Edited by Admin_Dermpath
Case Number : Case 2465 - 13 December 2019 Posted By: Dr. Richard Carr
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
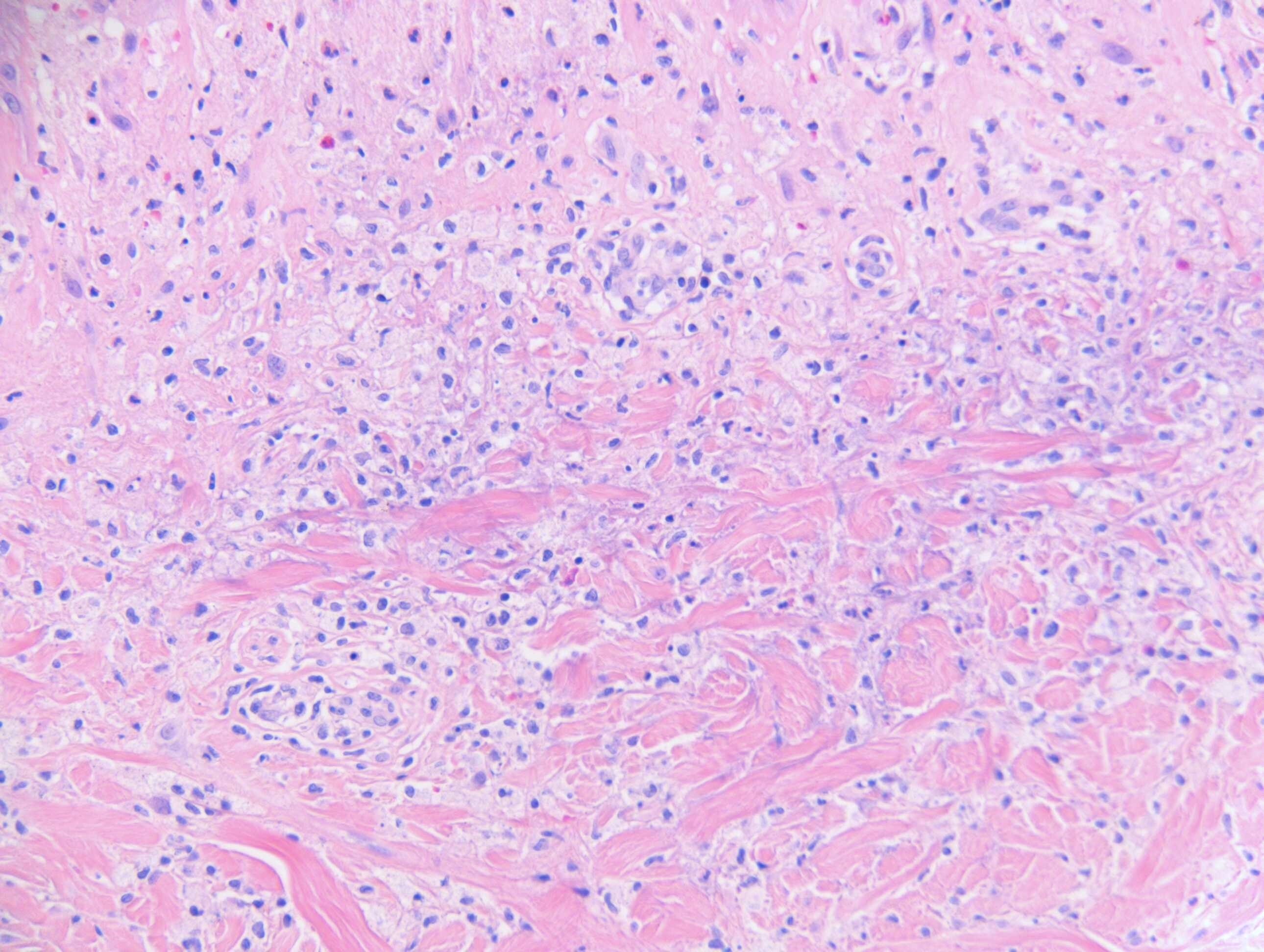
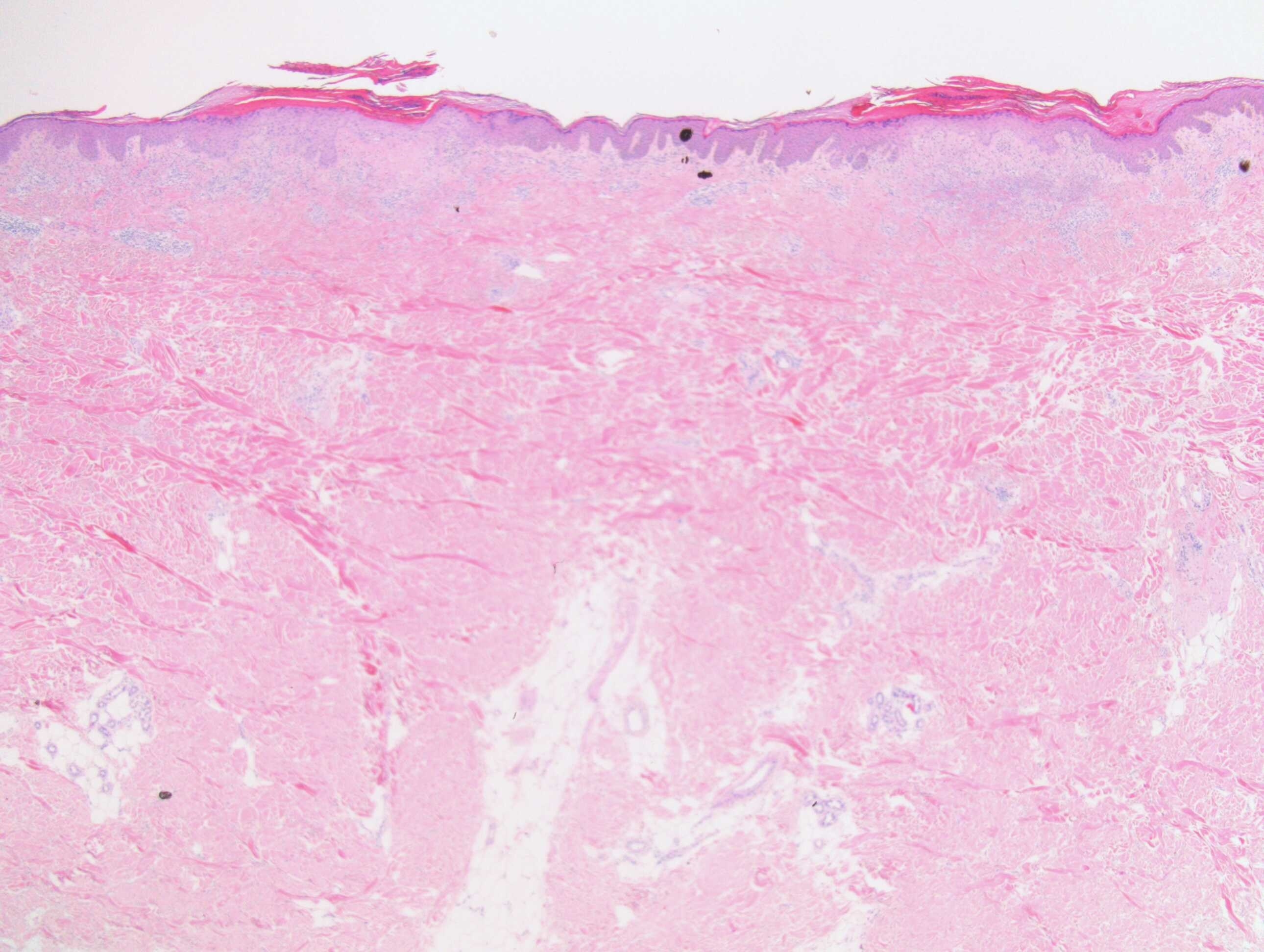
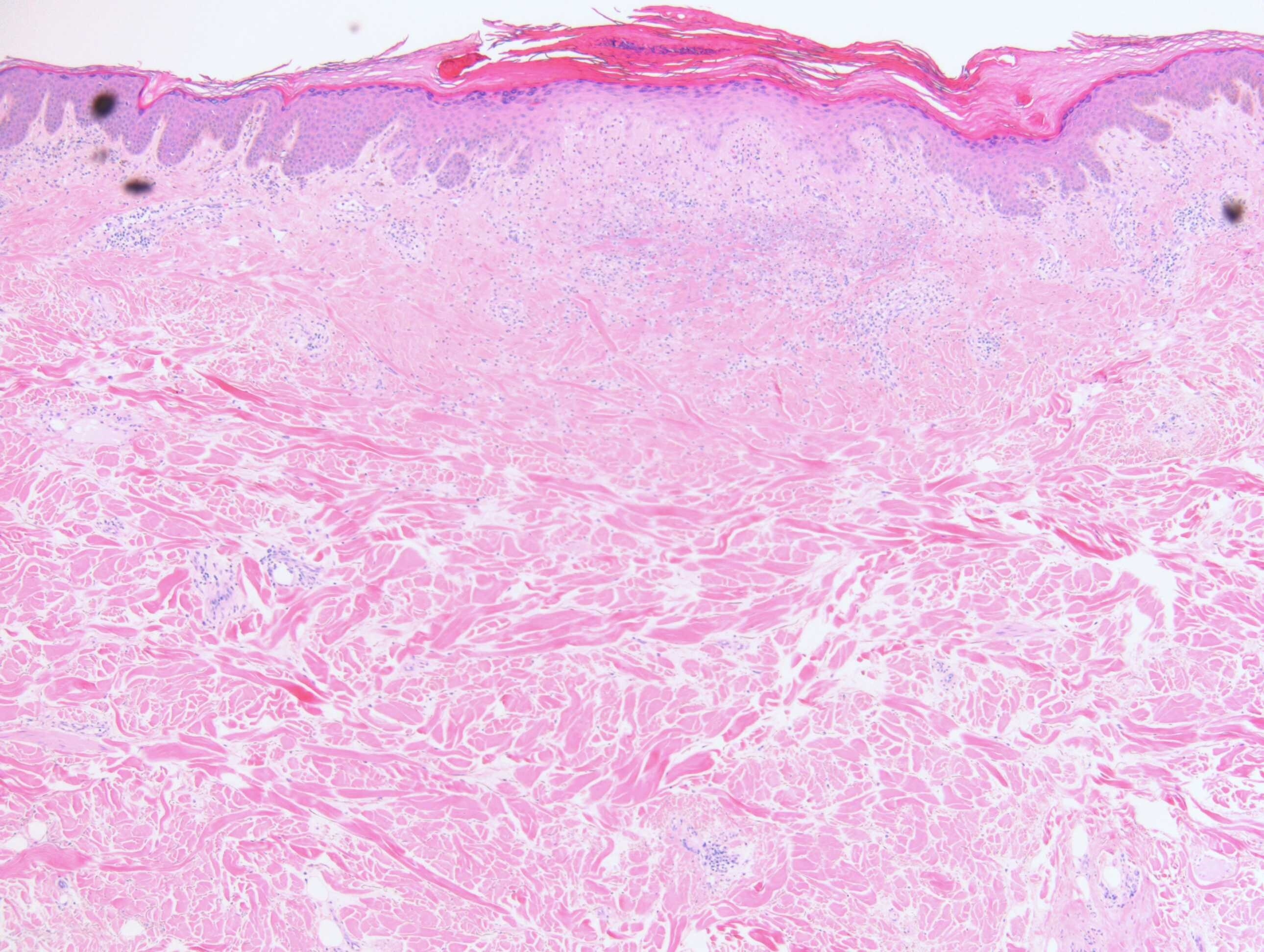
