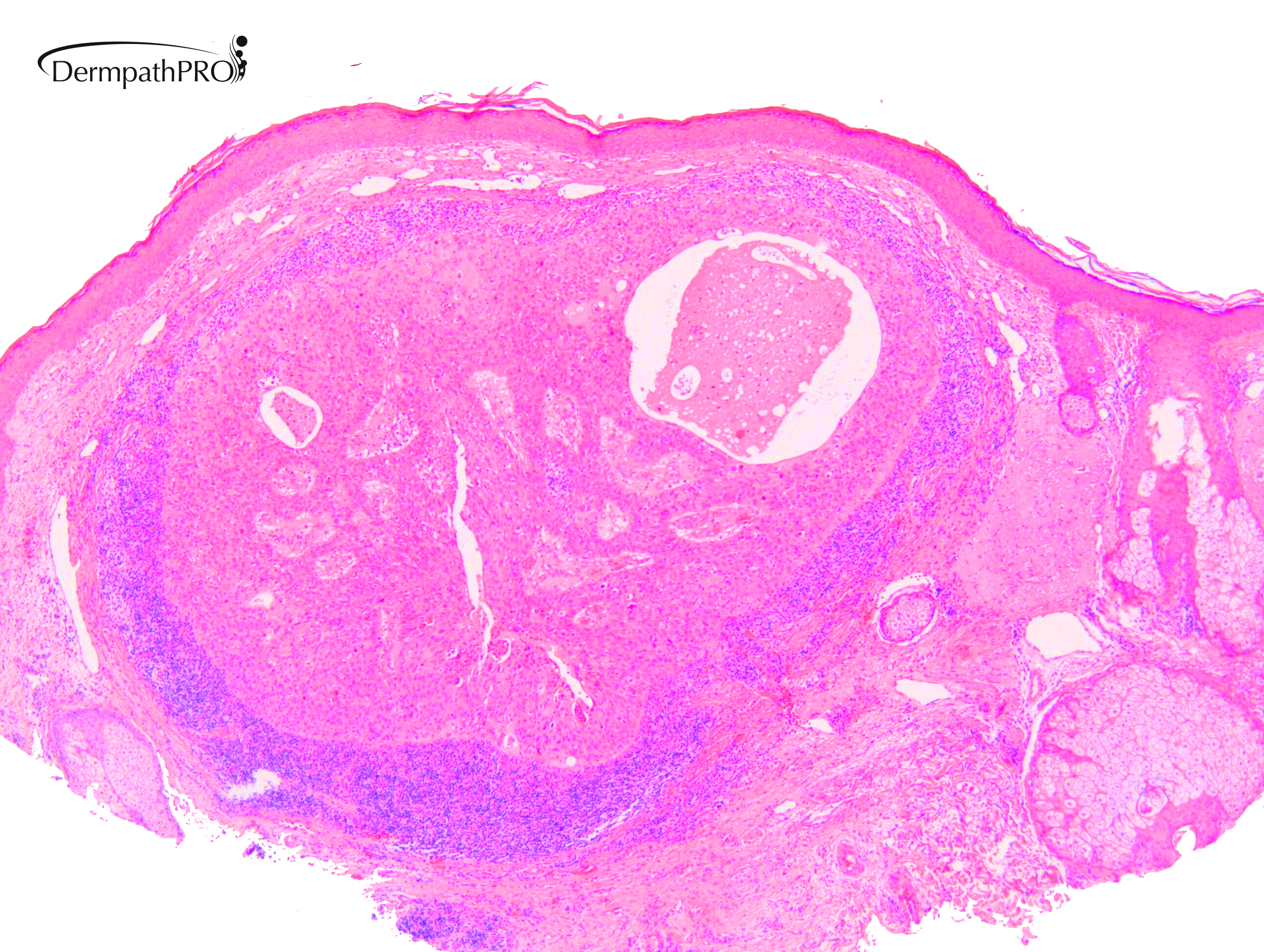
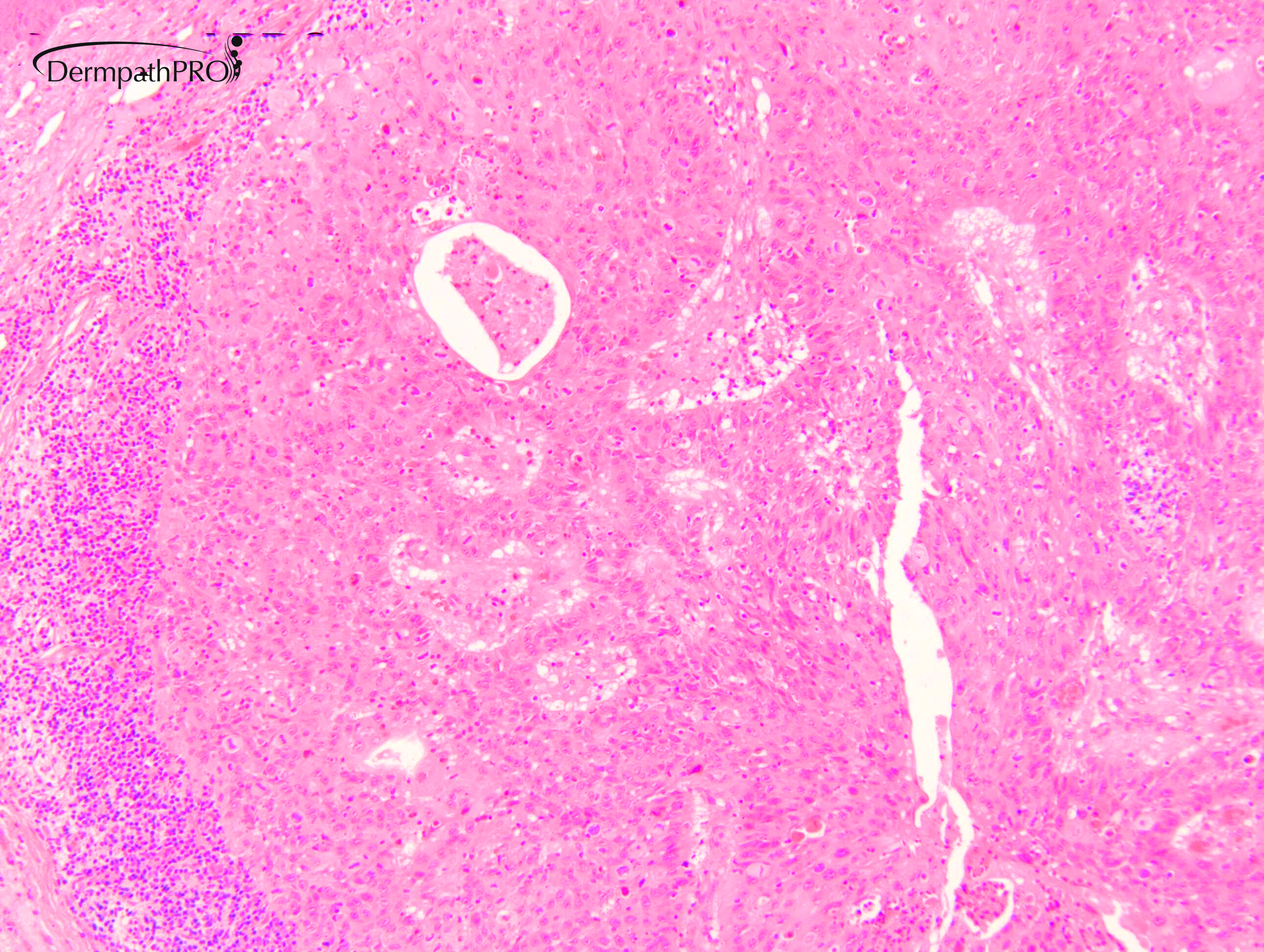
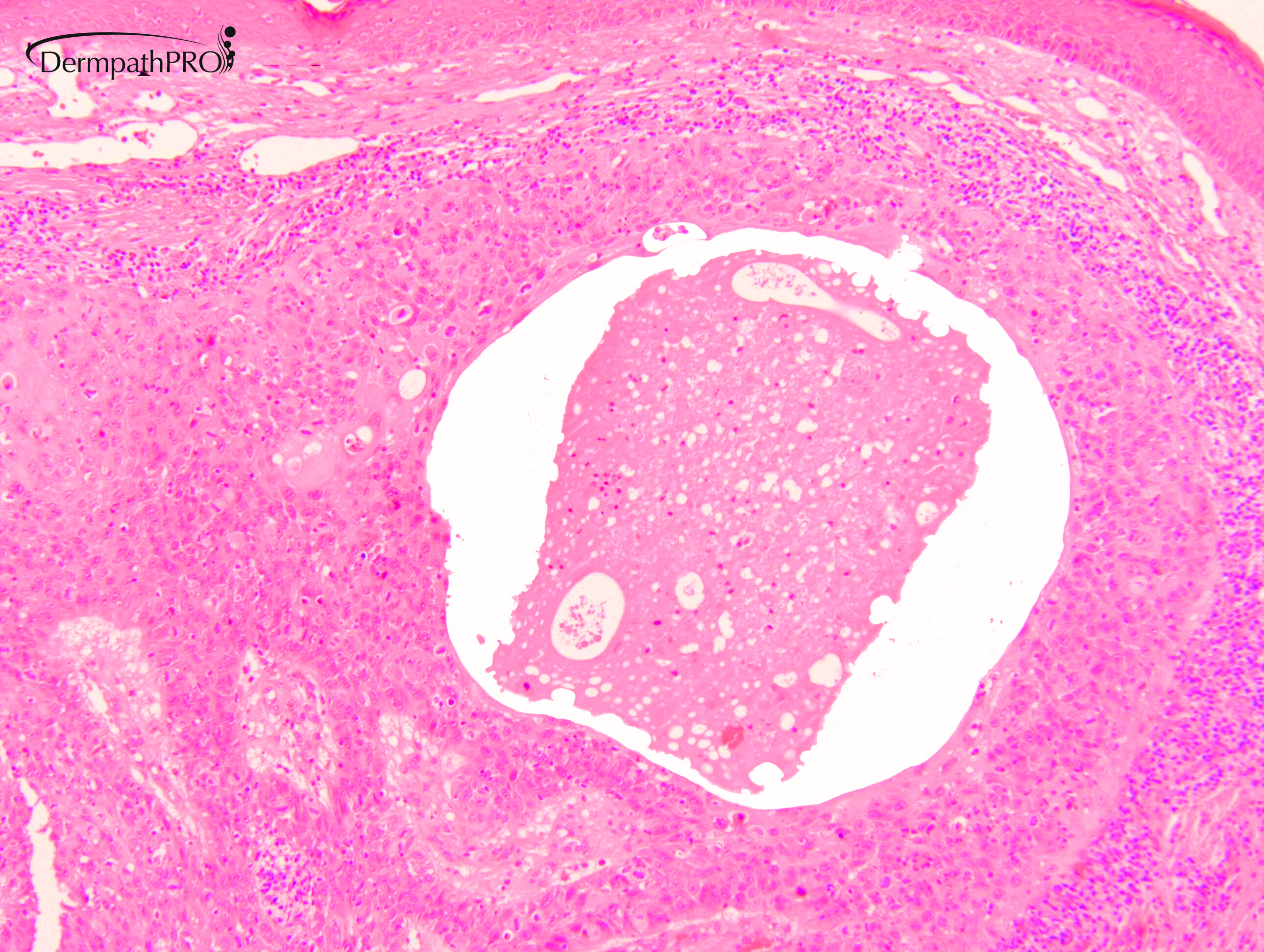
