-
 2
2
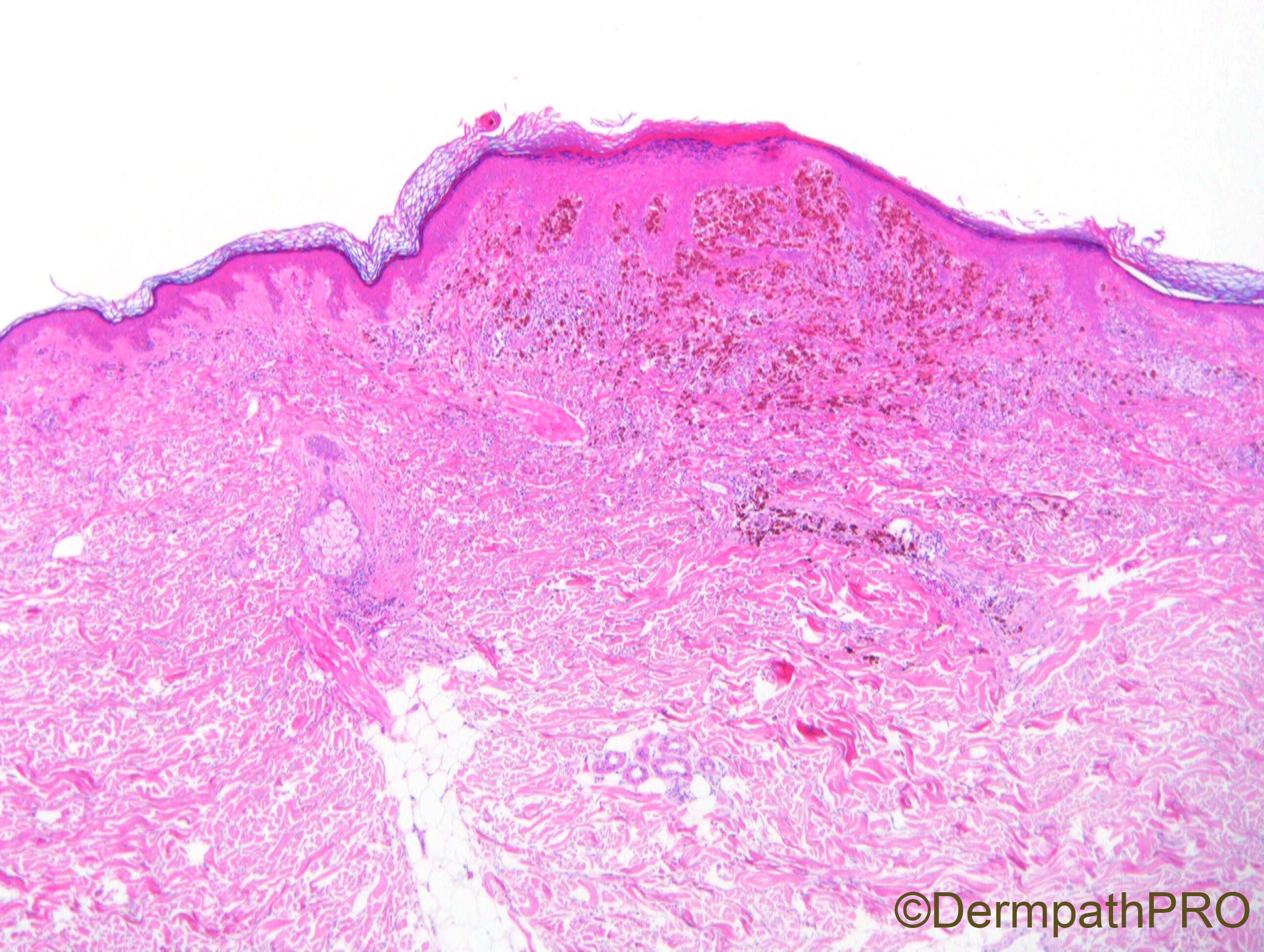
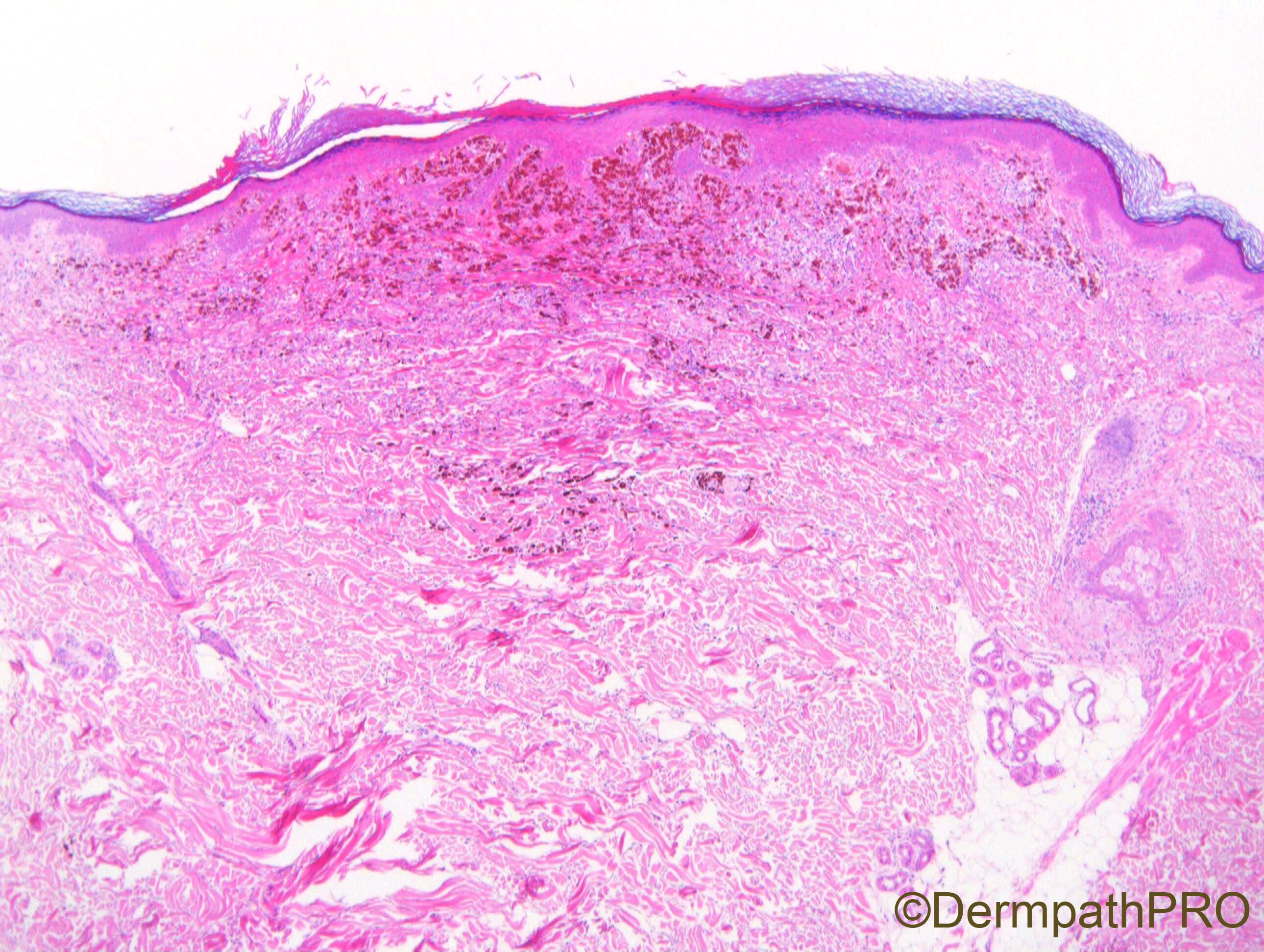