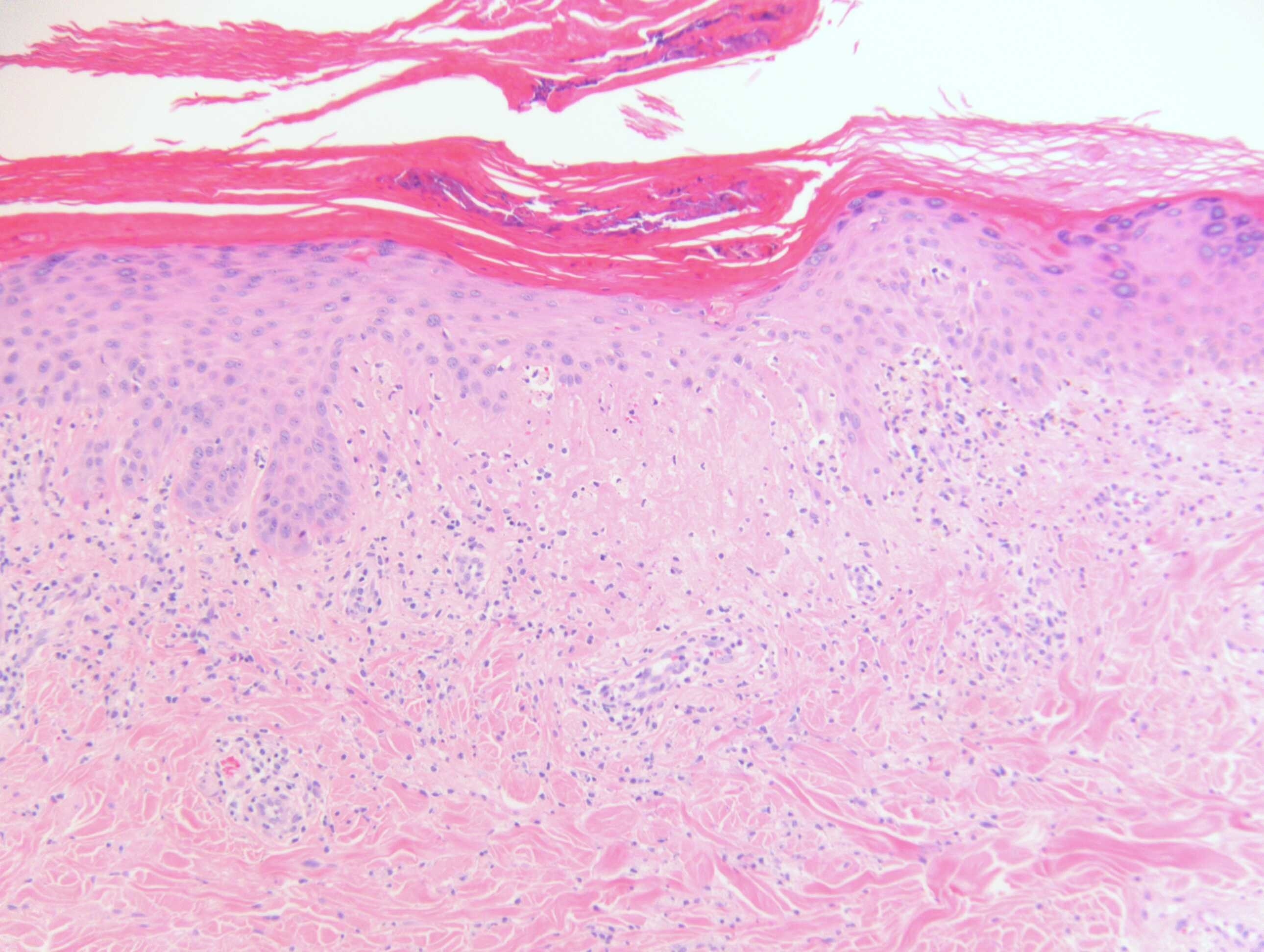
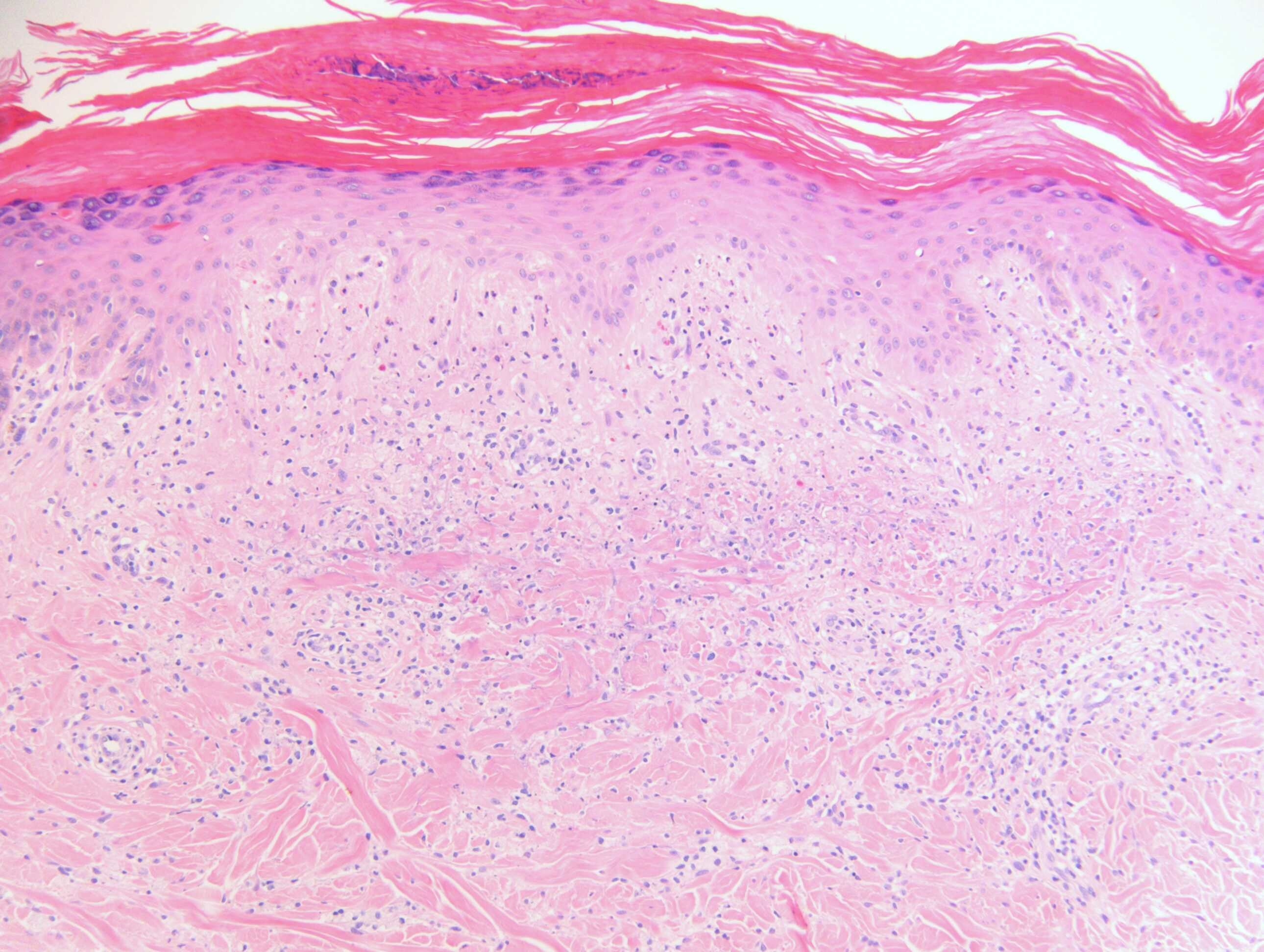
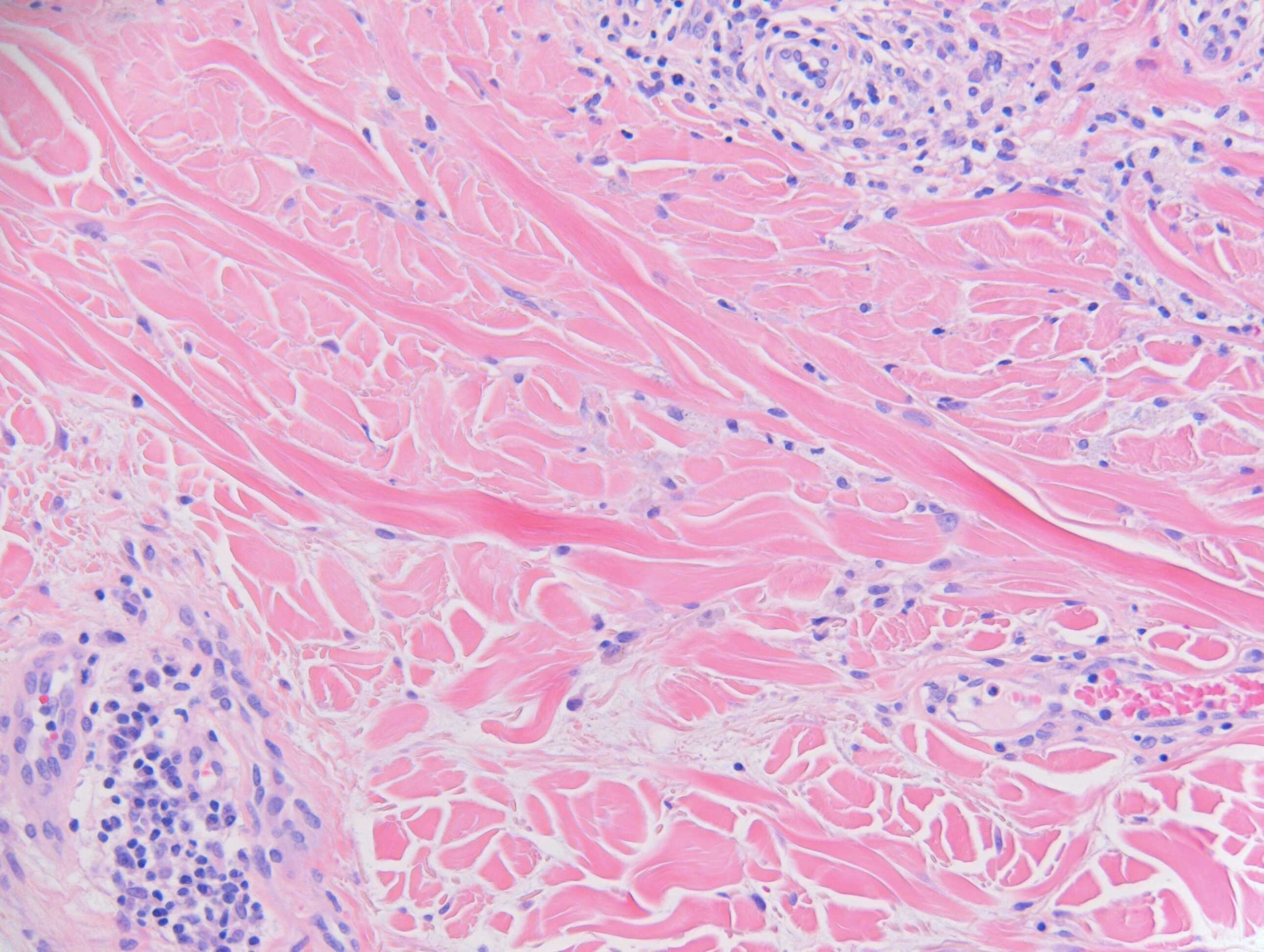