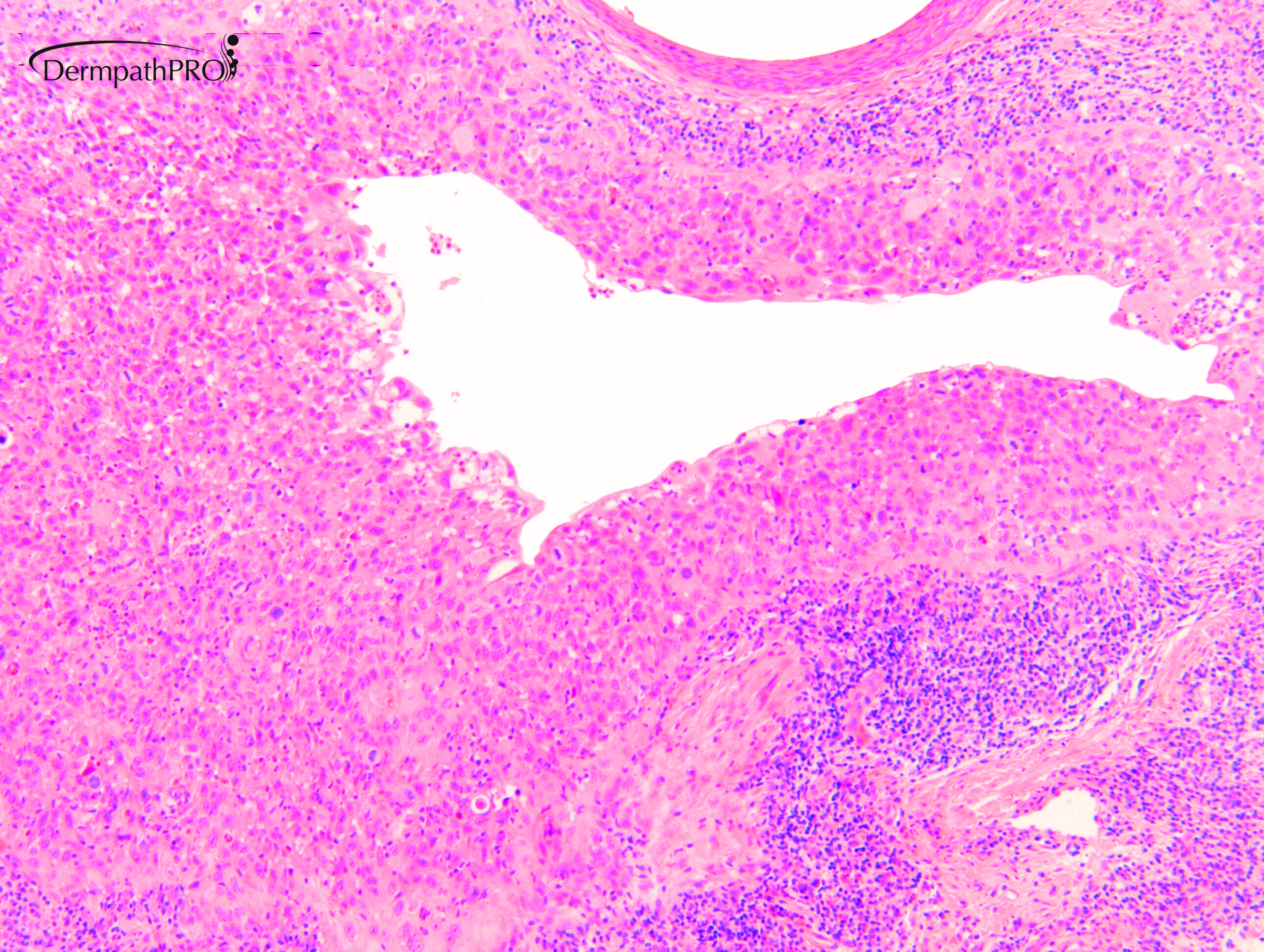
Case Number : Case 2622 - 24 July 2020 Posted By: Dr. Richard Carr
