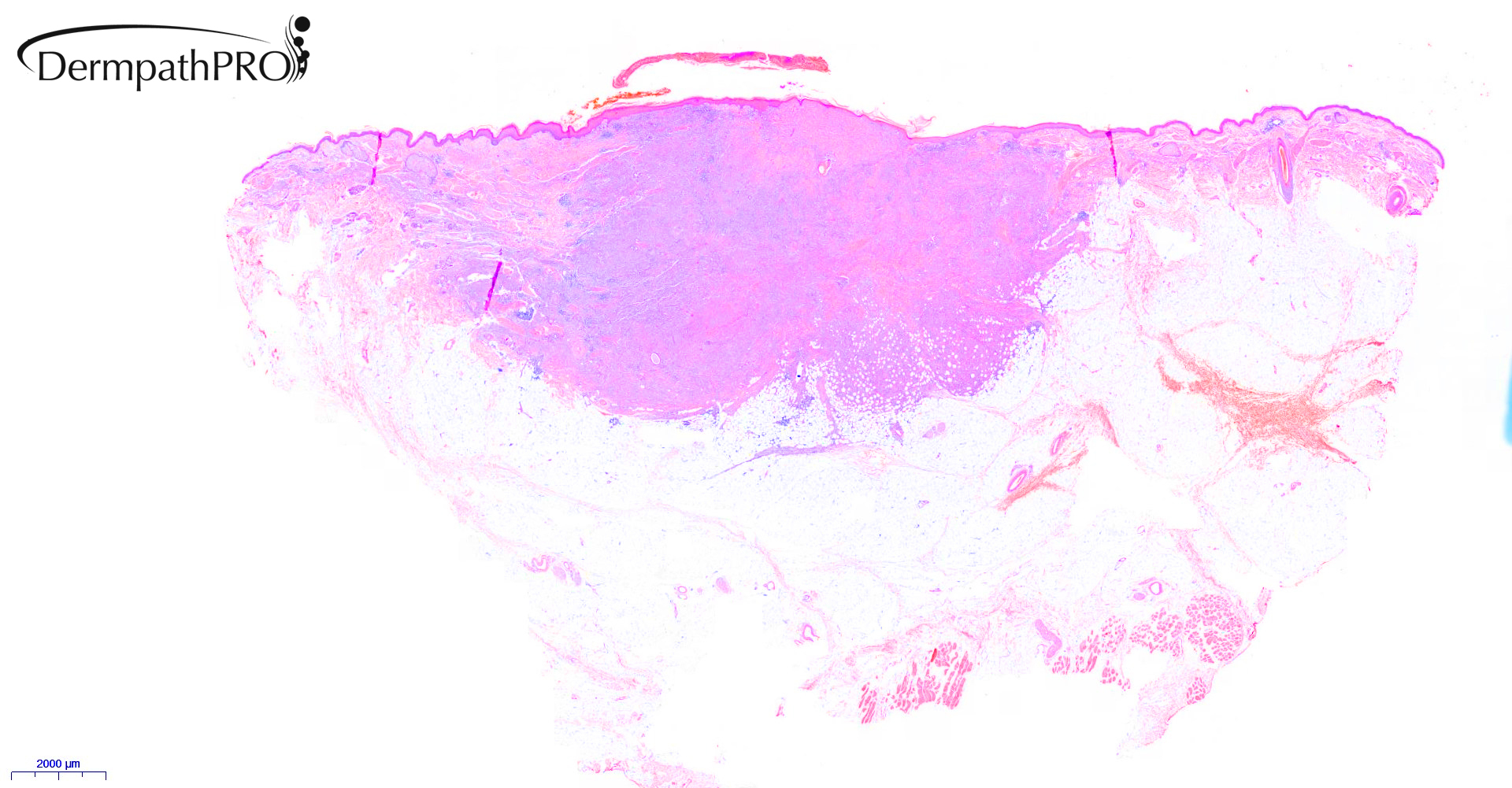
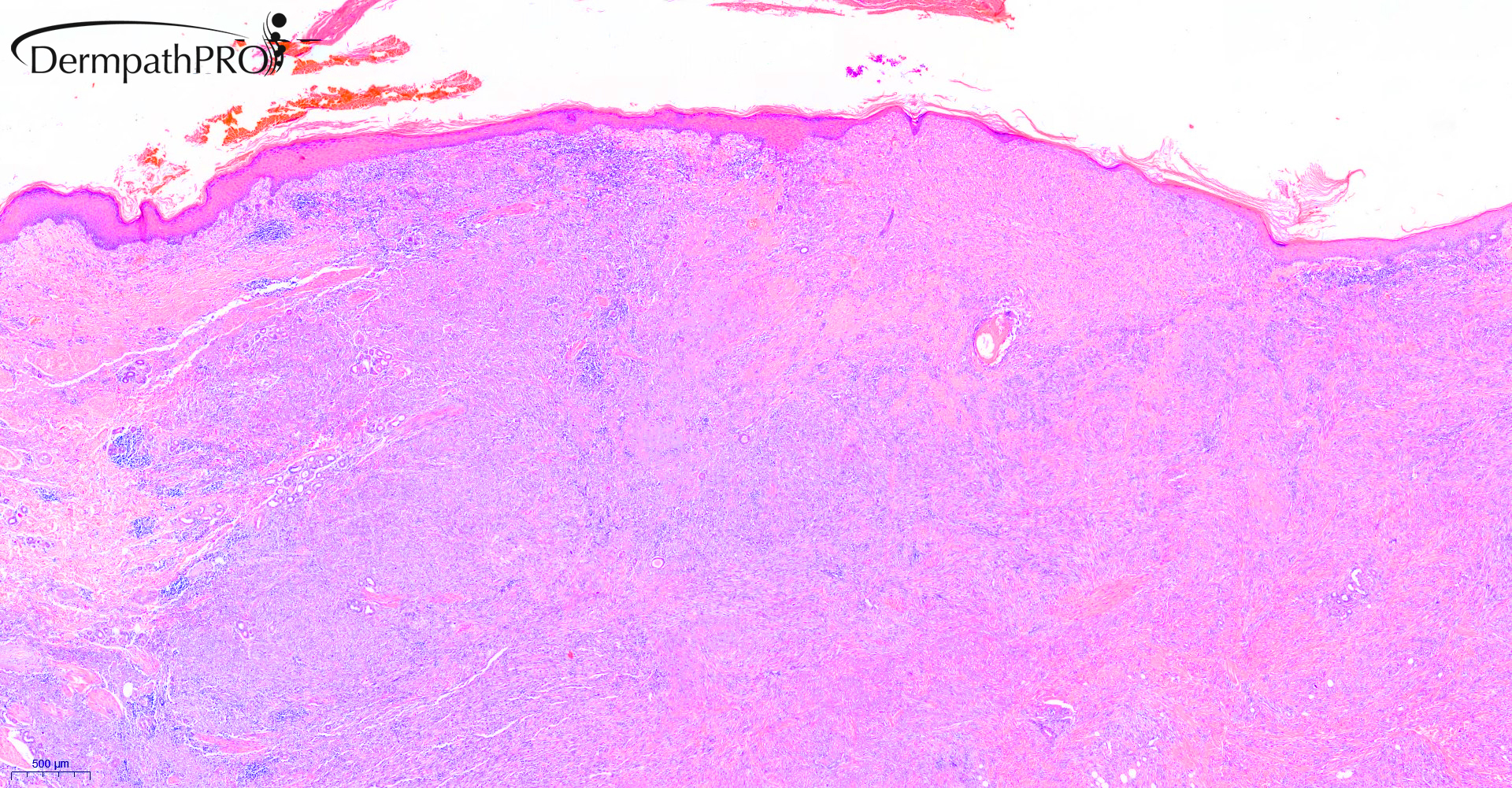
