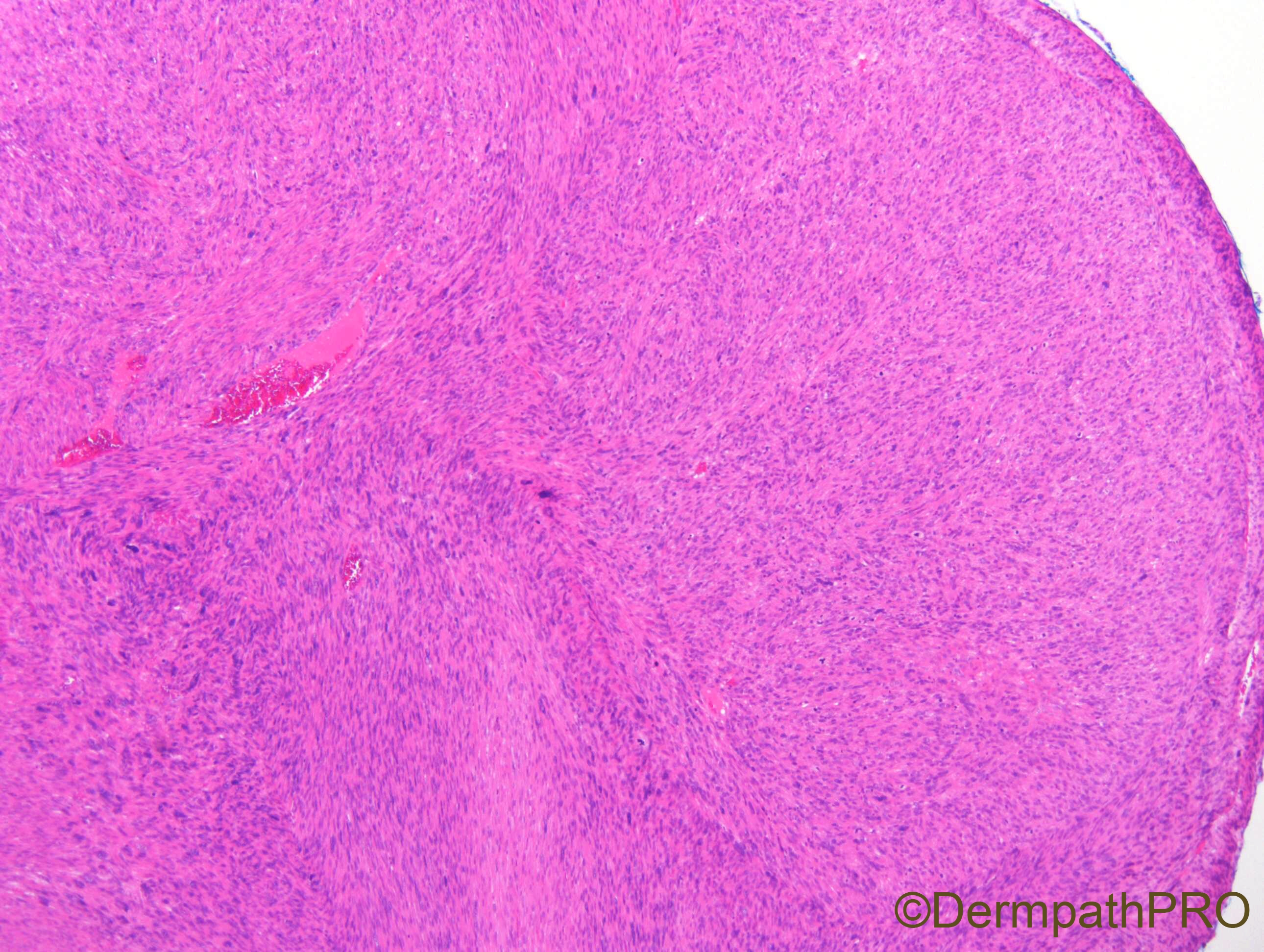