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
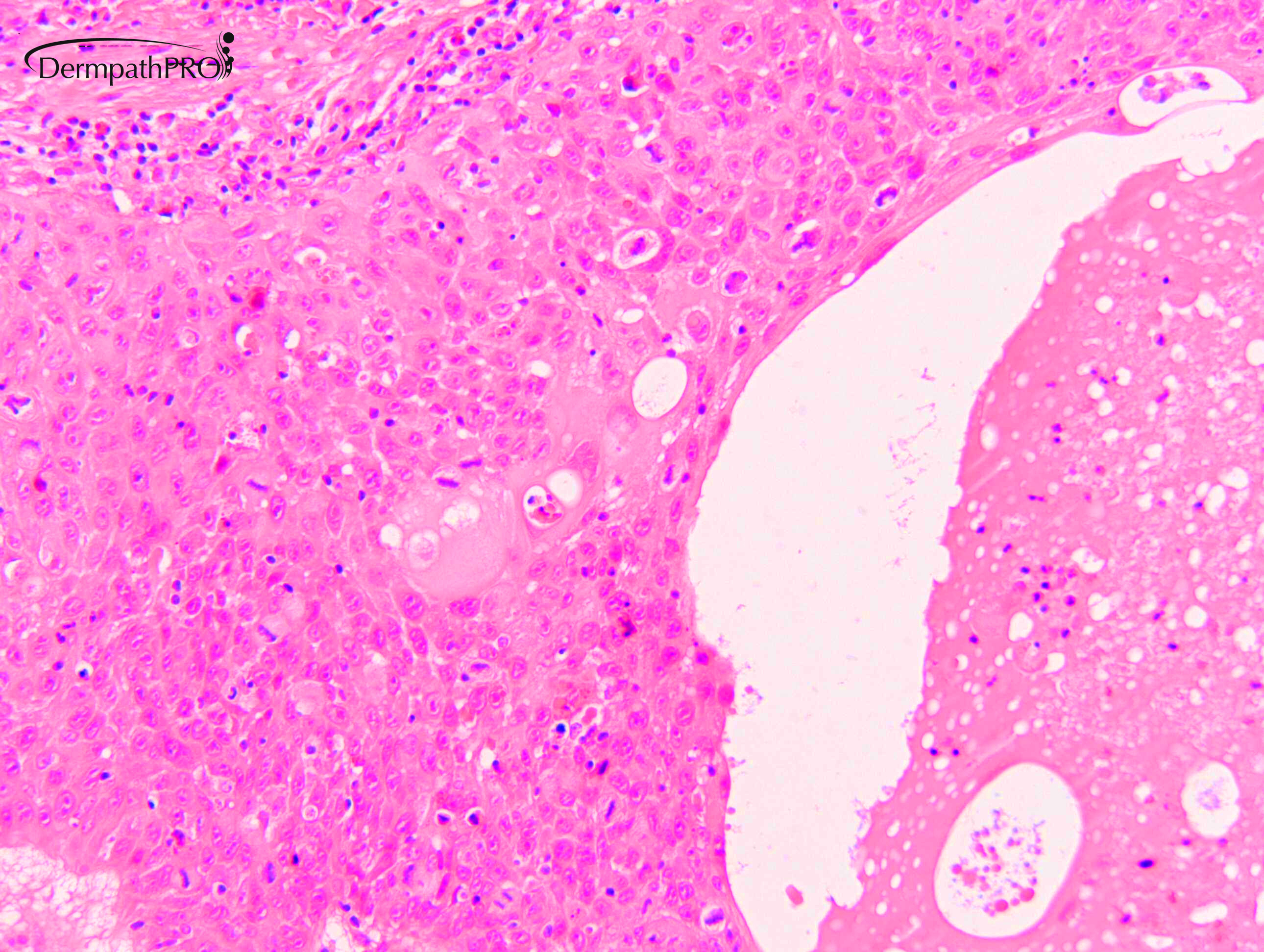