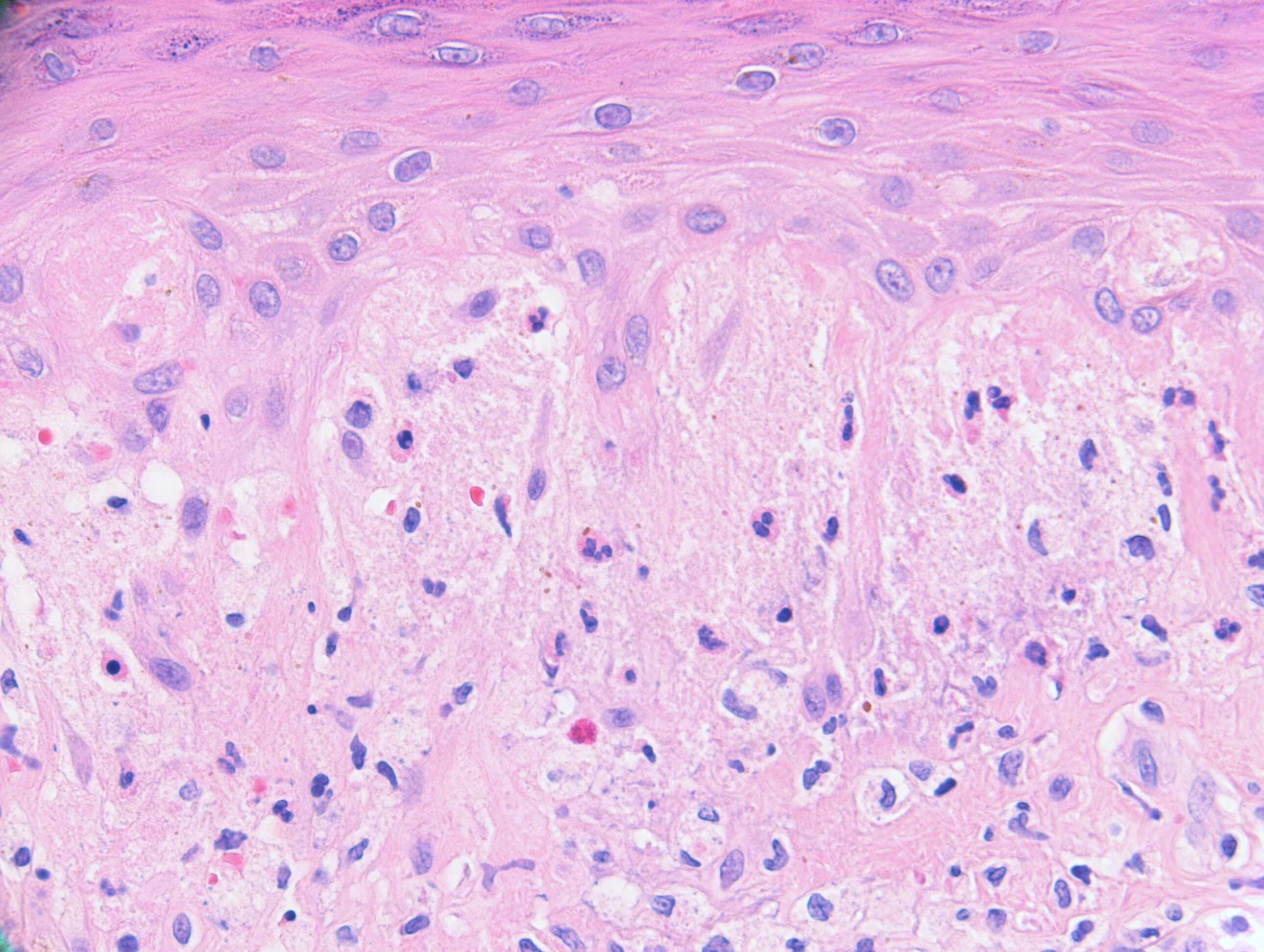
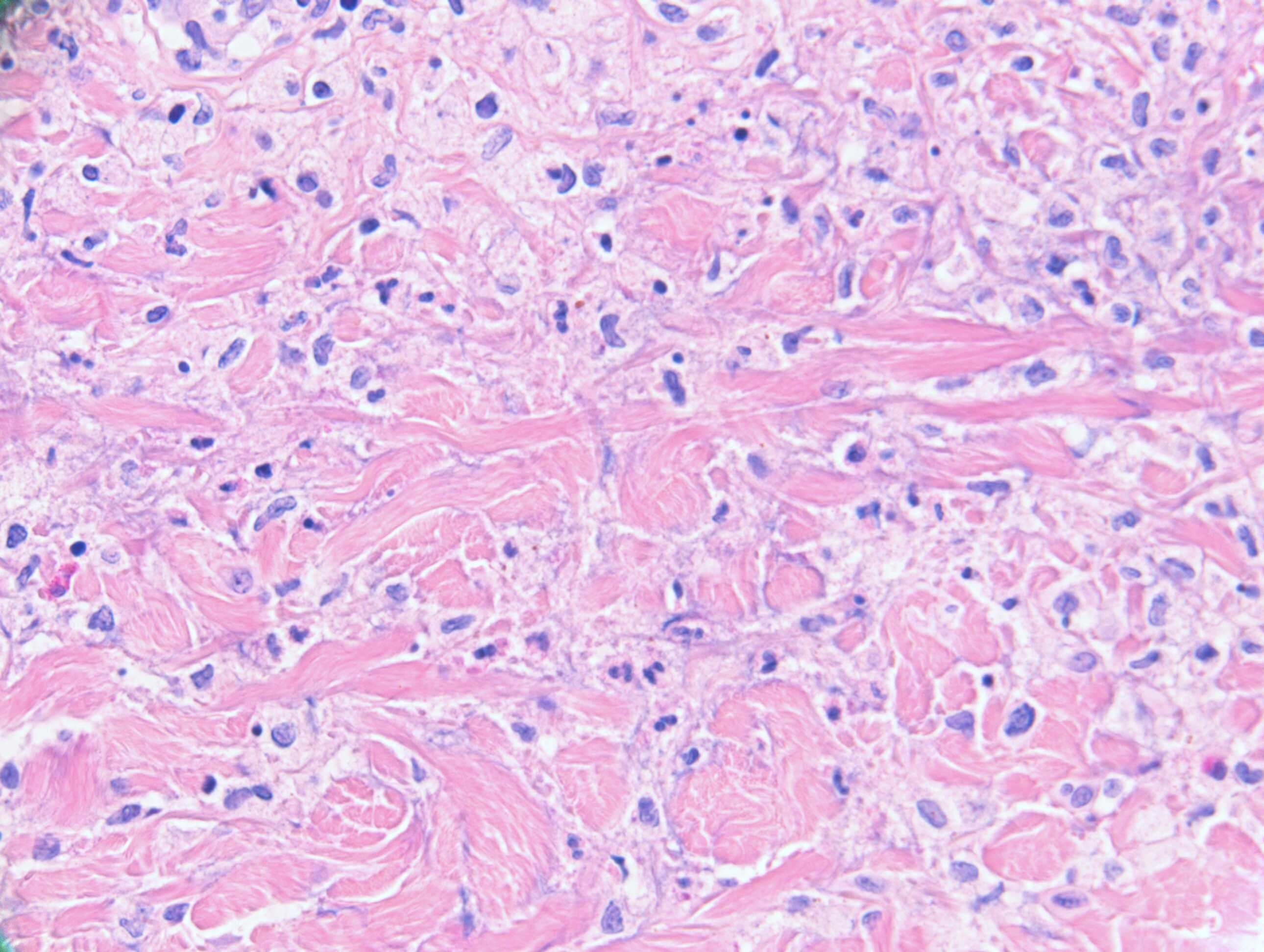
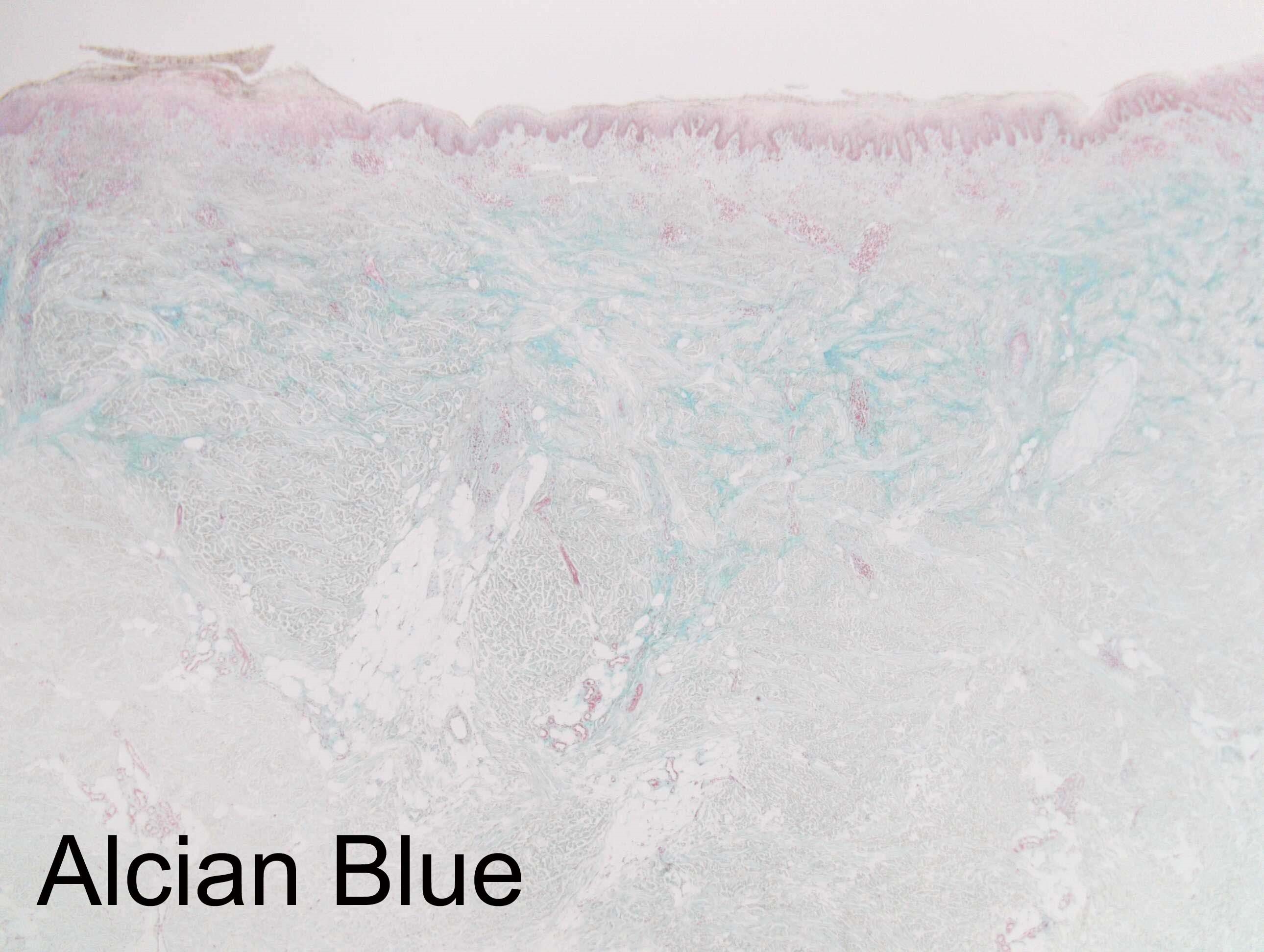