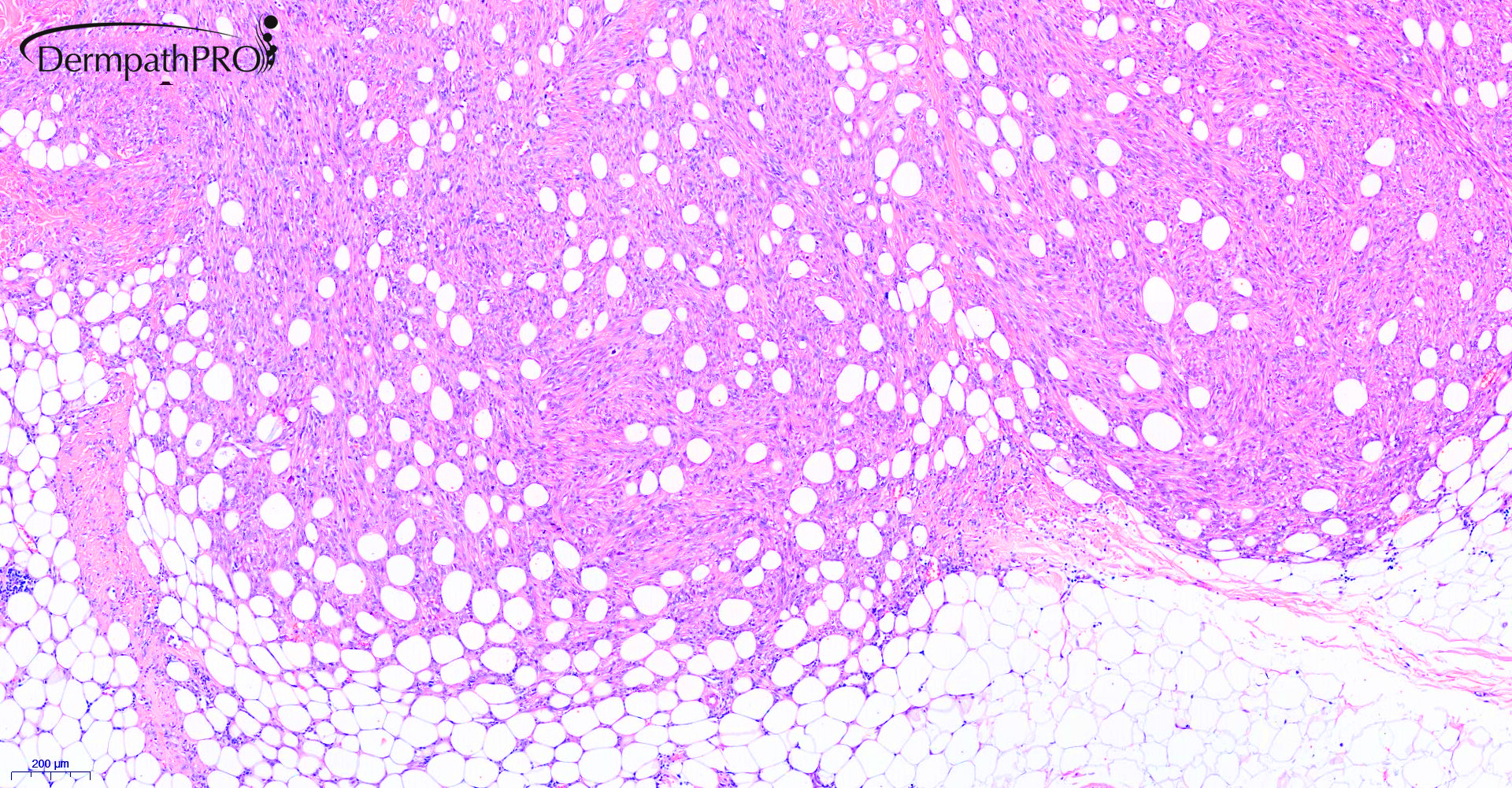