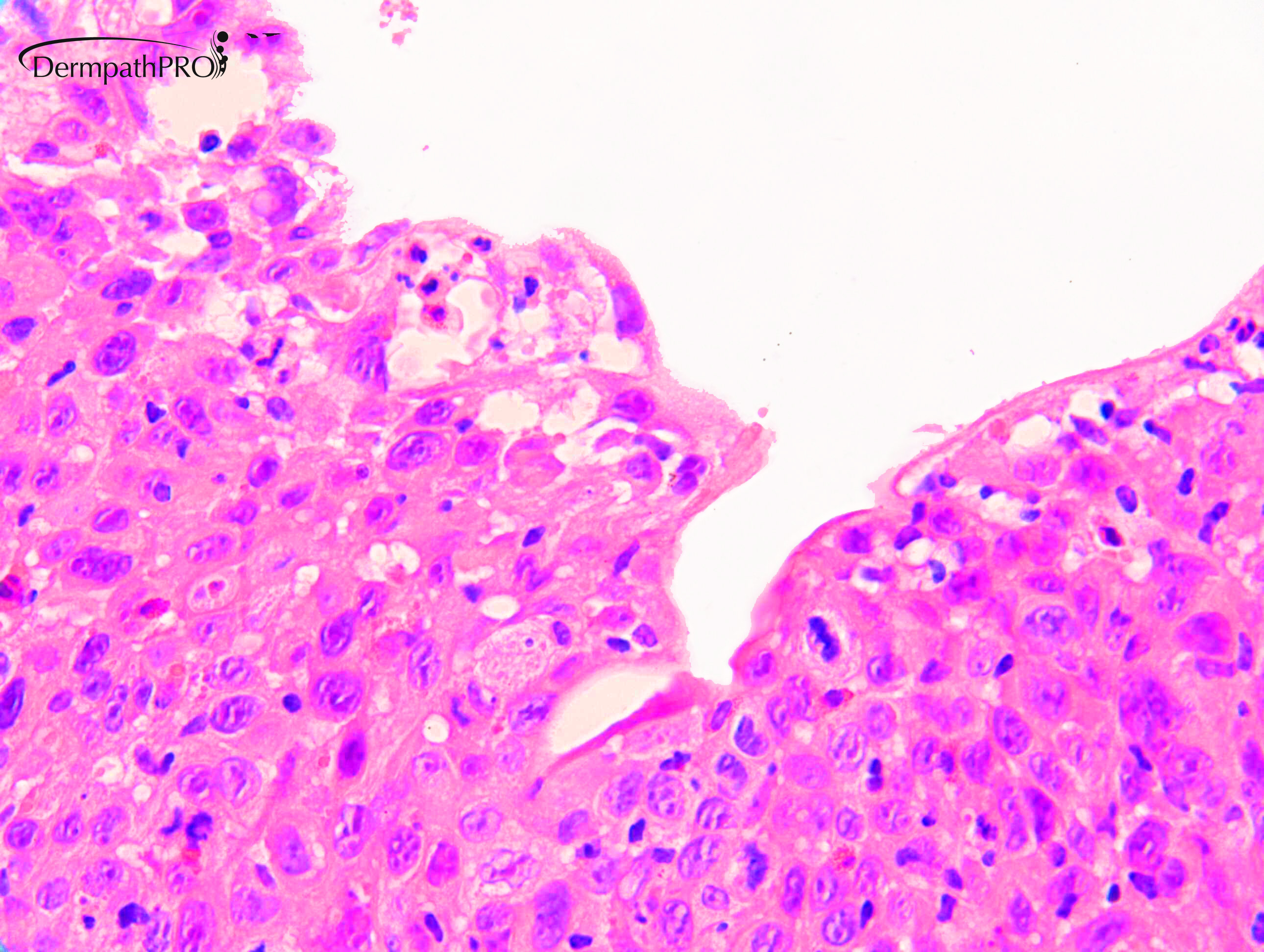
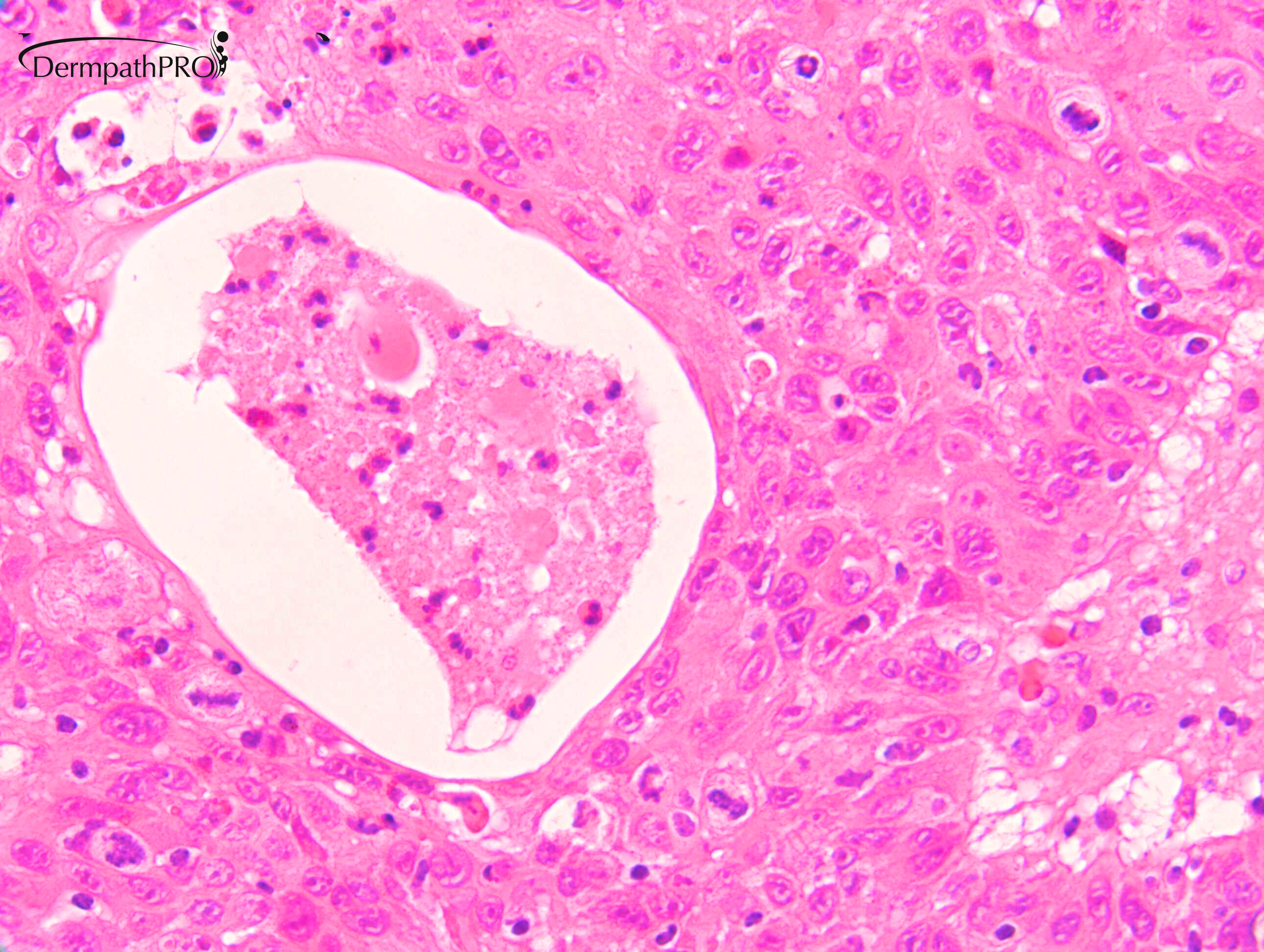
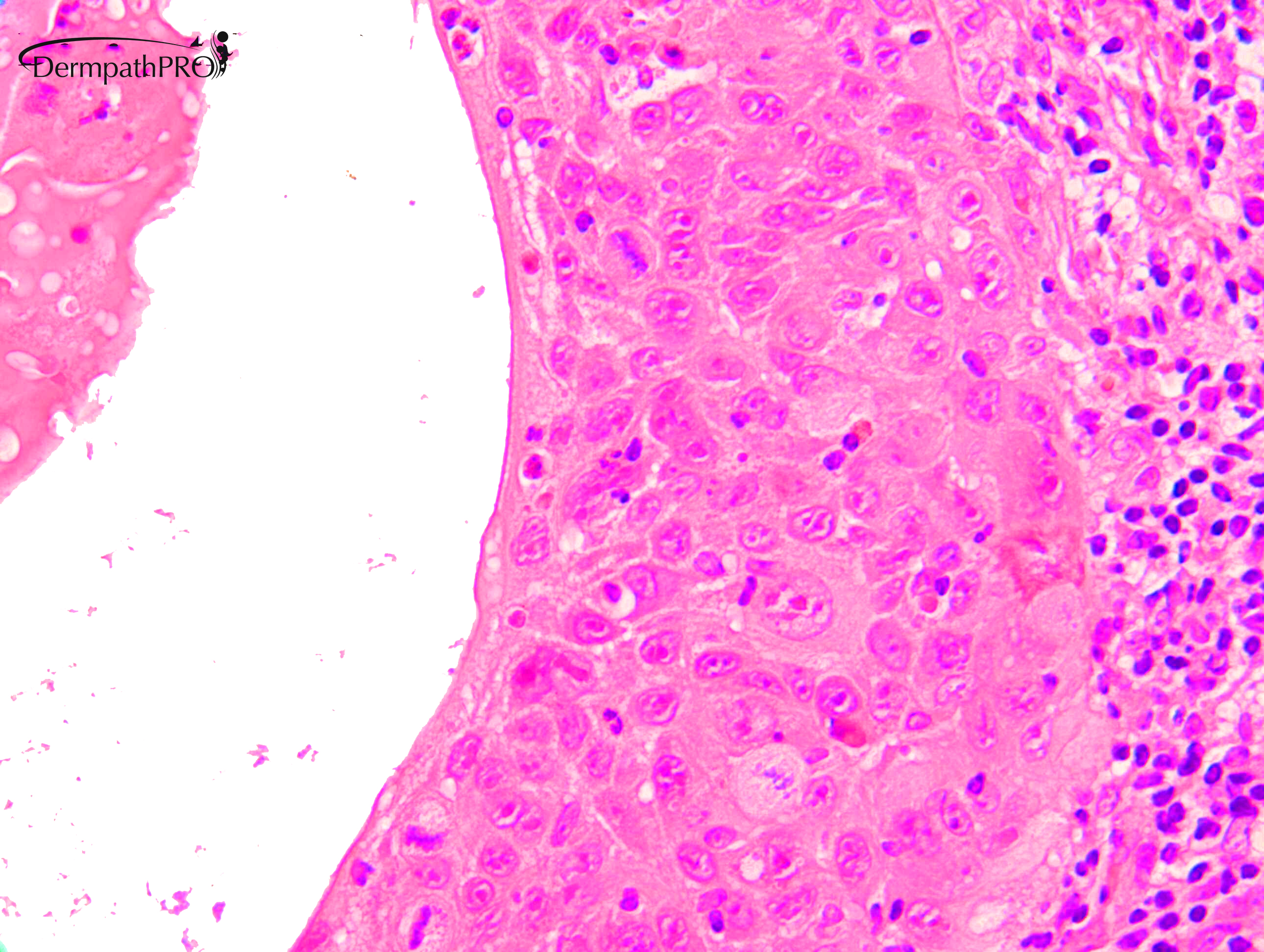