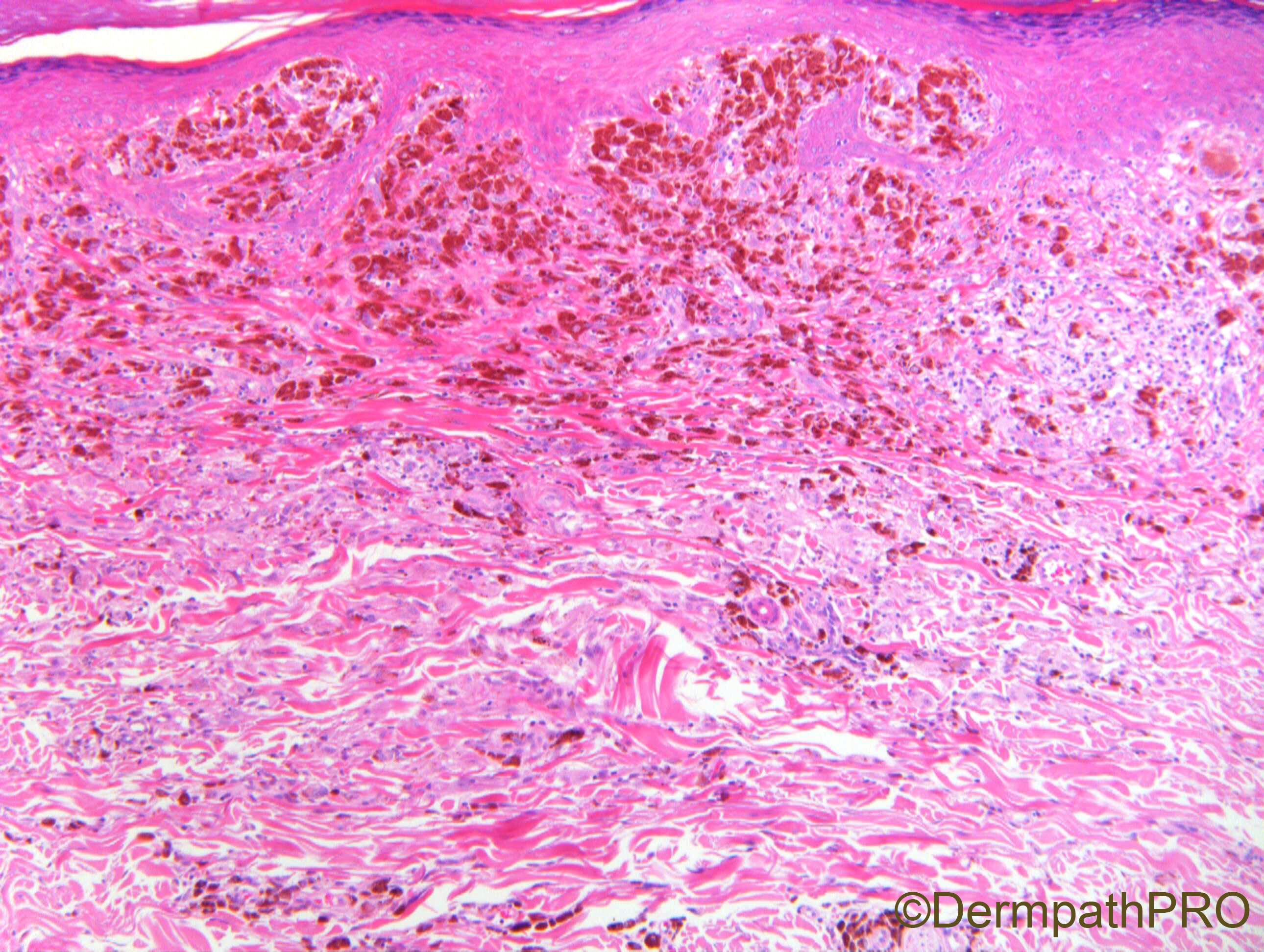
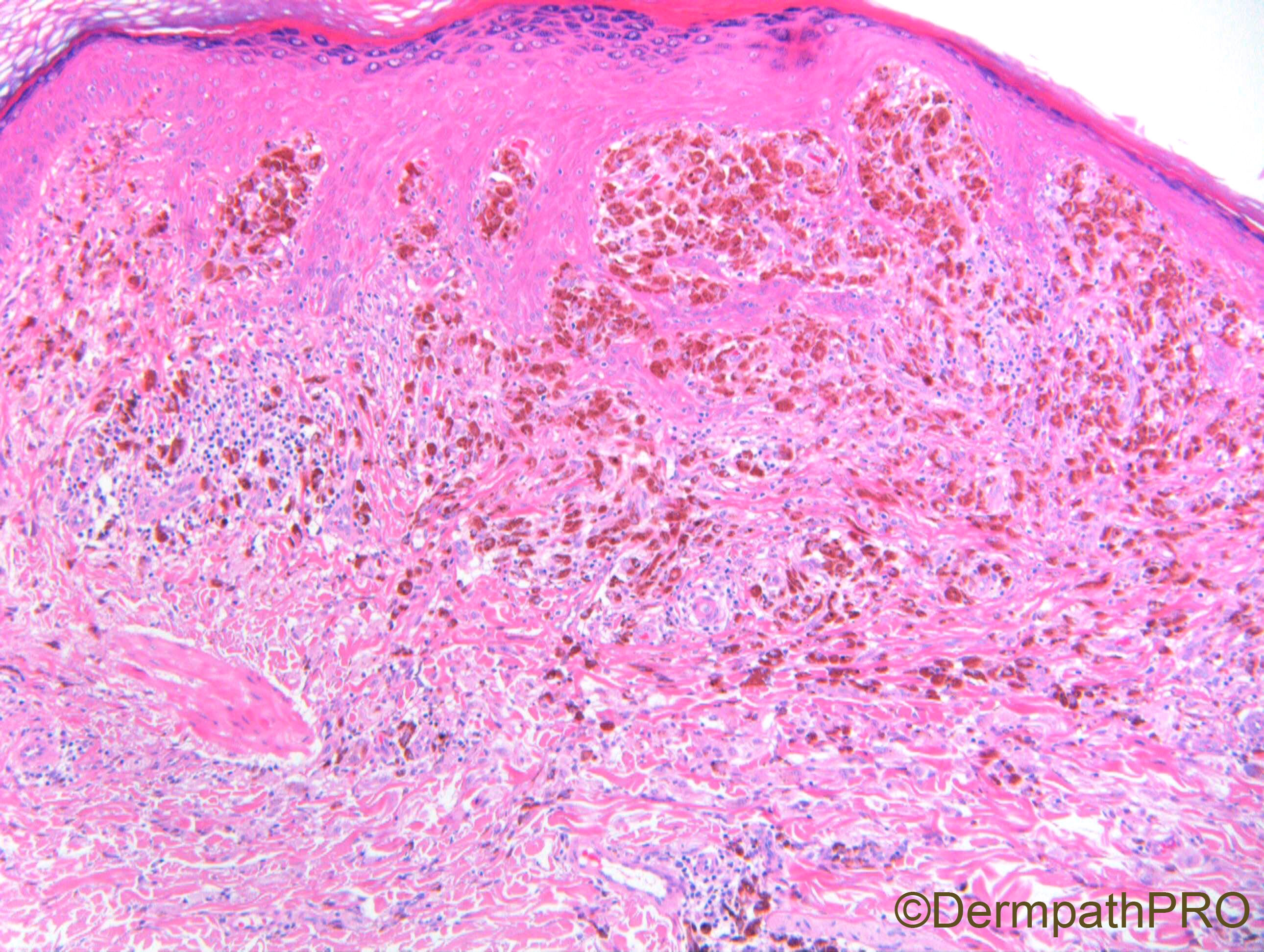