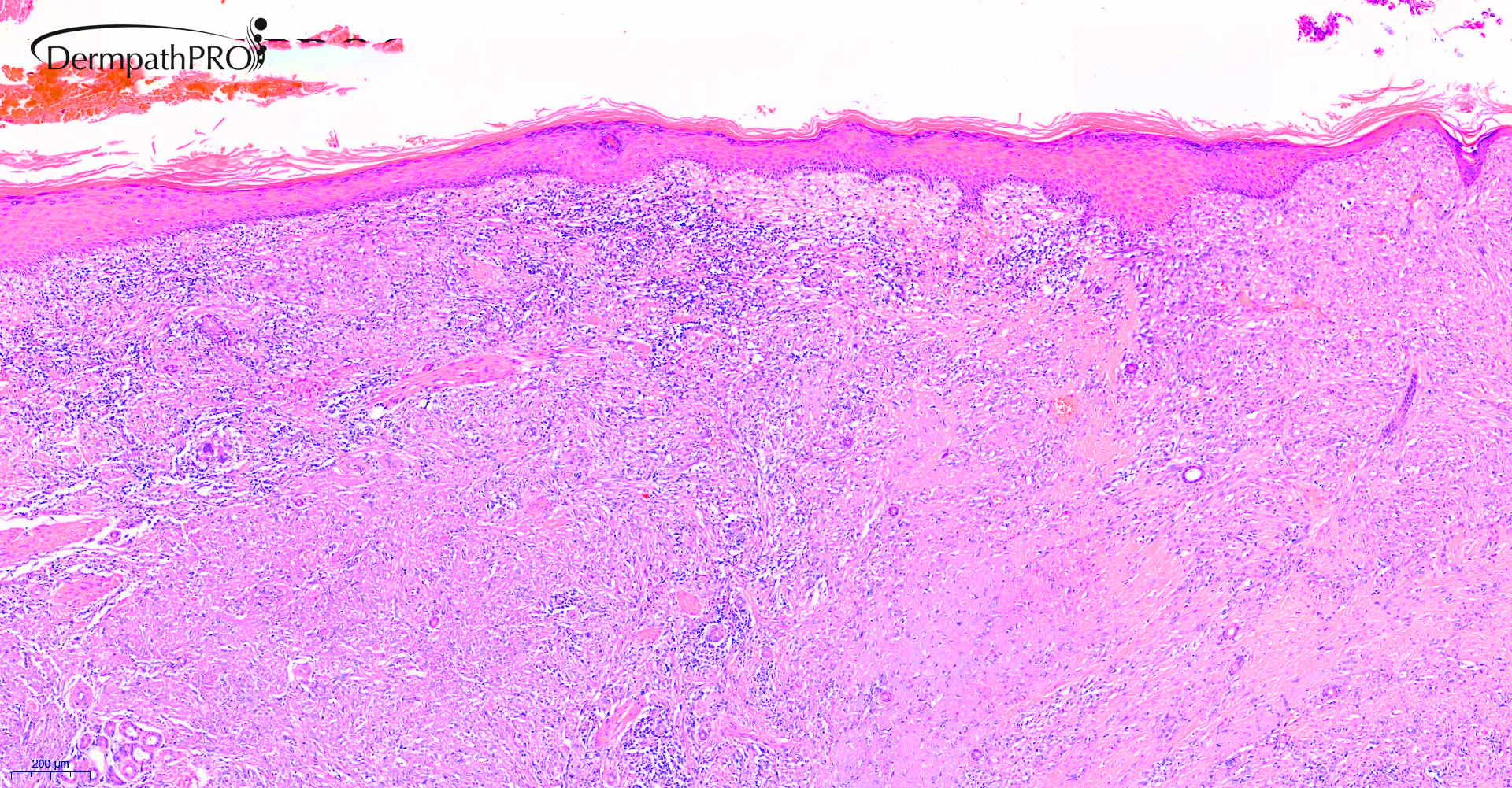
Case Number : Case 2616 - 16 July 2020 