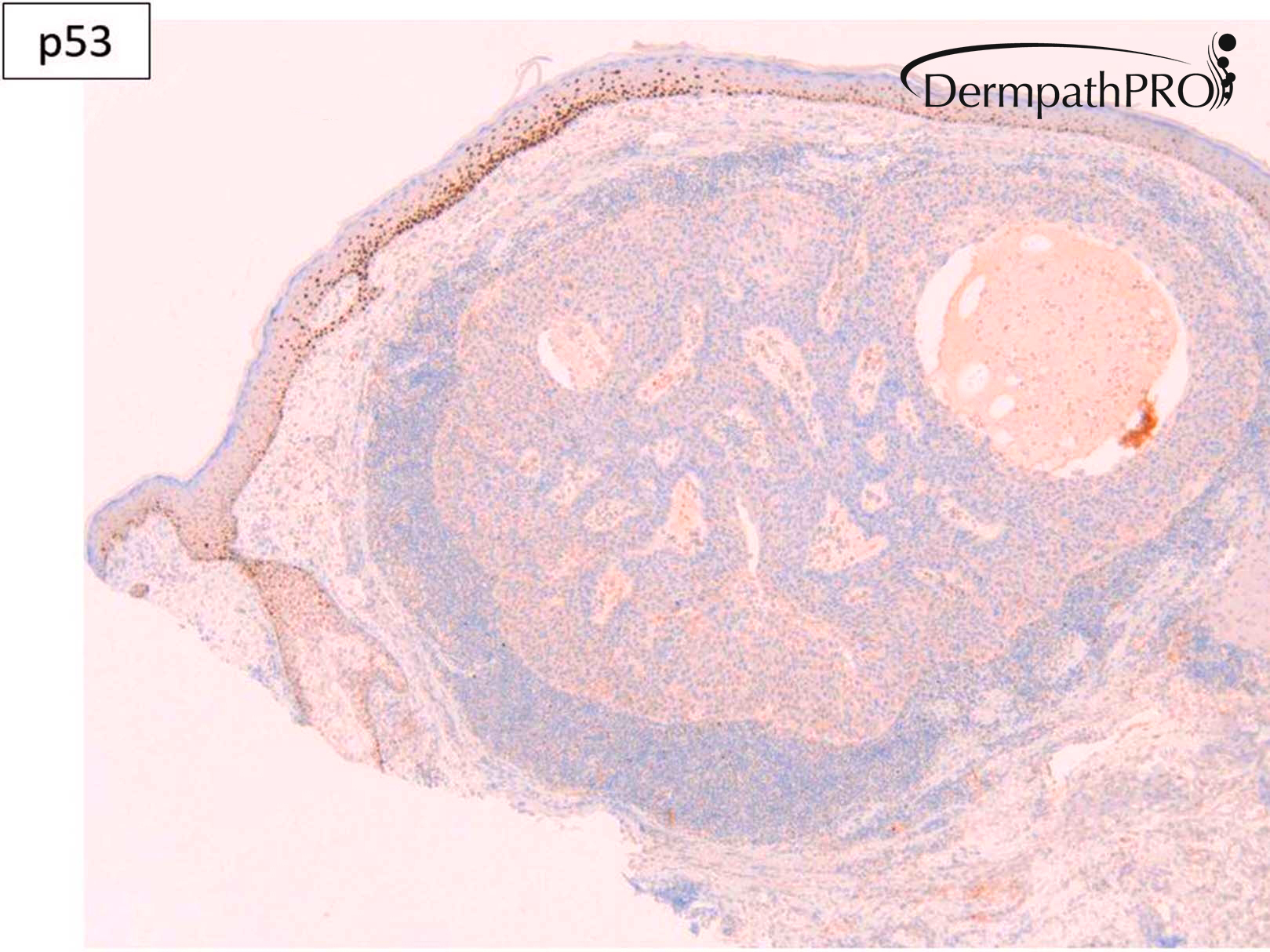
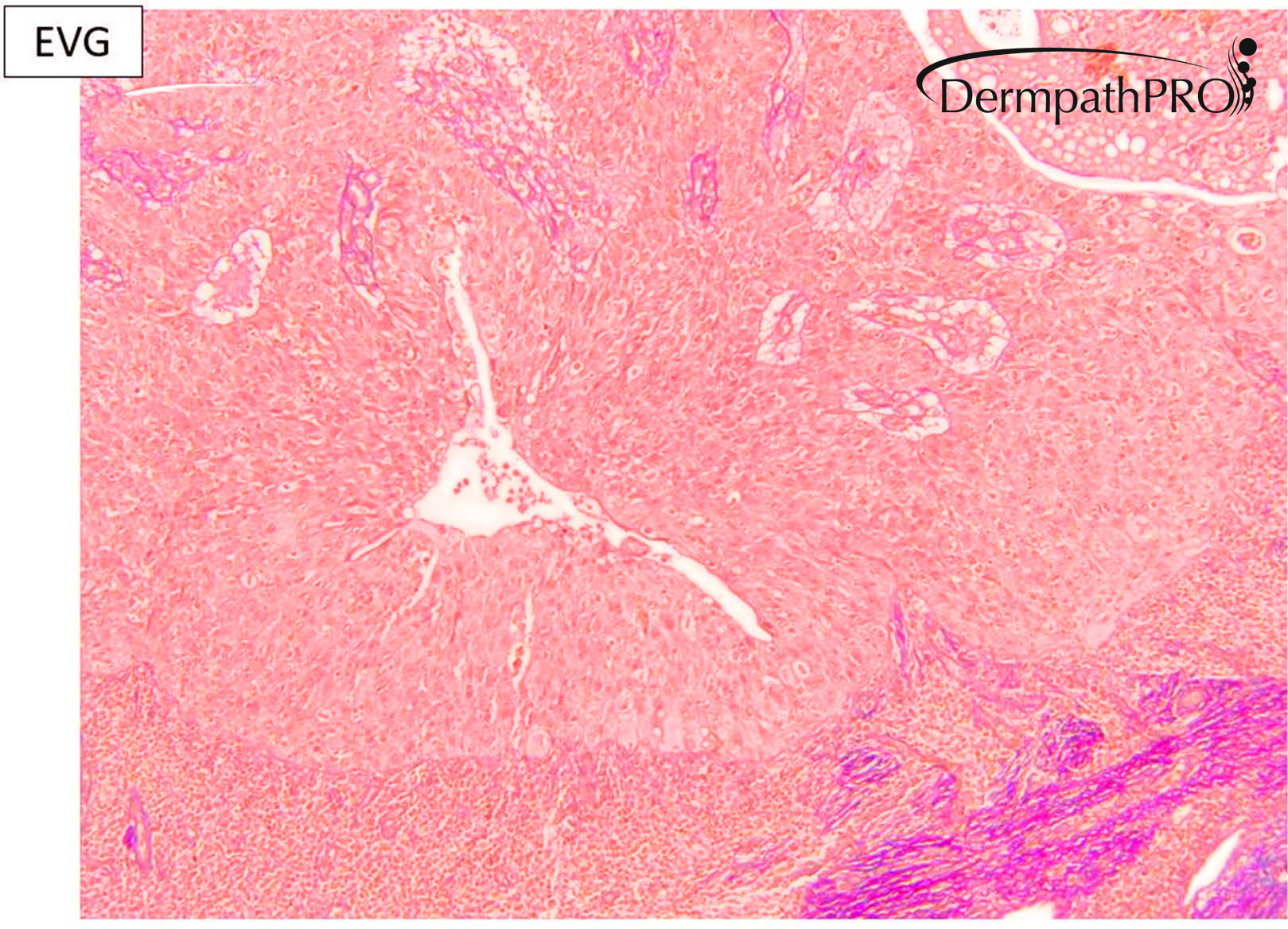
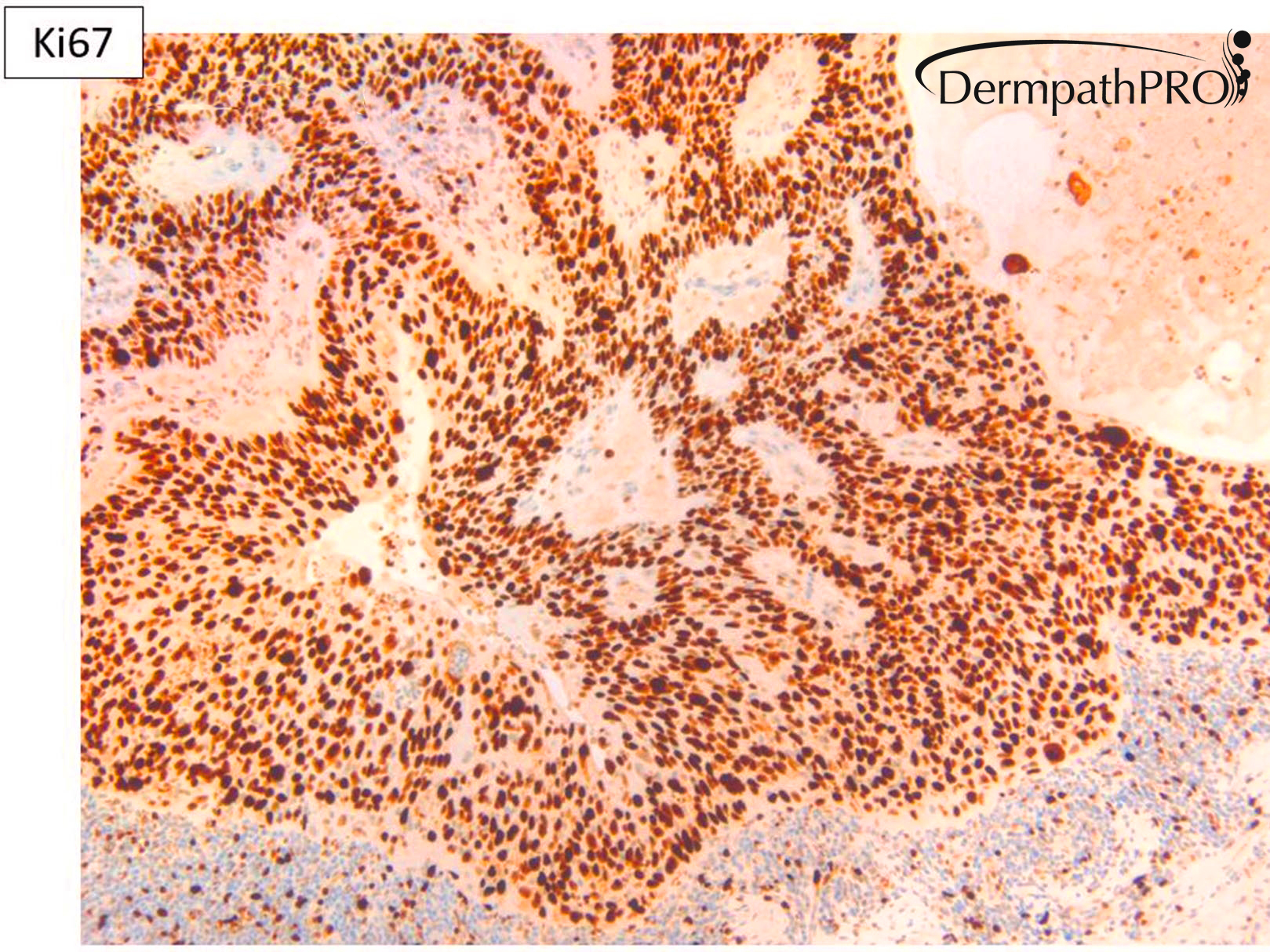