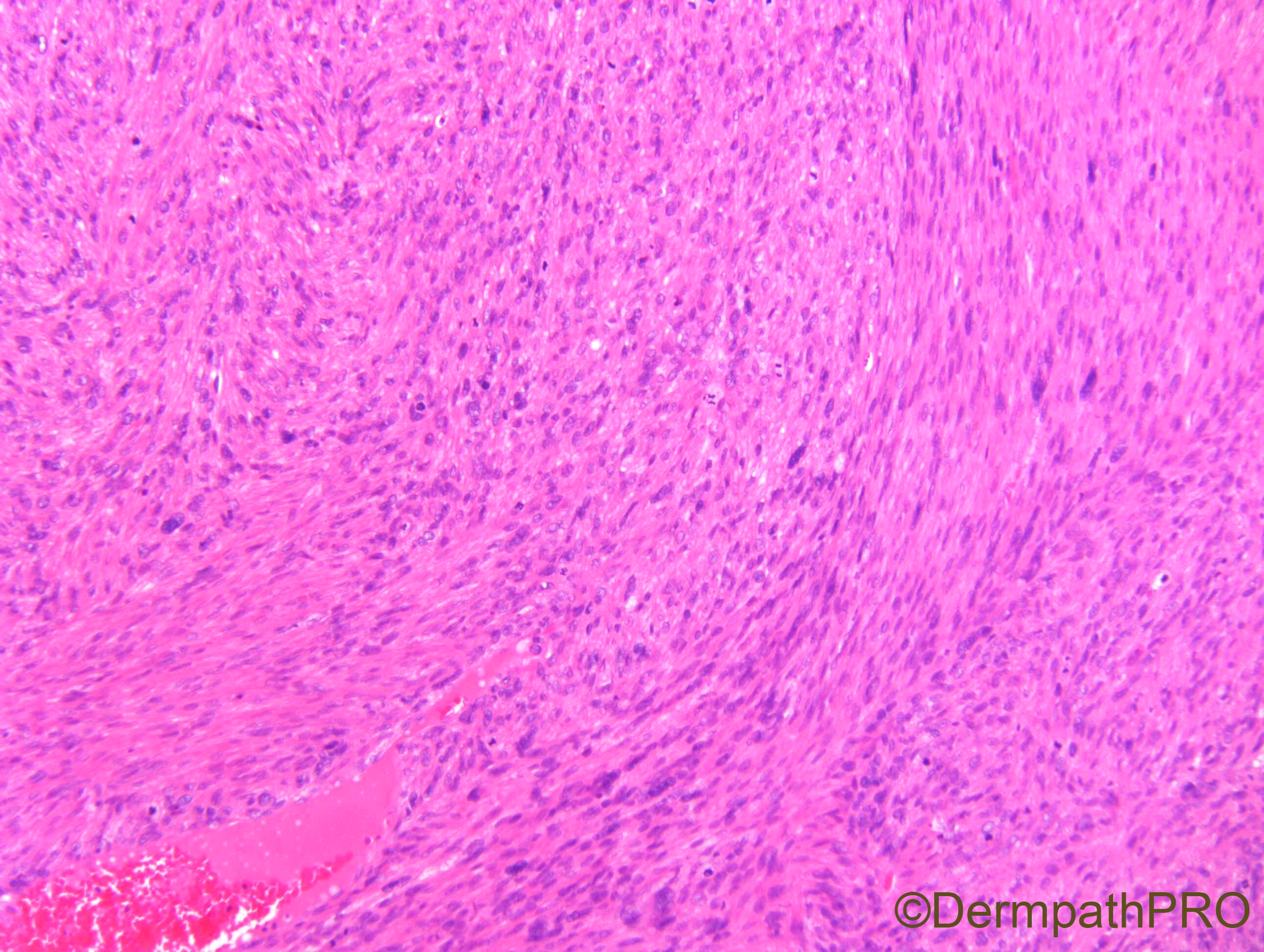
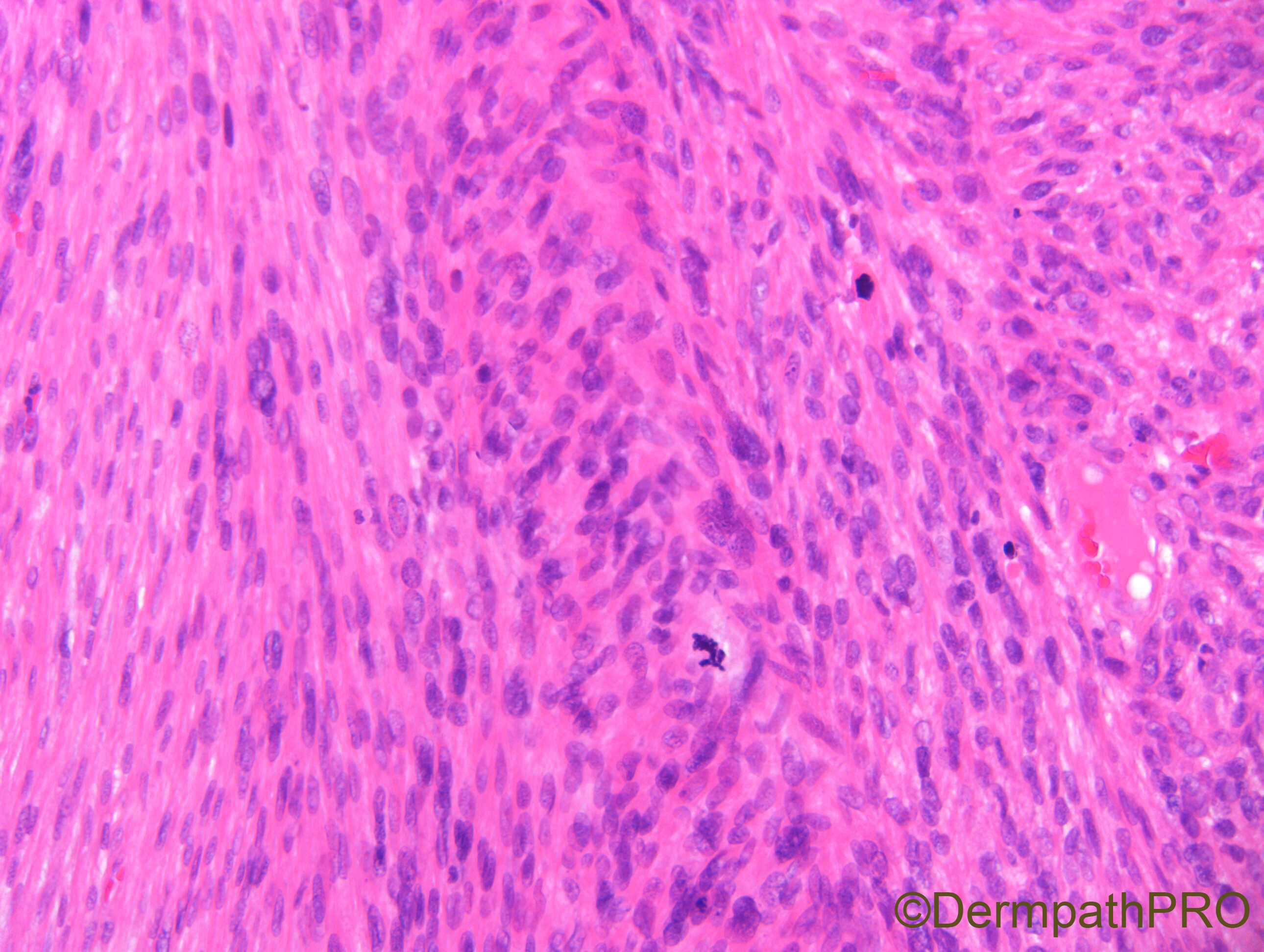