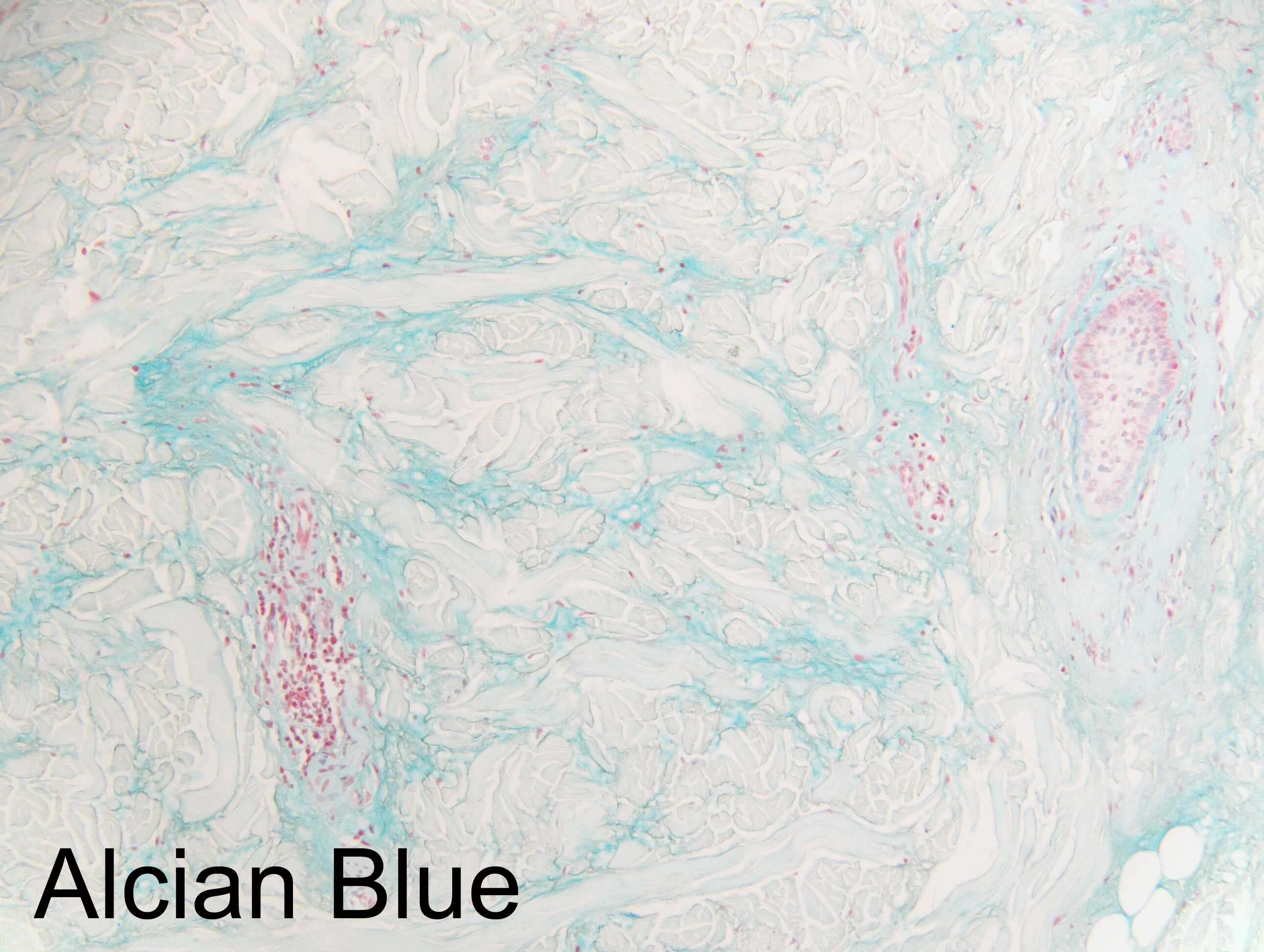
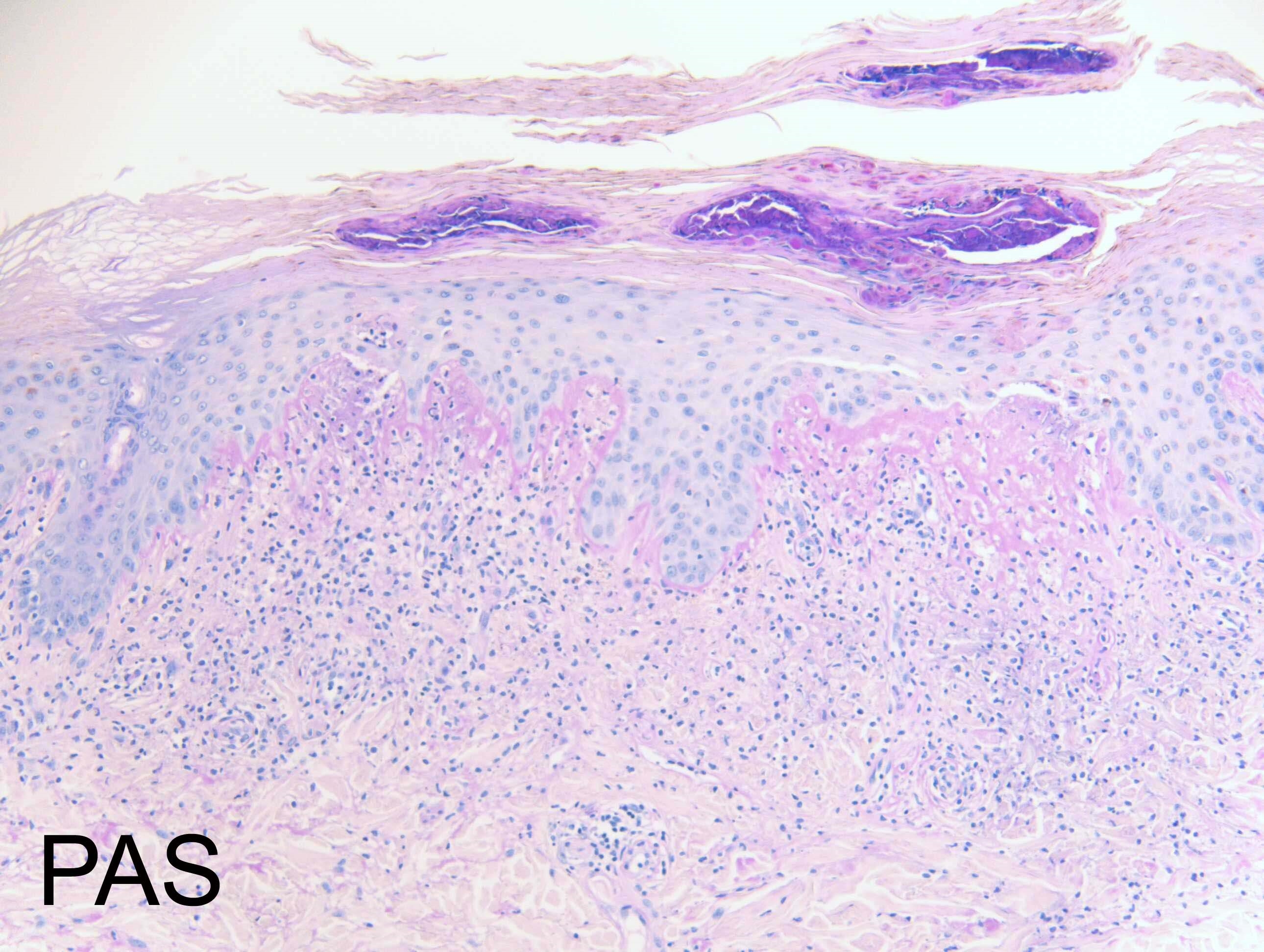
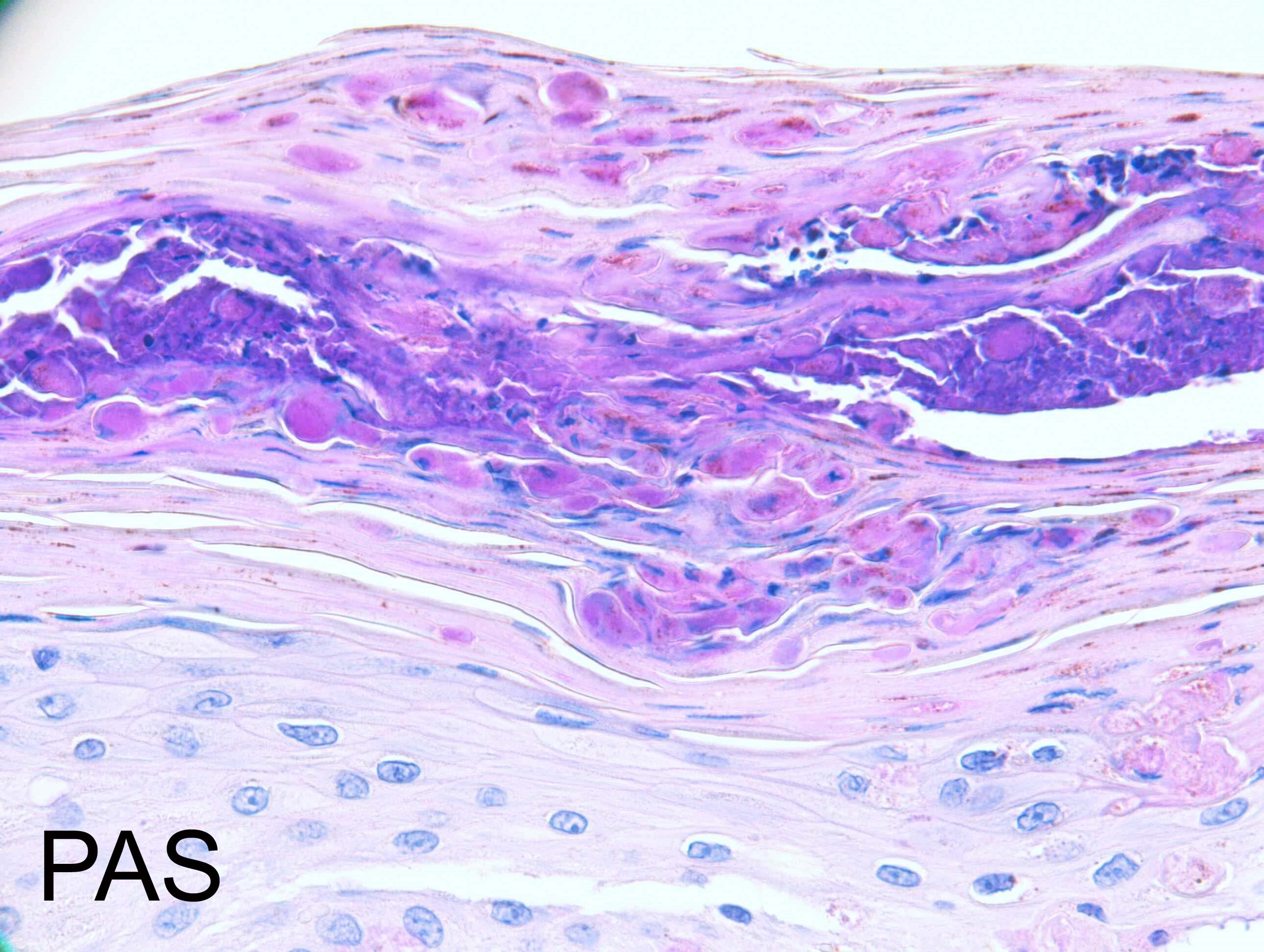
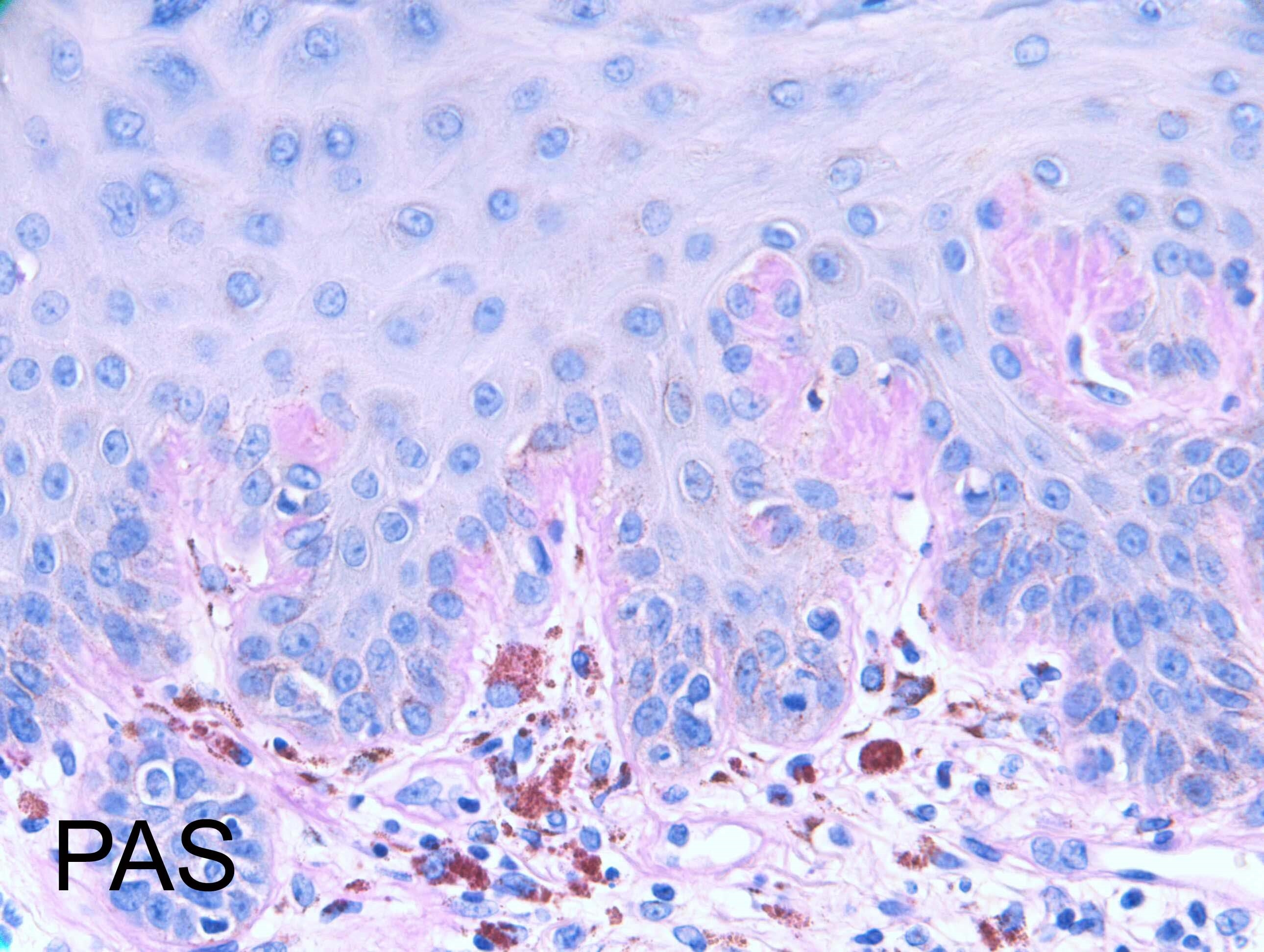
Itchy macular papular rash, prickling sensation since March 2019. Midline lower back,
back of shoulders & upper back, neck & scalp. ?lichen planus, ?lichen amyloidosis.
Skin type 4. Case c/o Dr Arti Bakshi
back of shoulders & upper back, neck & scalp. ?lichen planus, ?lichen amyloidosis.
Skin type 4. Case c/o Dr Arti Bakshi

Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.