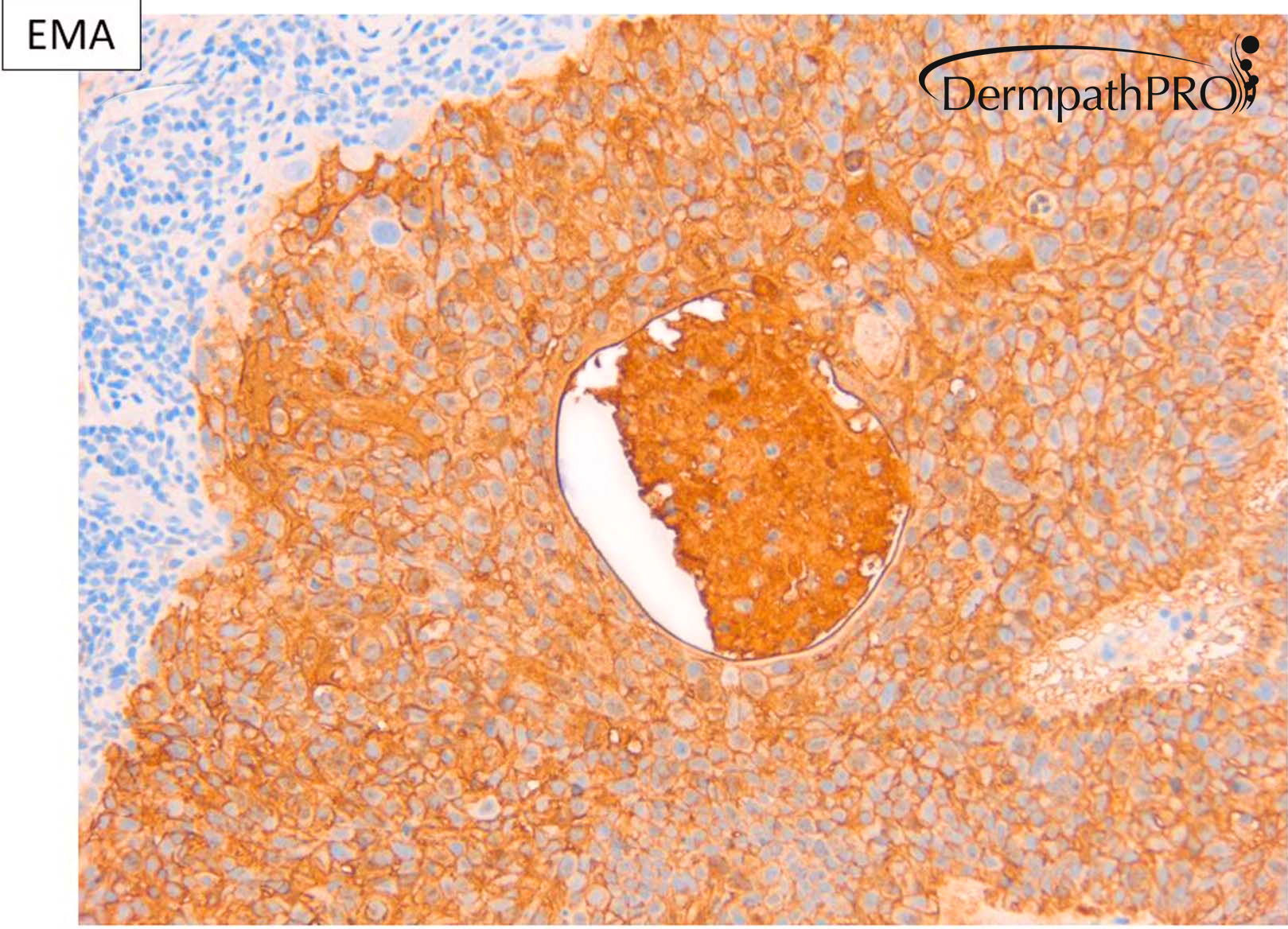
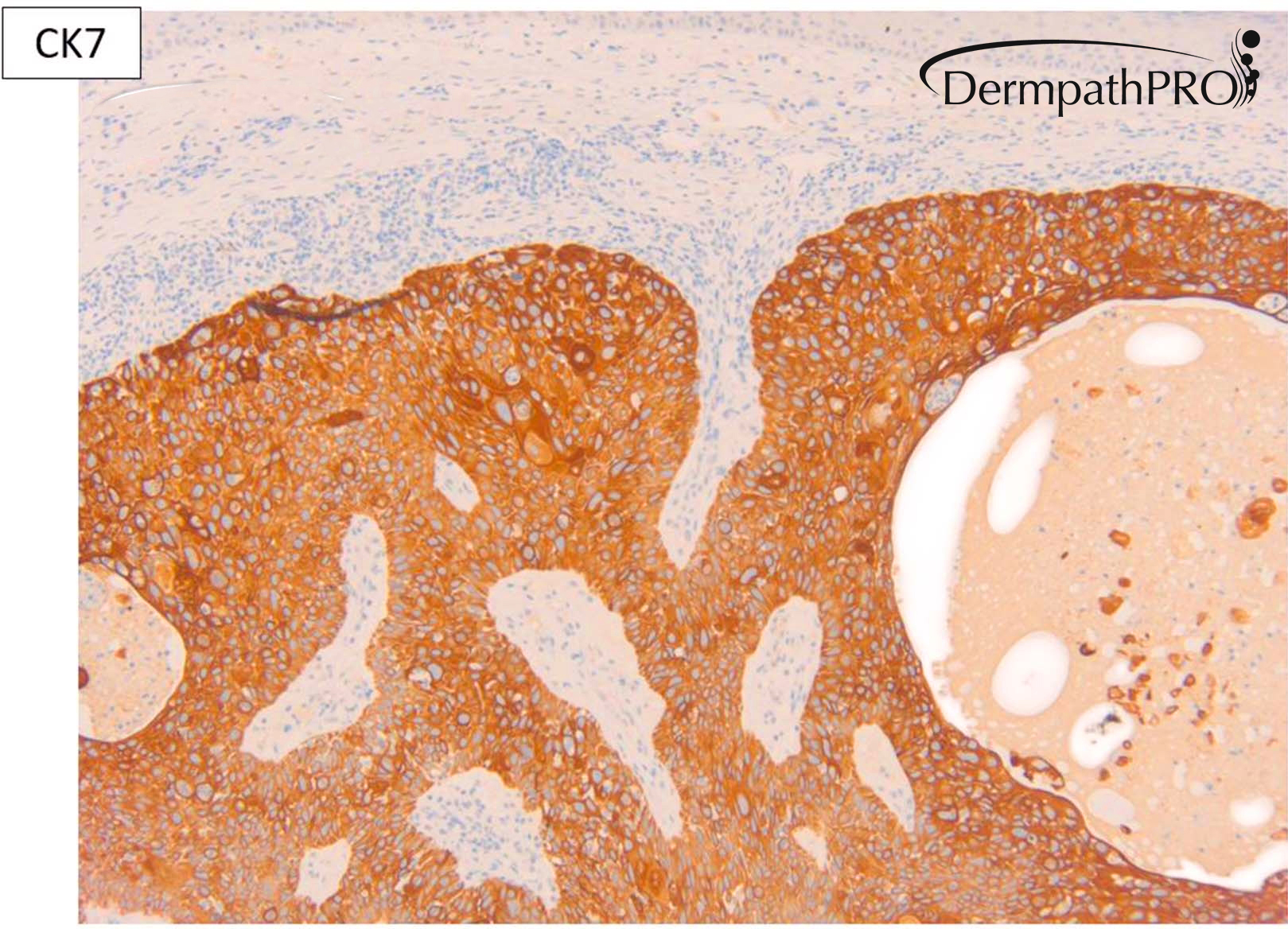
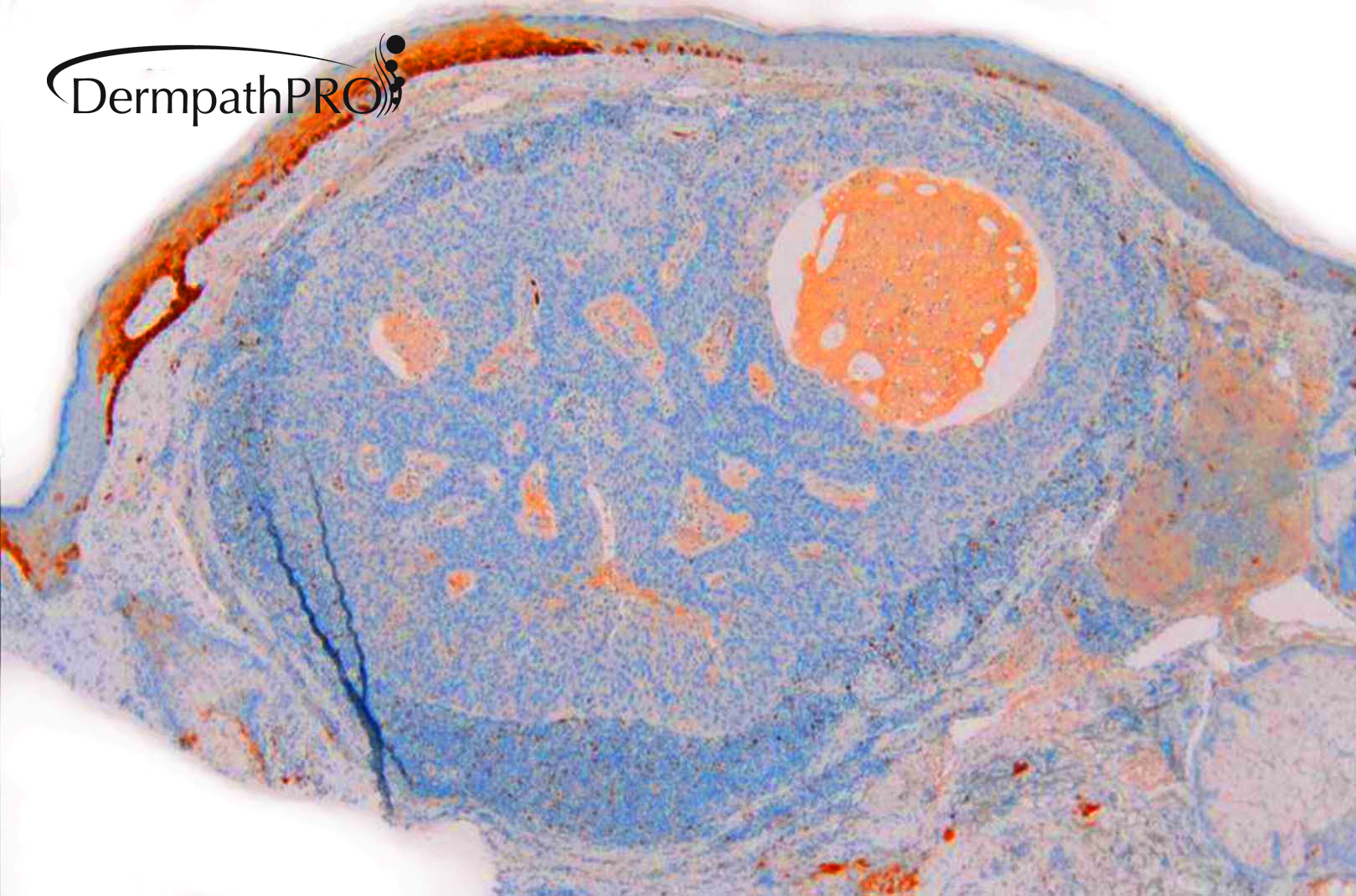
