-
 2
2
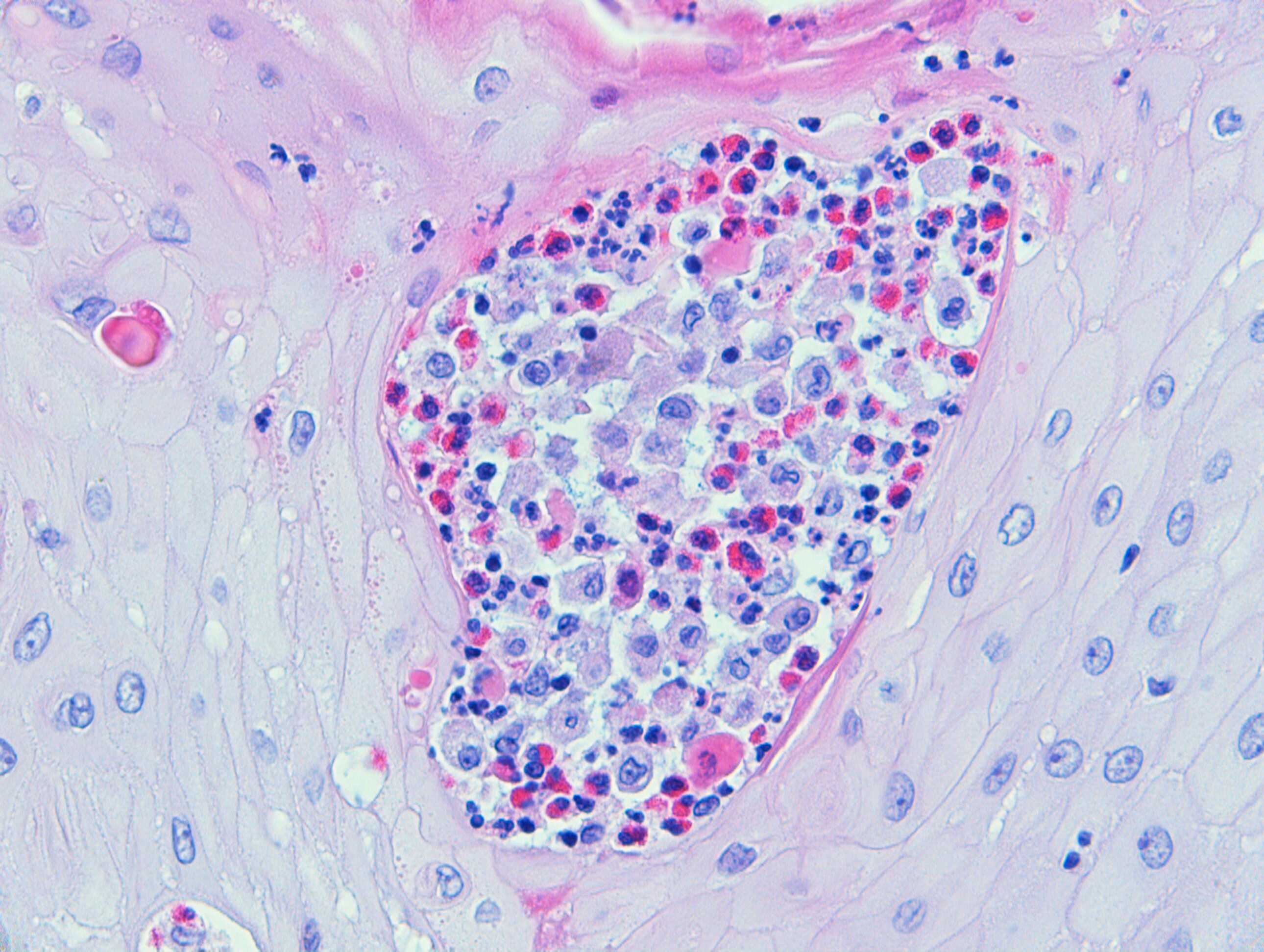
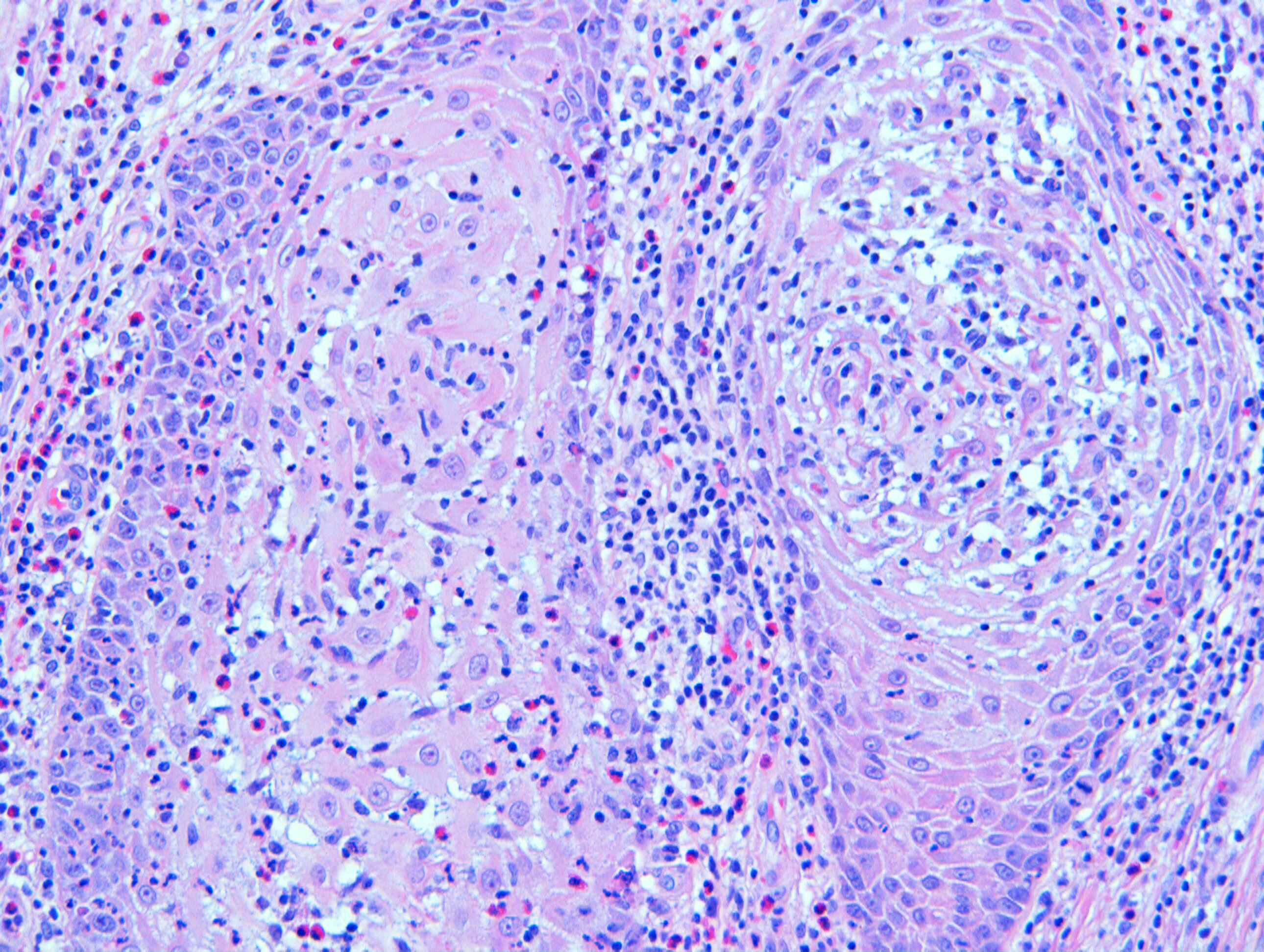