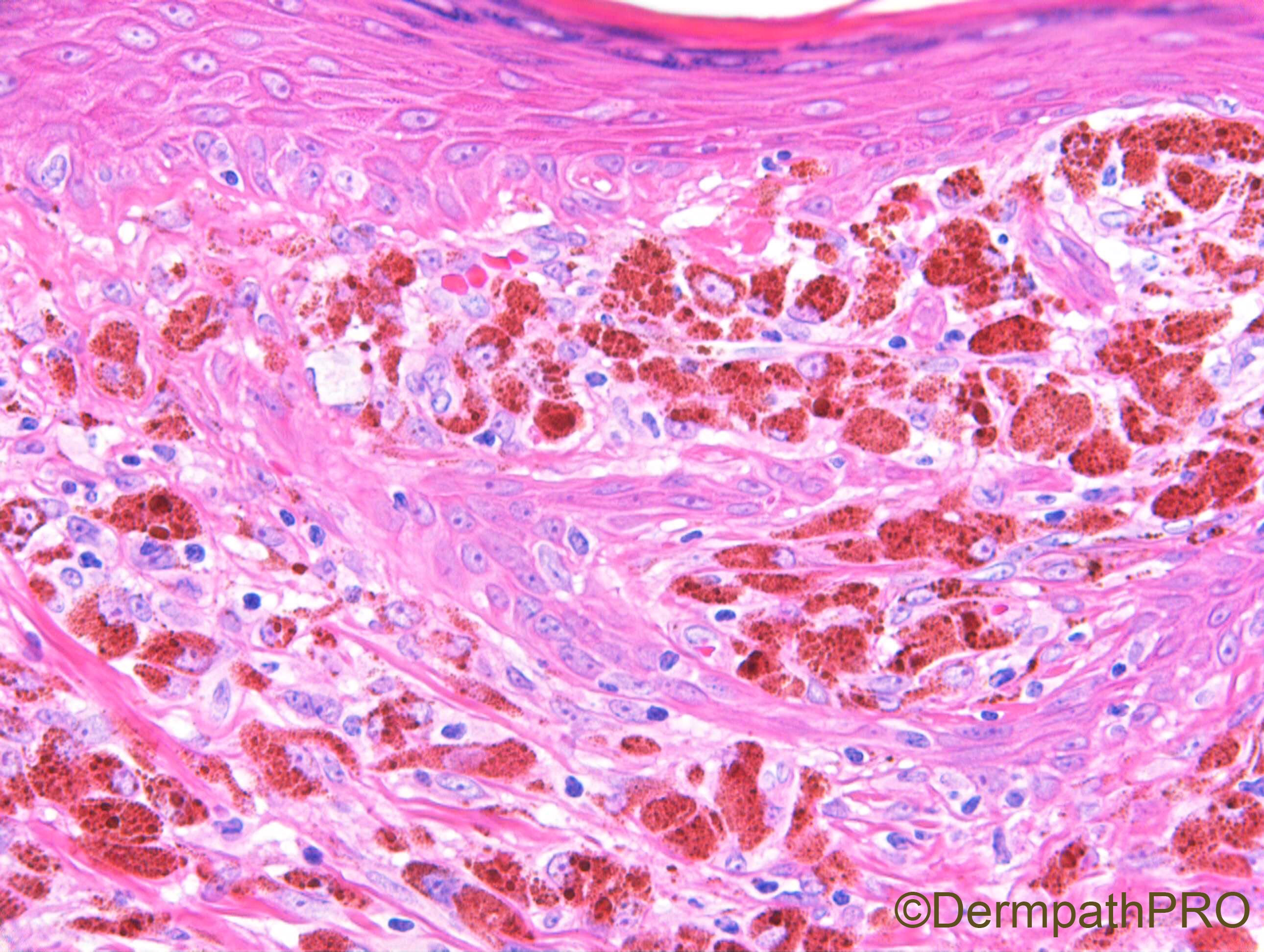
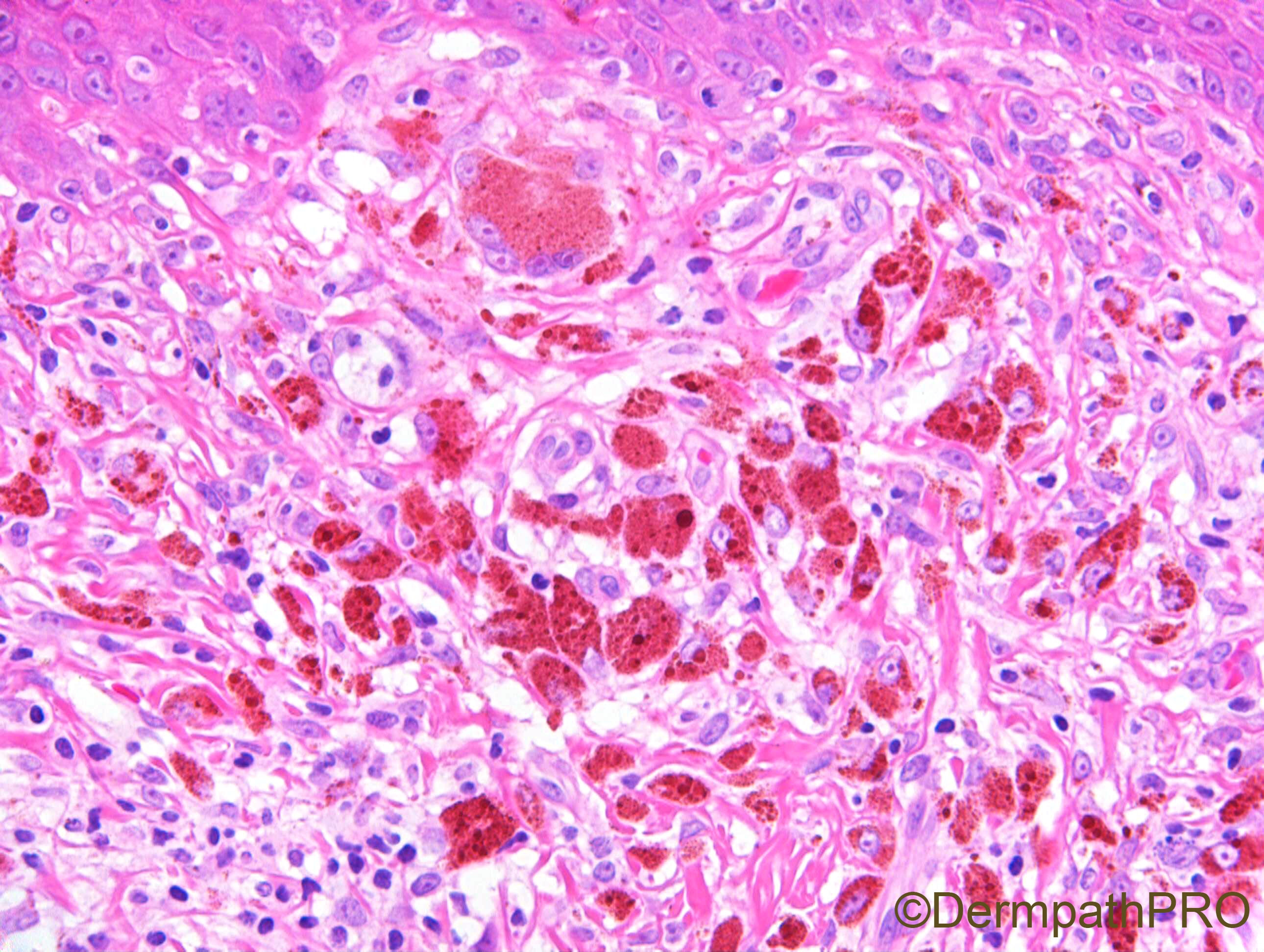