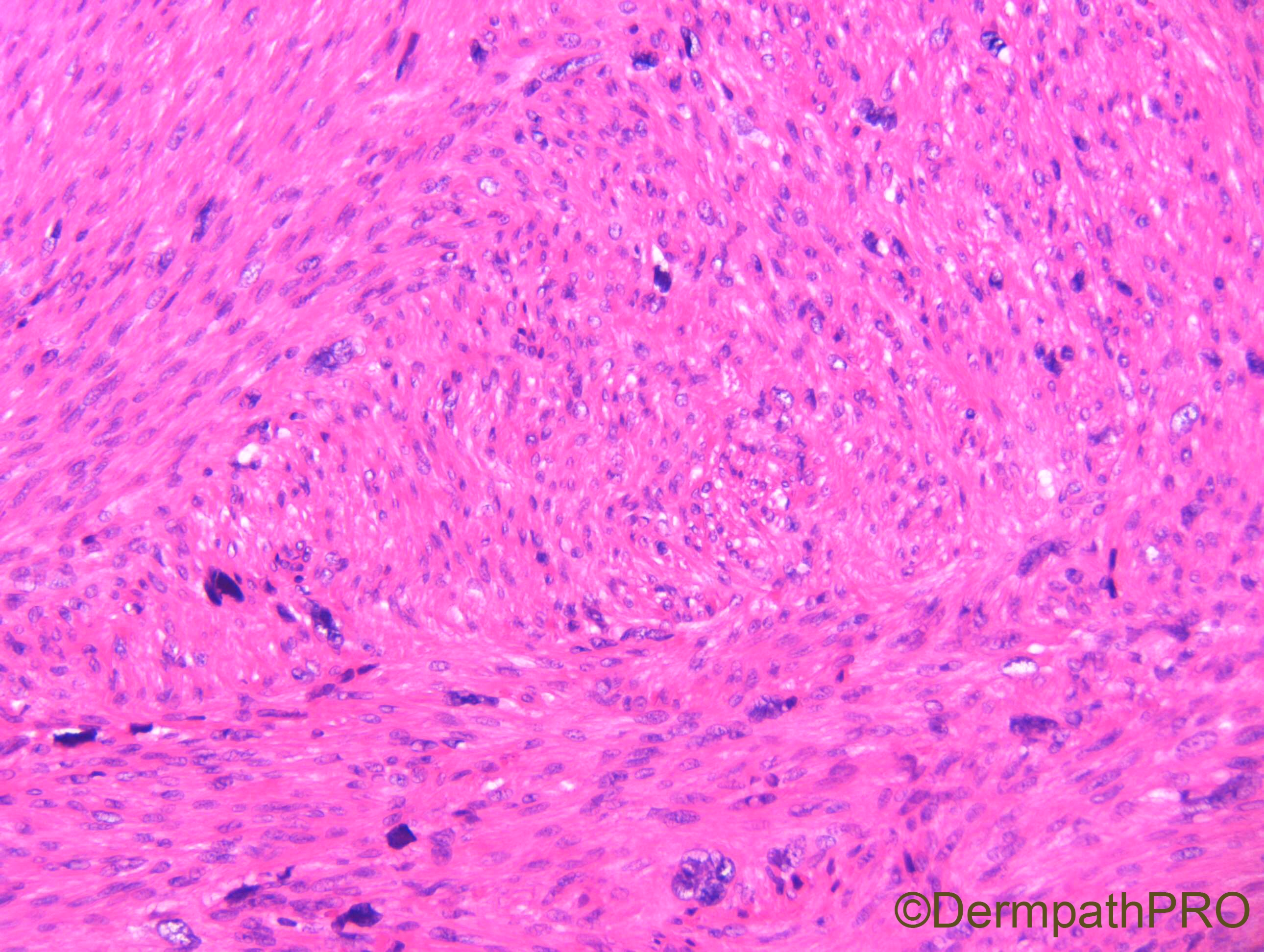