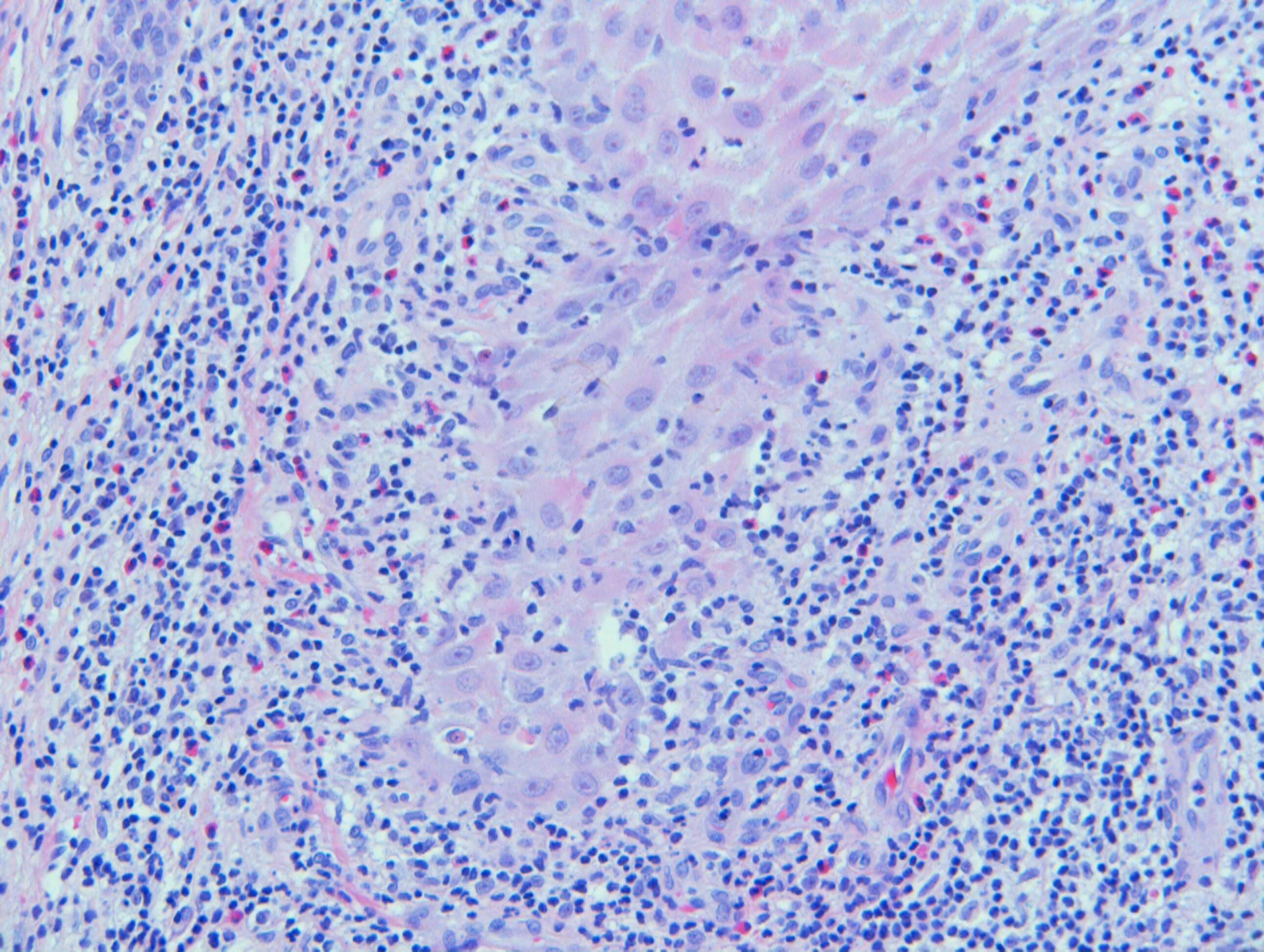
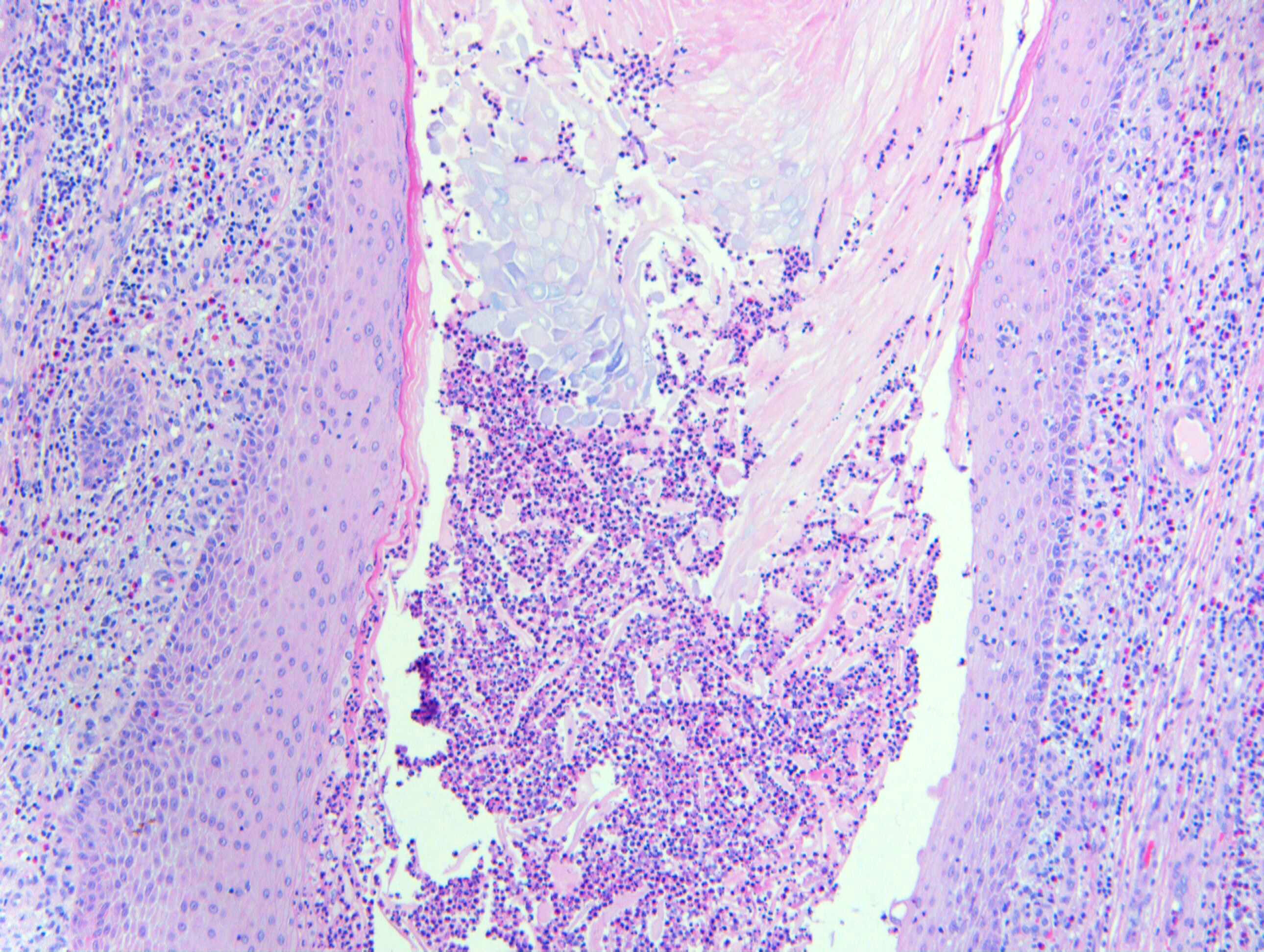