Case Number : Case 2172 - 5 October 2018 Posted By: Dr. Richard Carr
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
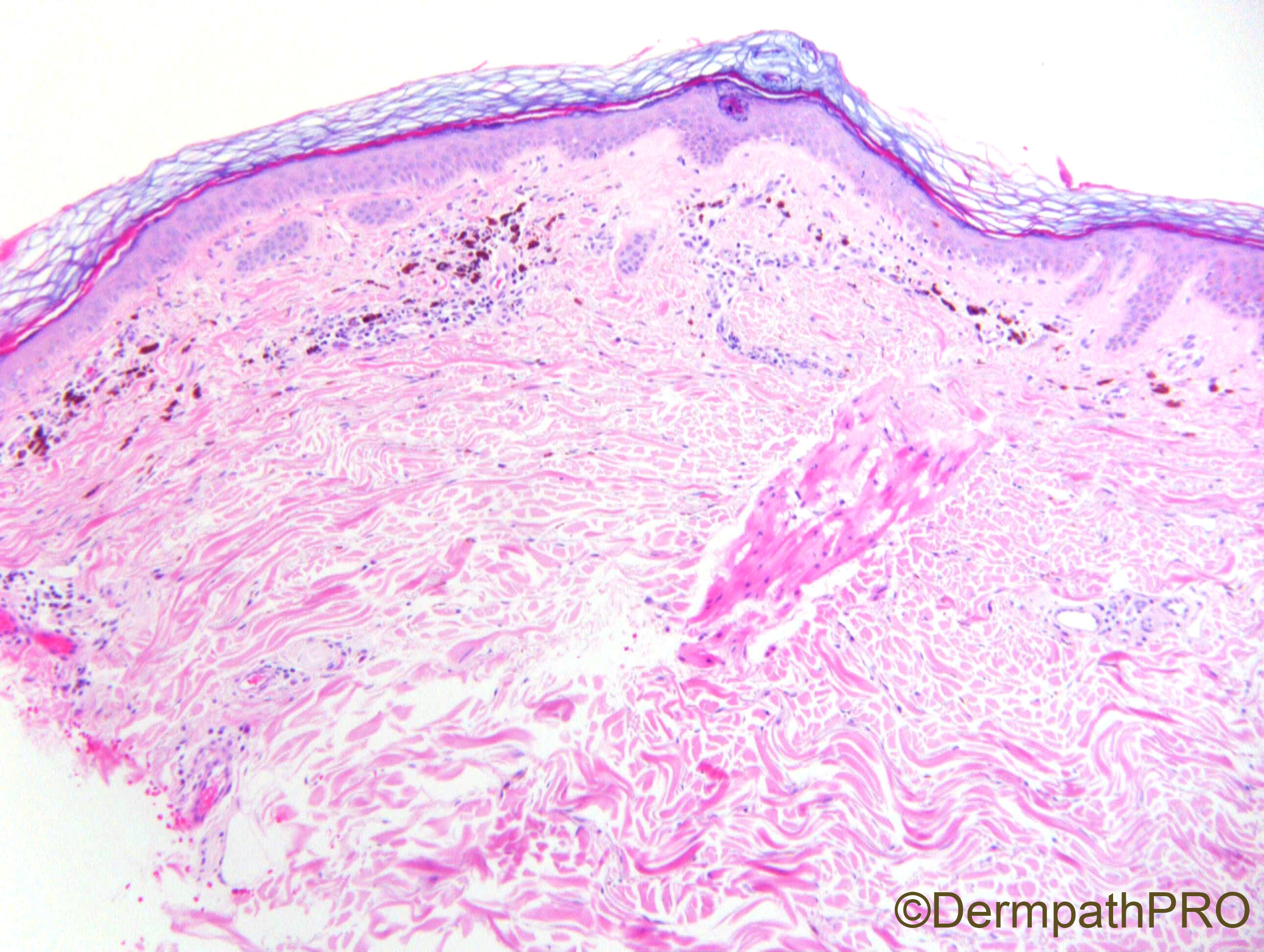