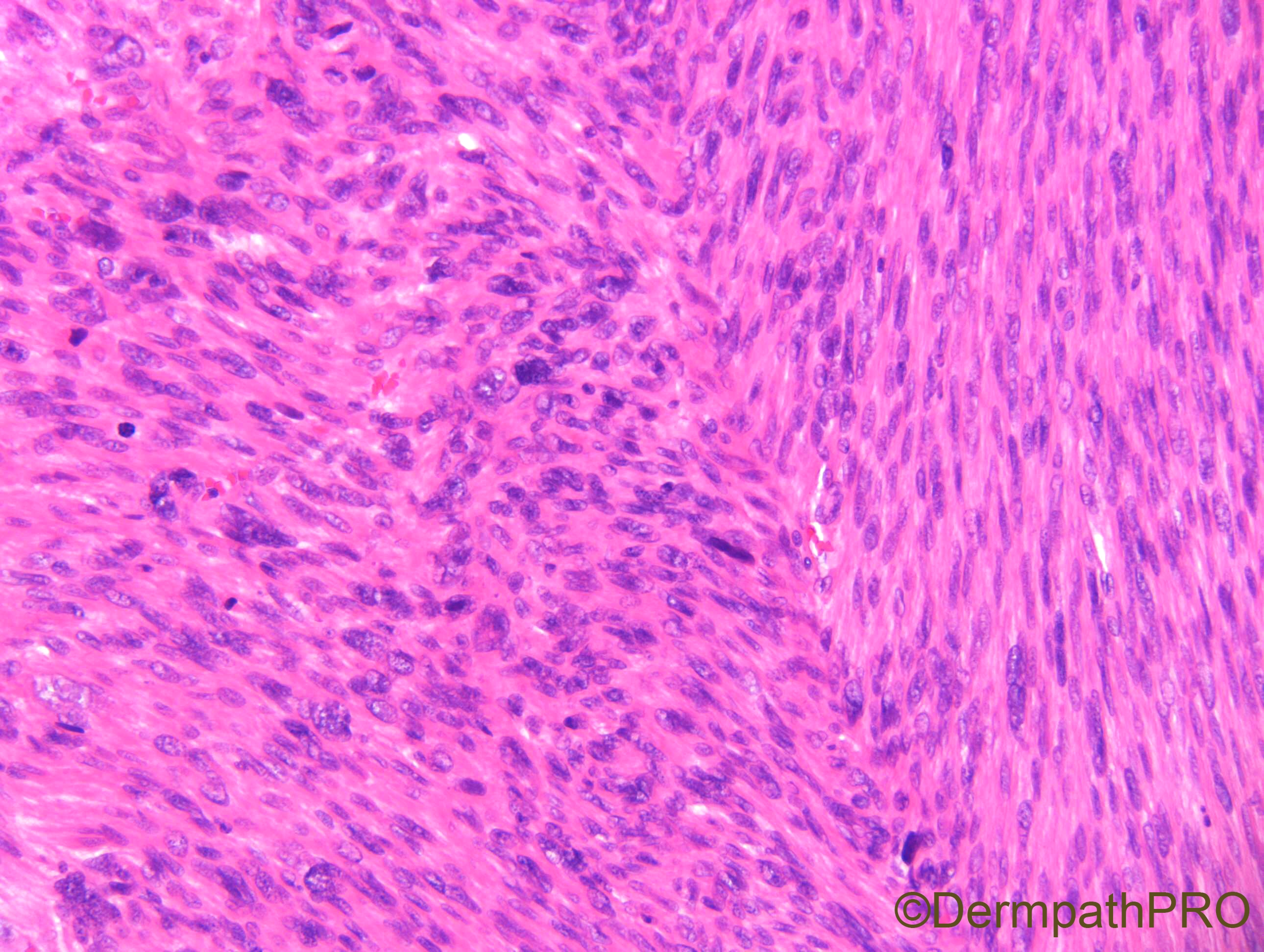