Posted By: Saleem Taibjee
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
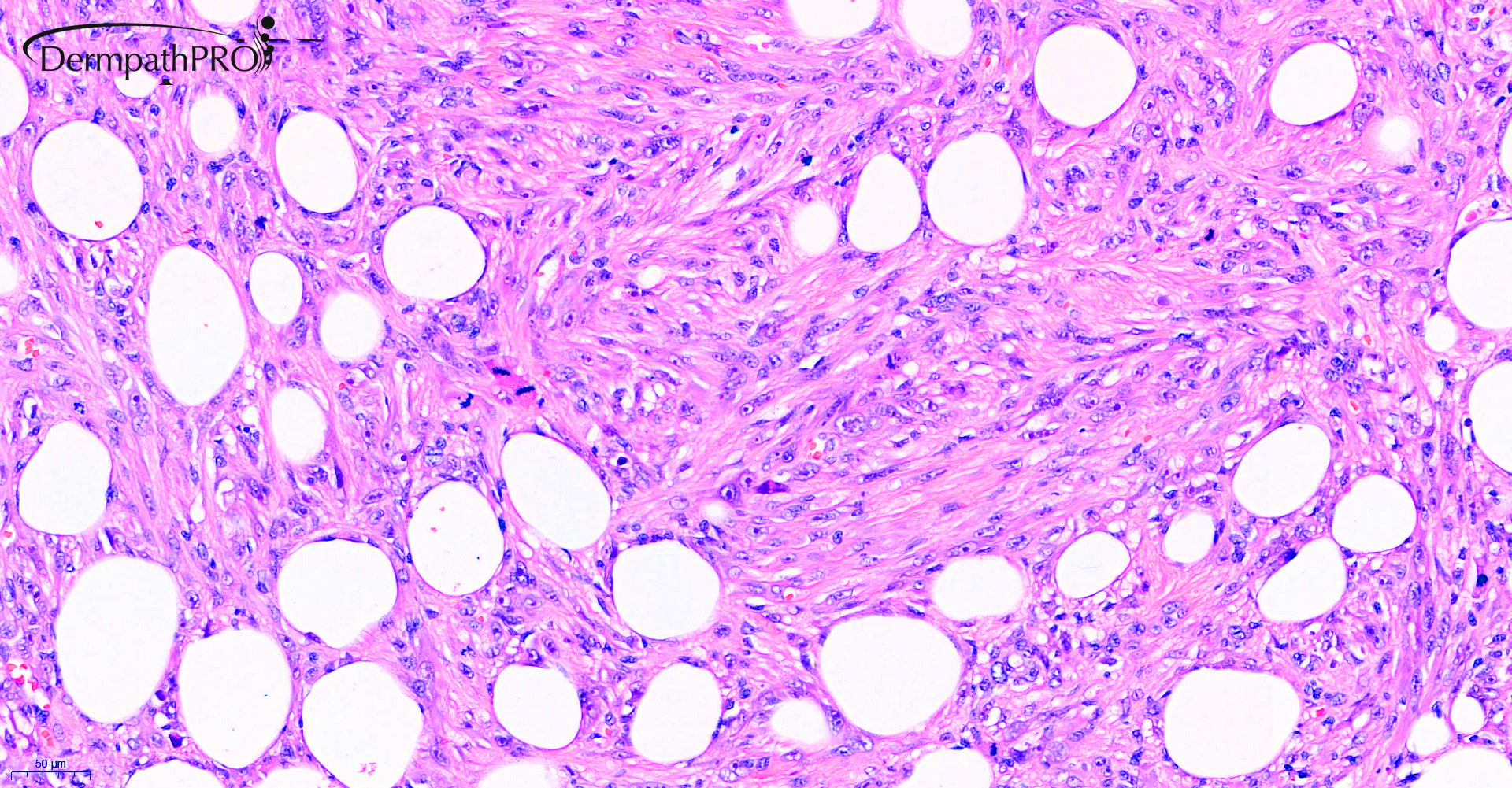