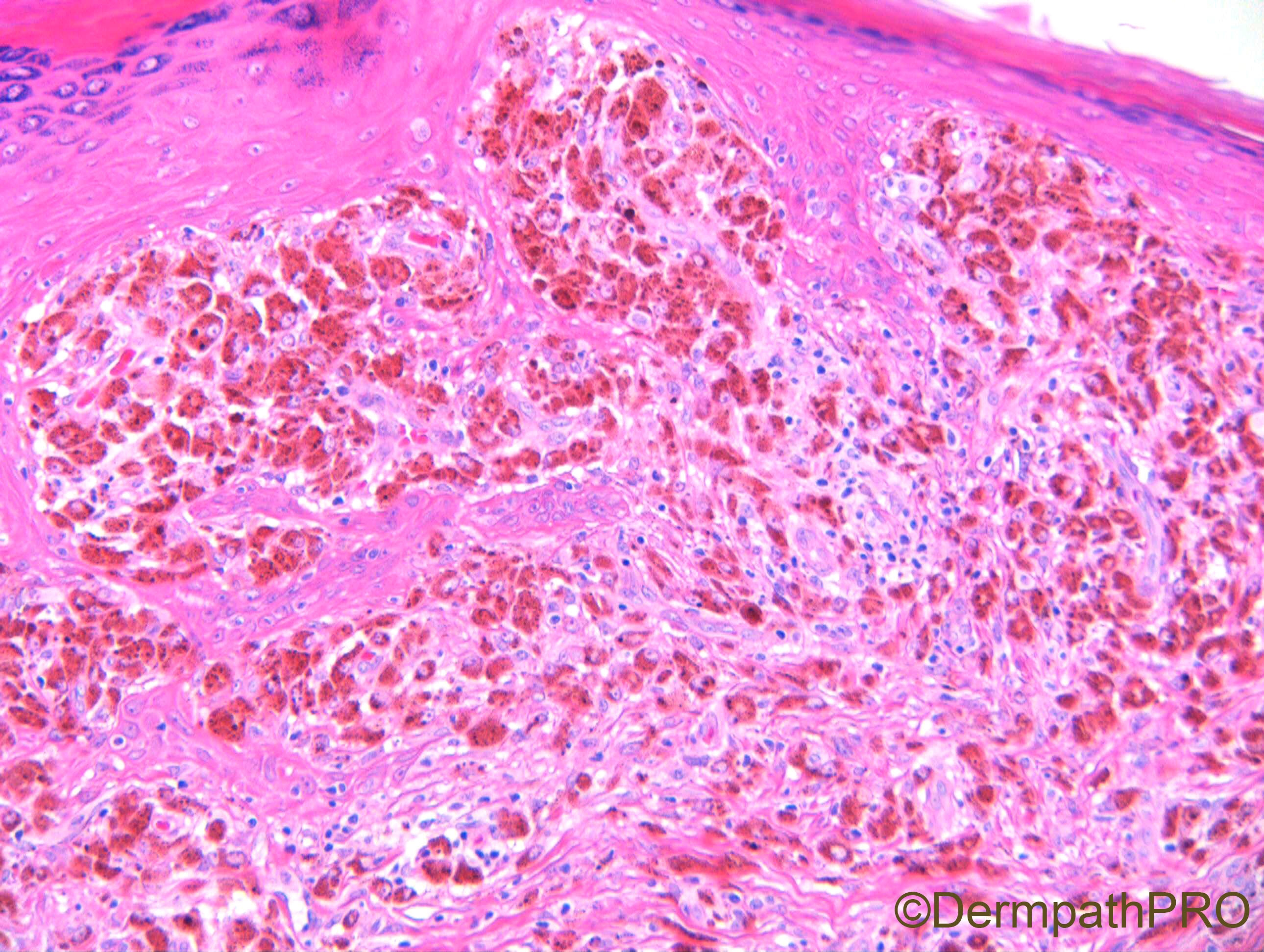
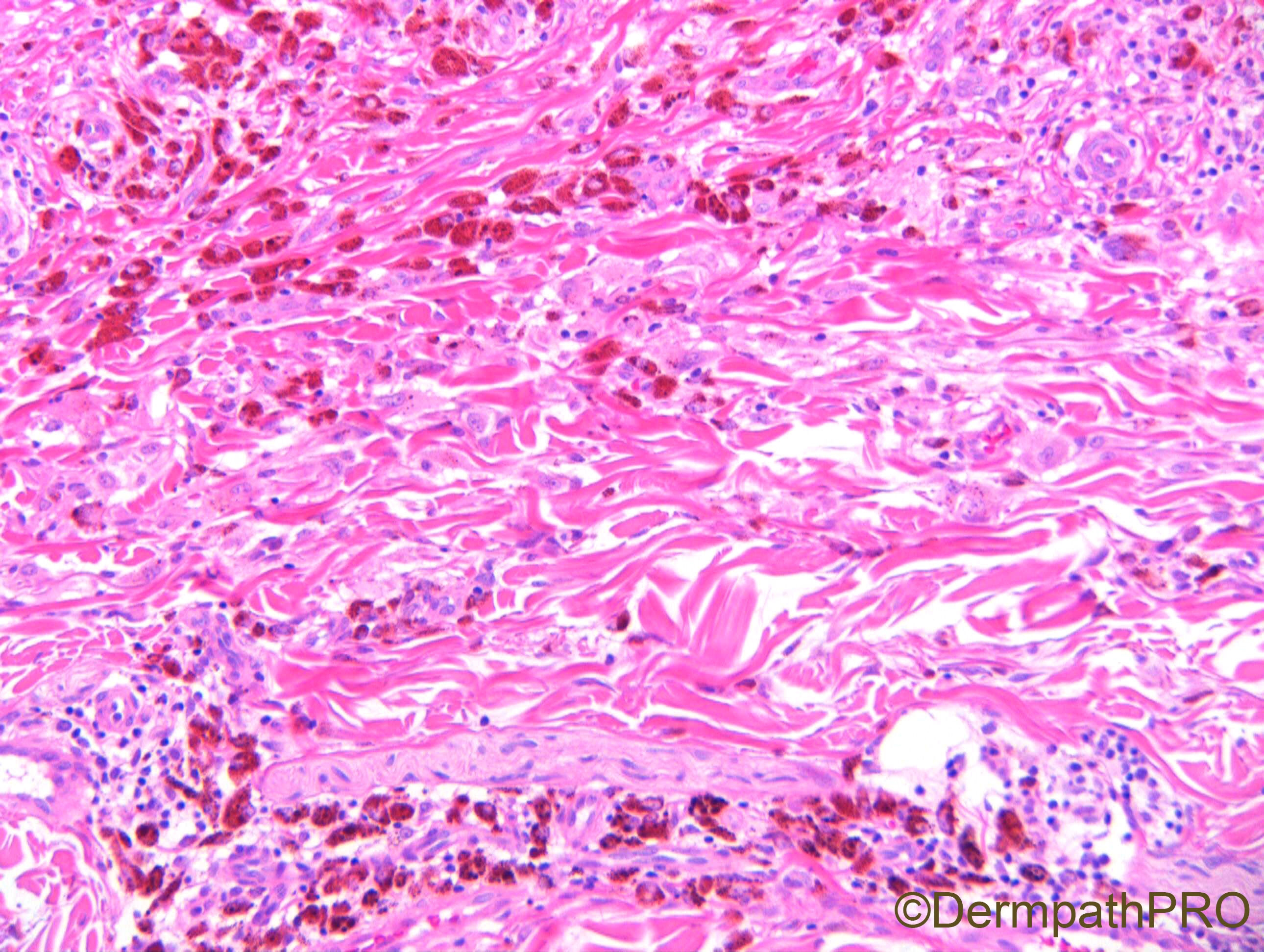