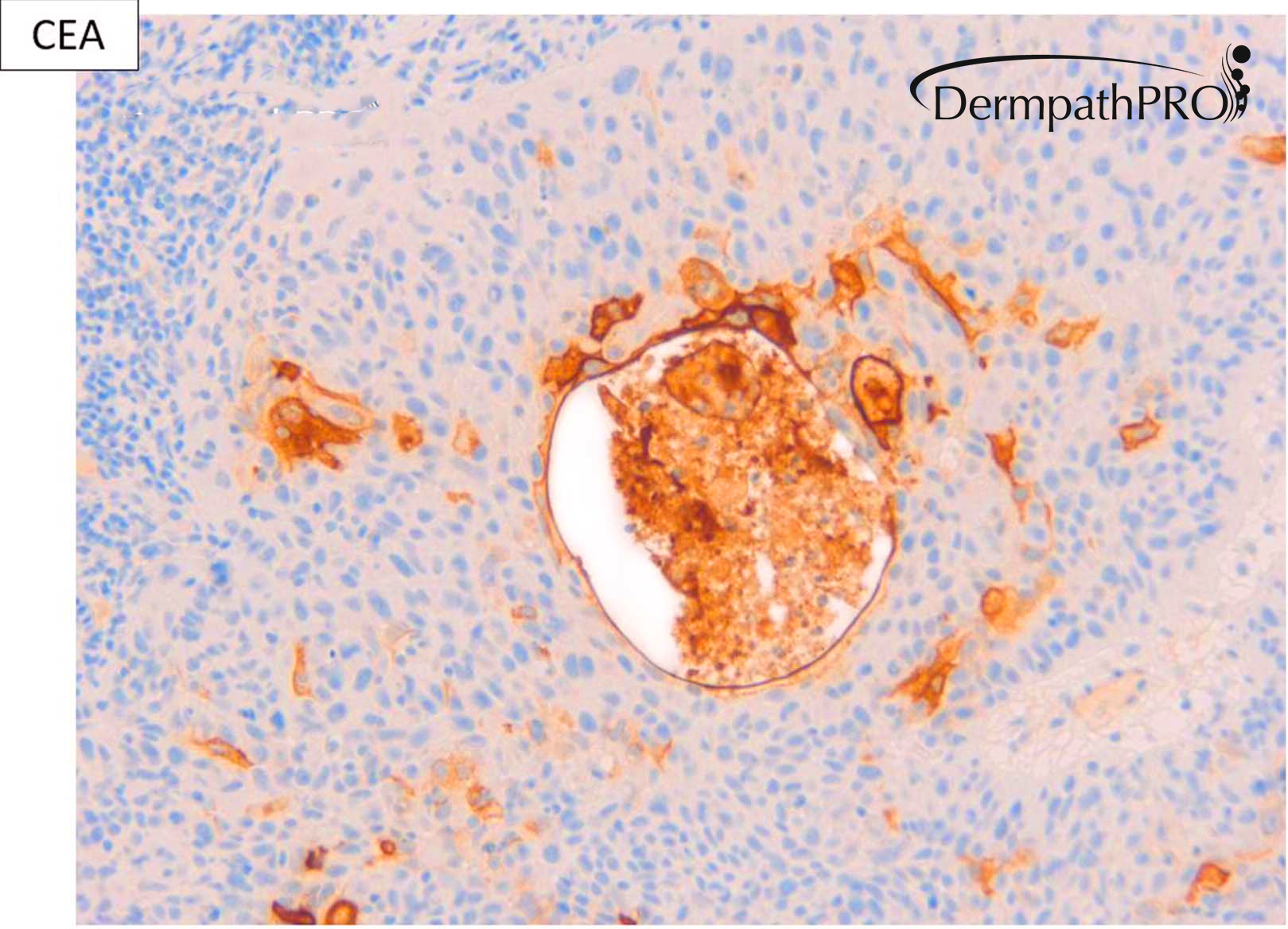
M80. Cheek. Initially 8 x 8mm lesion (3 months) but at 4 weeks partially regressed to a 3 x 4mm papule. ?BCC ?BAK ?SCC

Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.