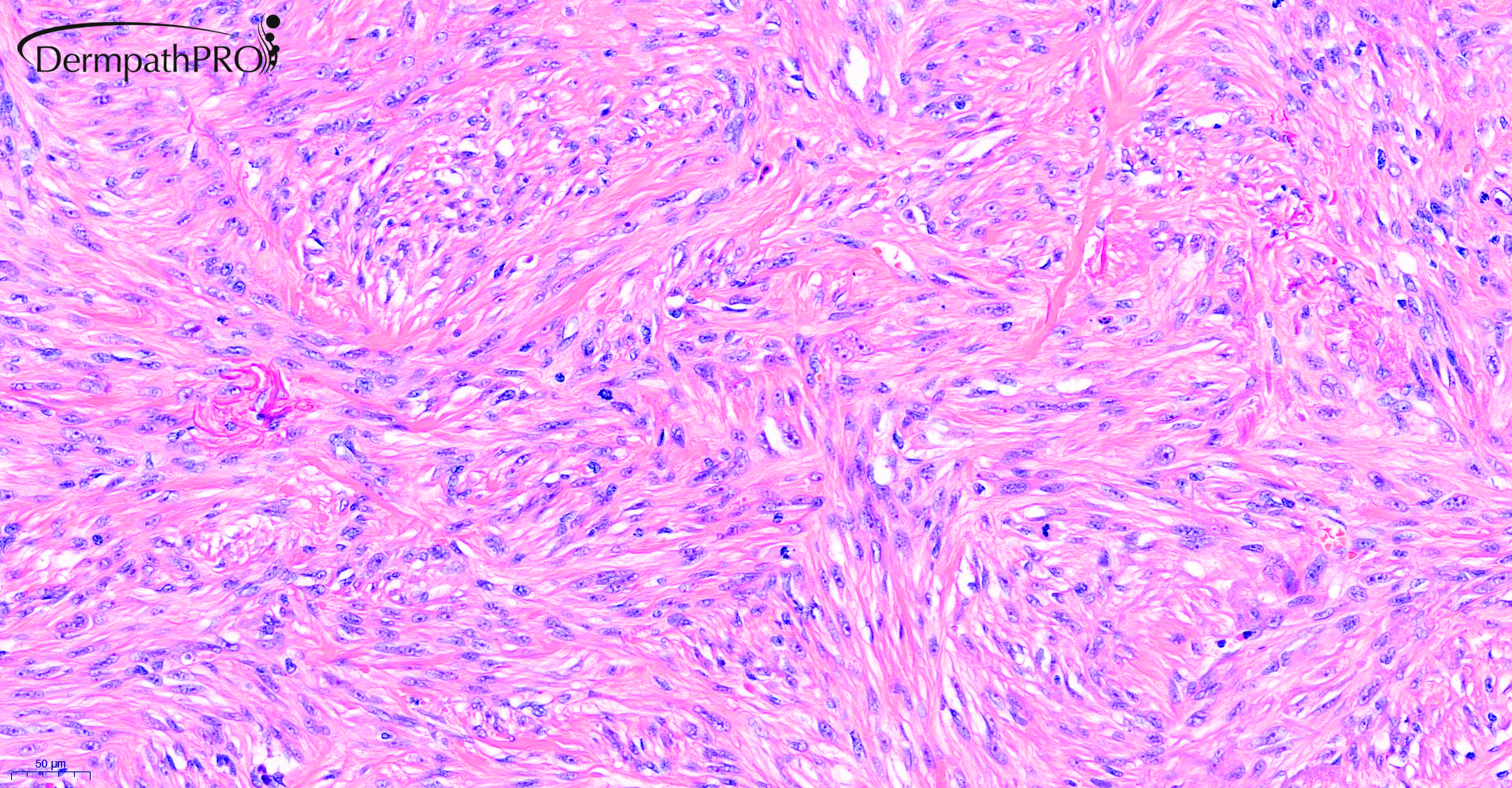
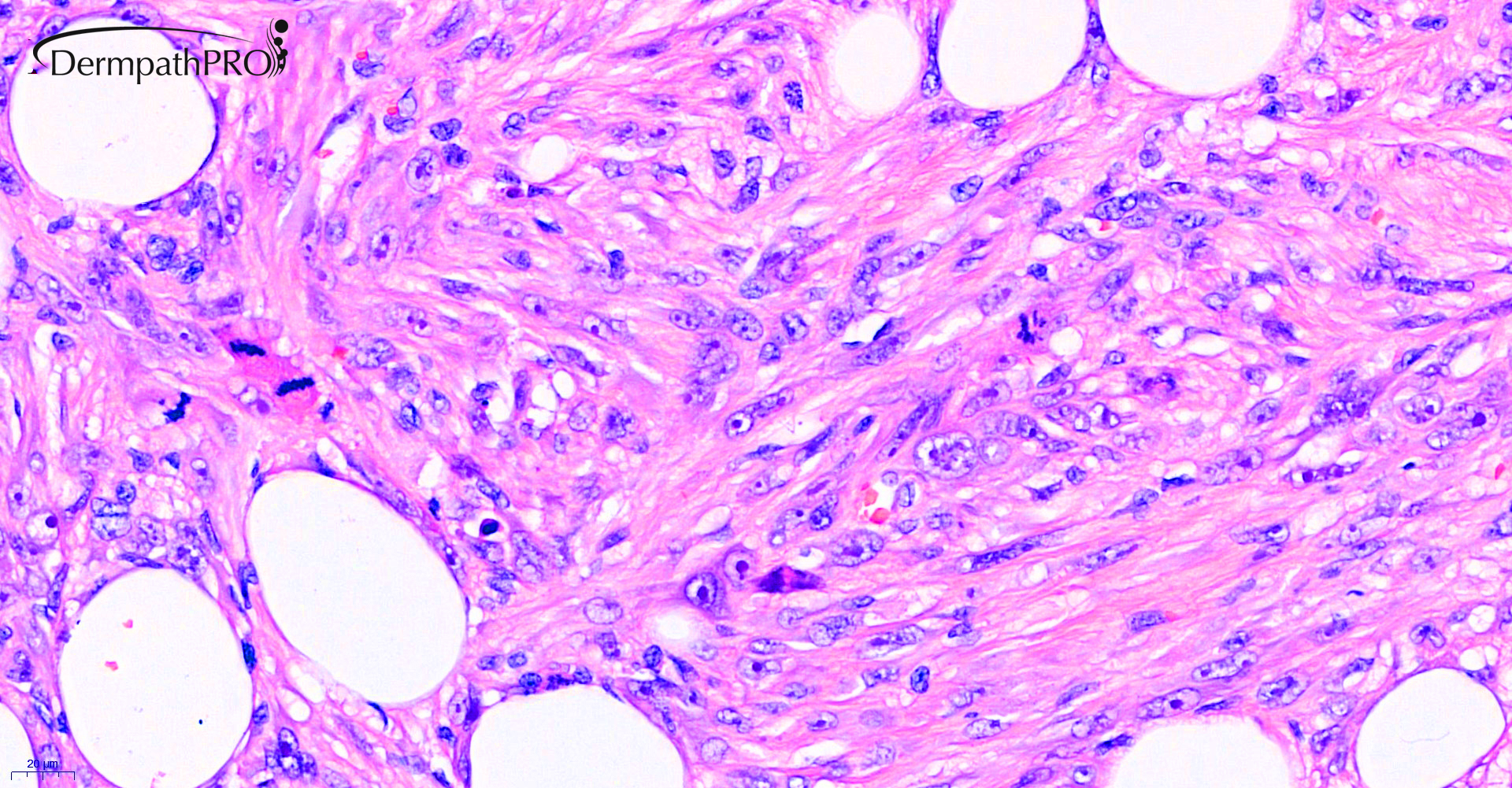