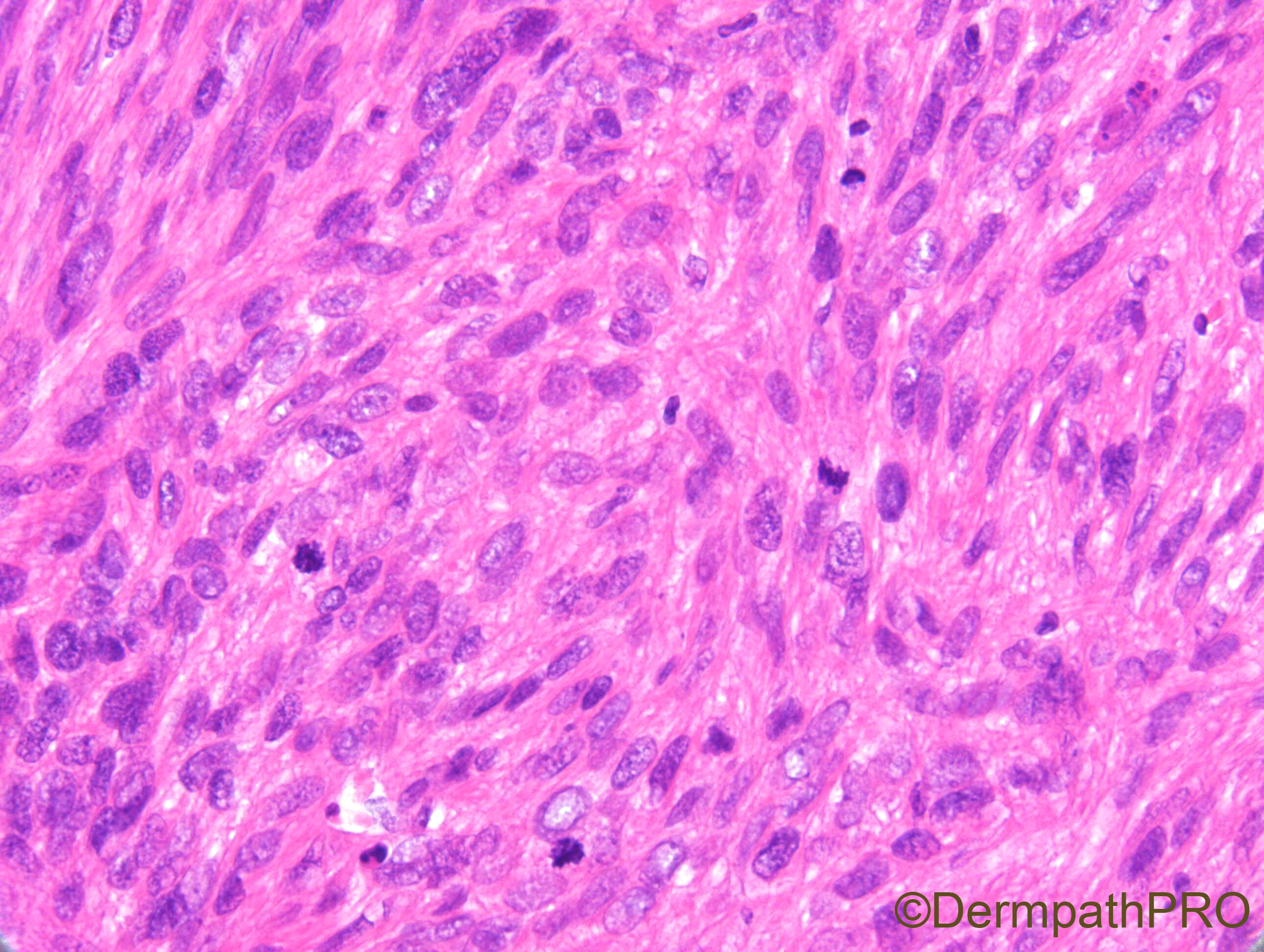