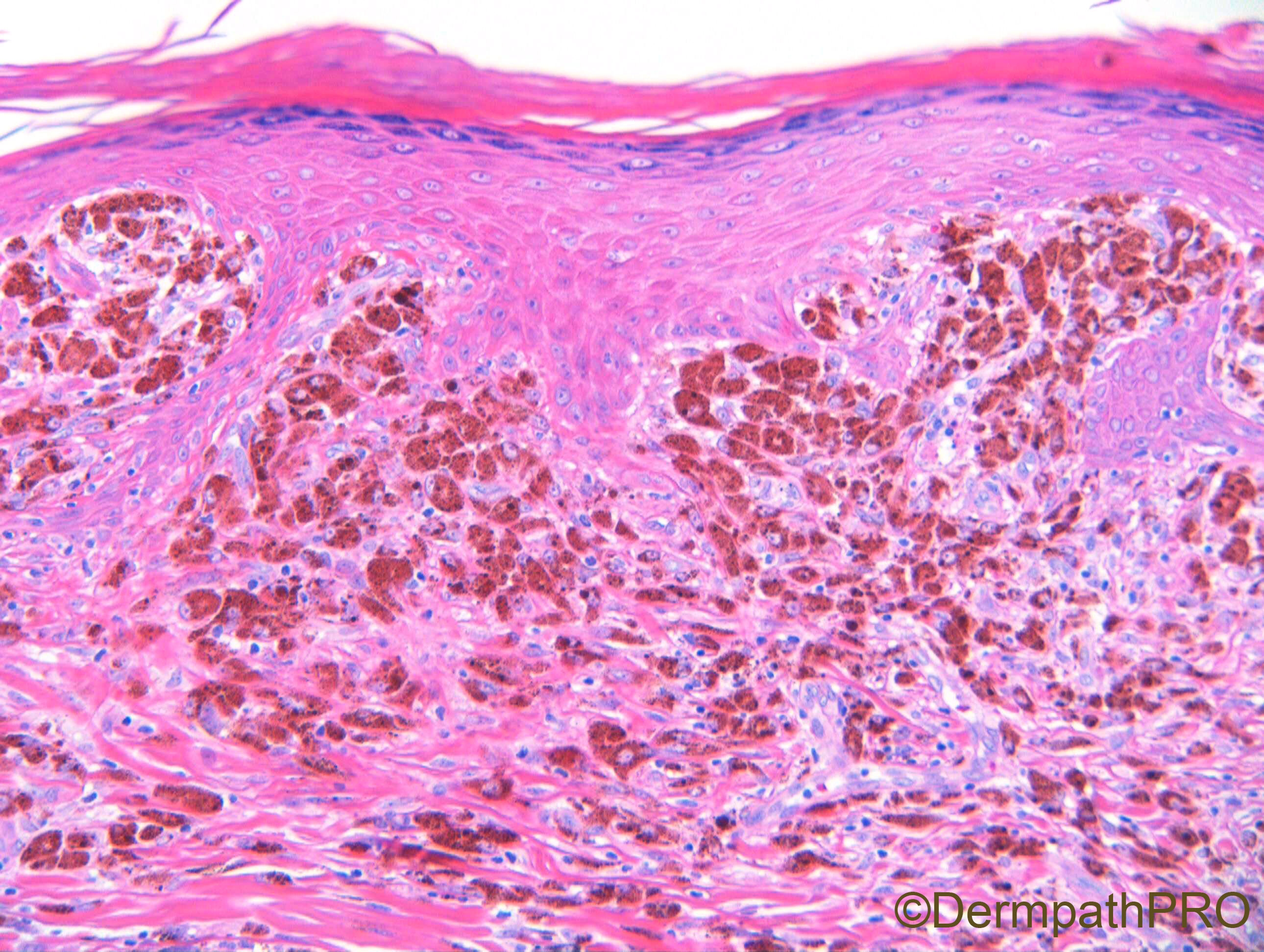
F65. 7 x 4mm lesion on back. ?naevus ?melanoma

Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.