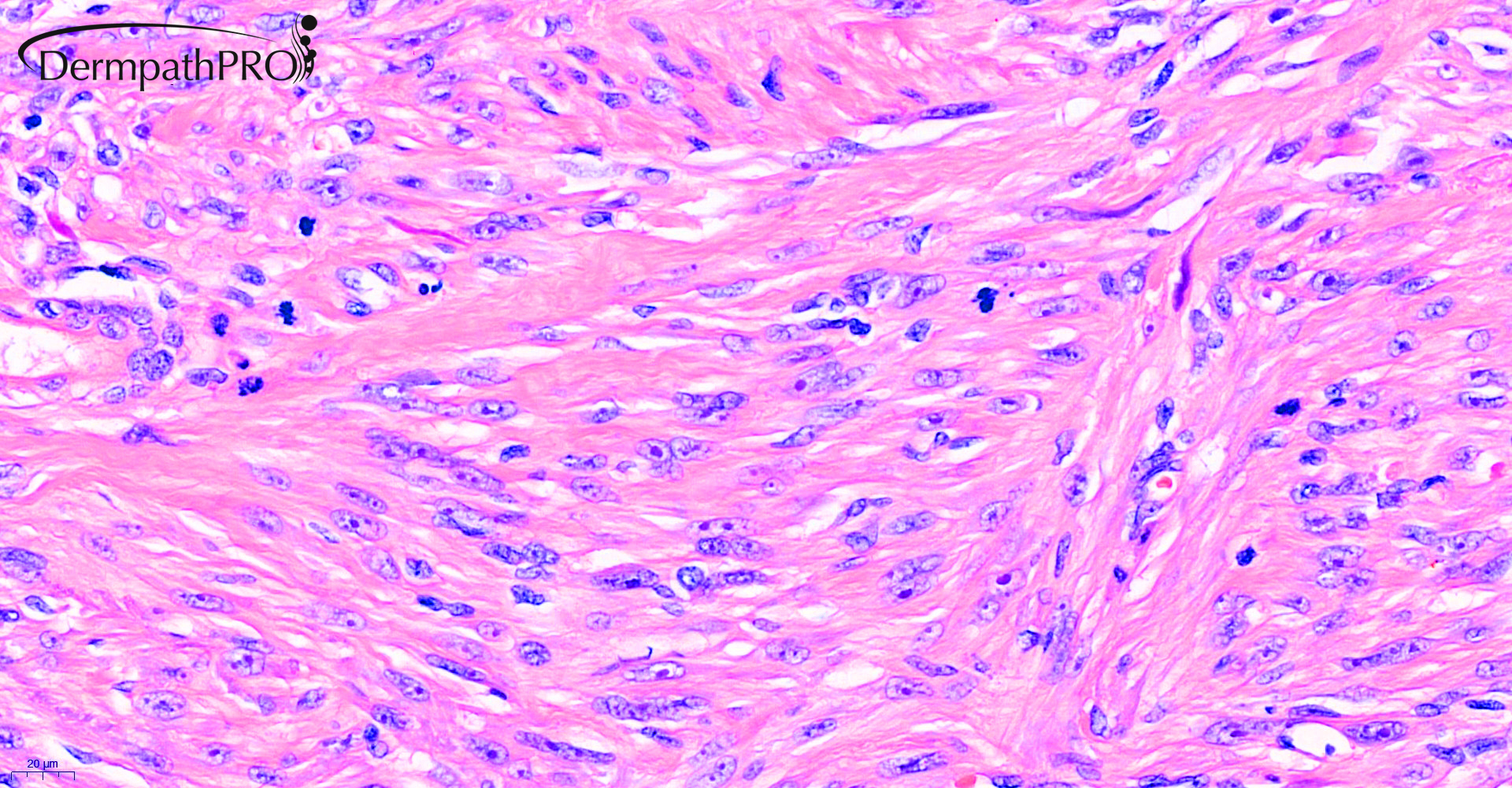
85M excision R cheek ?BCC ?SCC



Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.