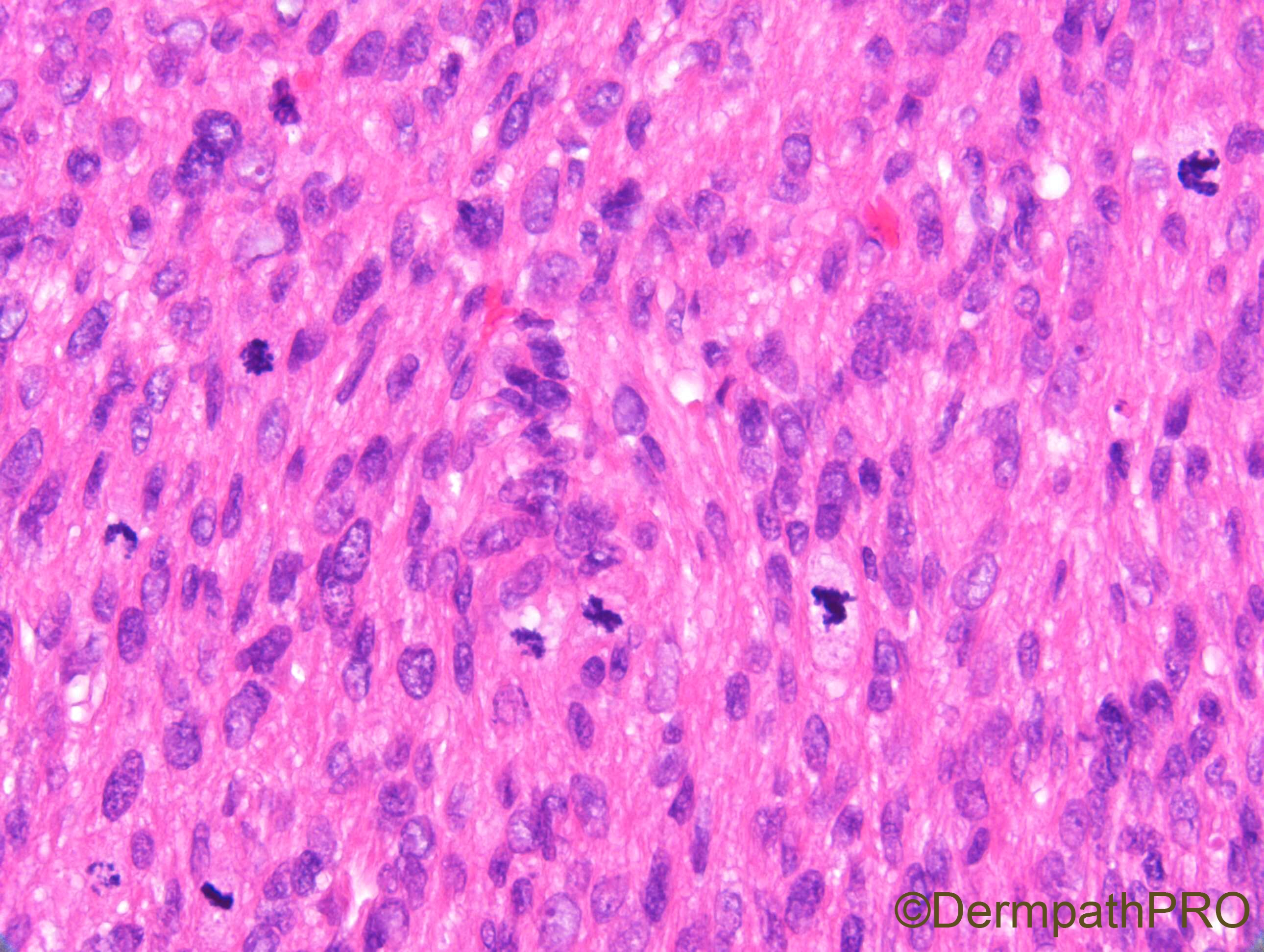
F70. Vulval cystic nodule.

Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.