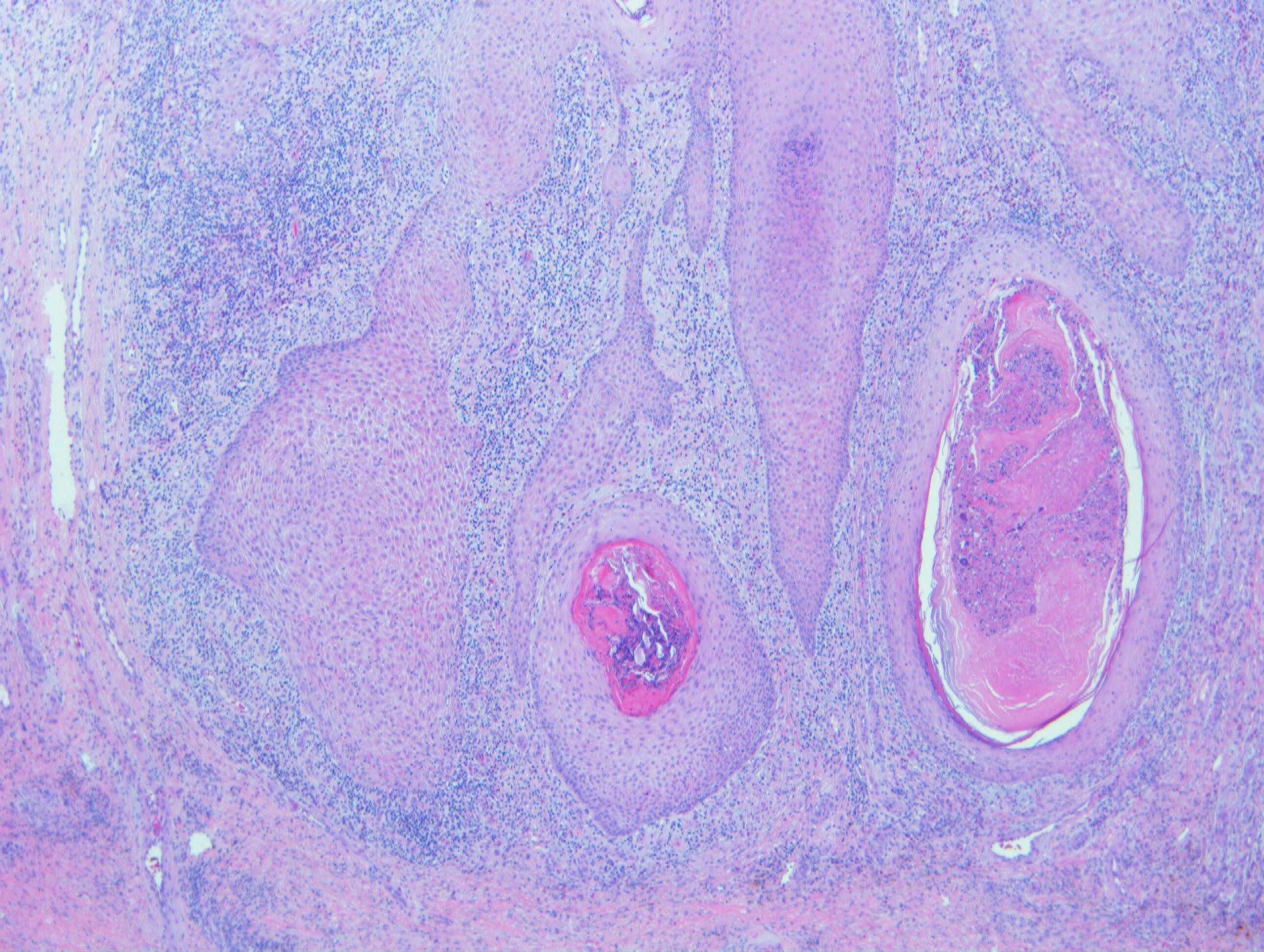
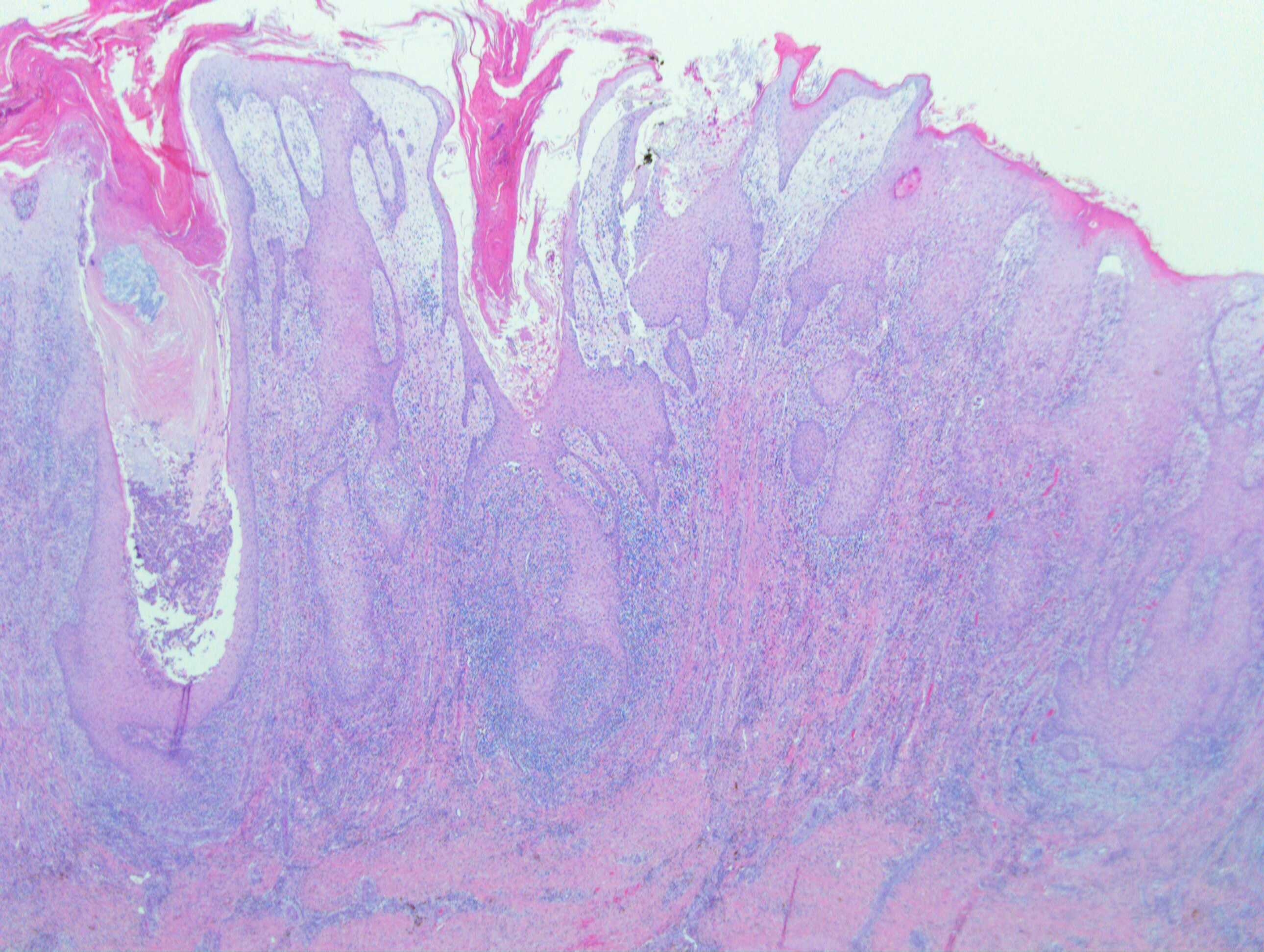
Case Number : Case 2440 - 8 November 2019 Posted By: Dr. Richard Carr
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
M65. 6/52 hx of multiple warty nodules both shins ?reactive squamous hyperplasia ?other



Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.