-
 2
2
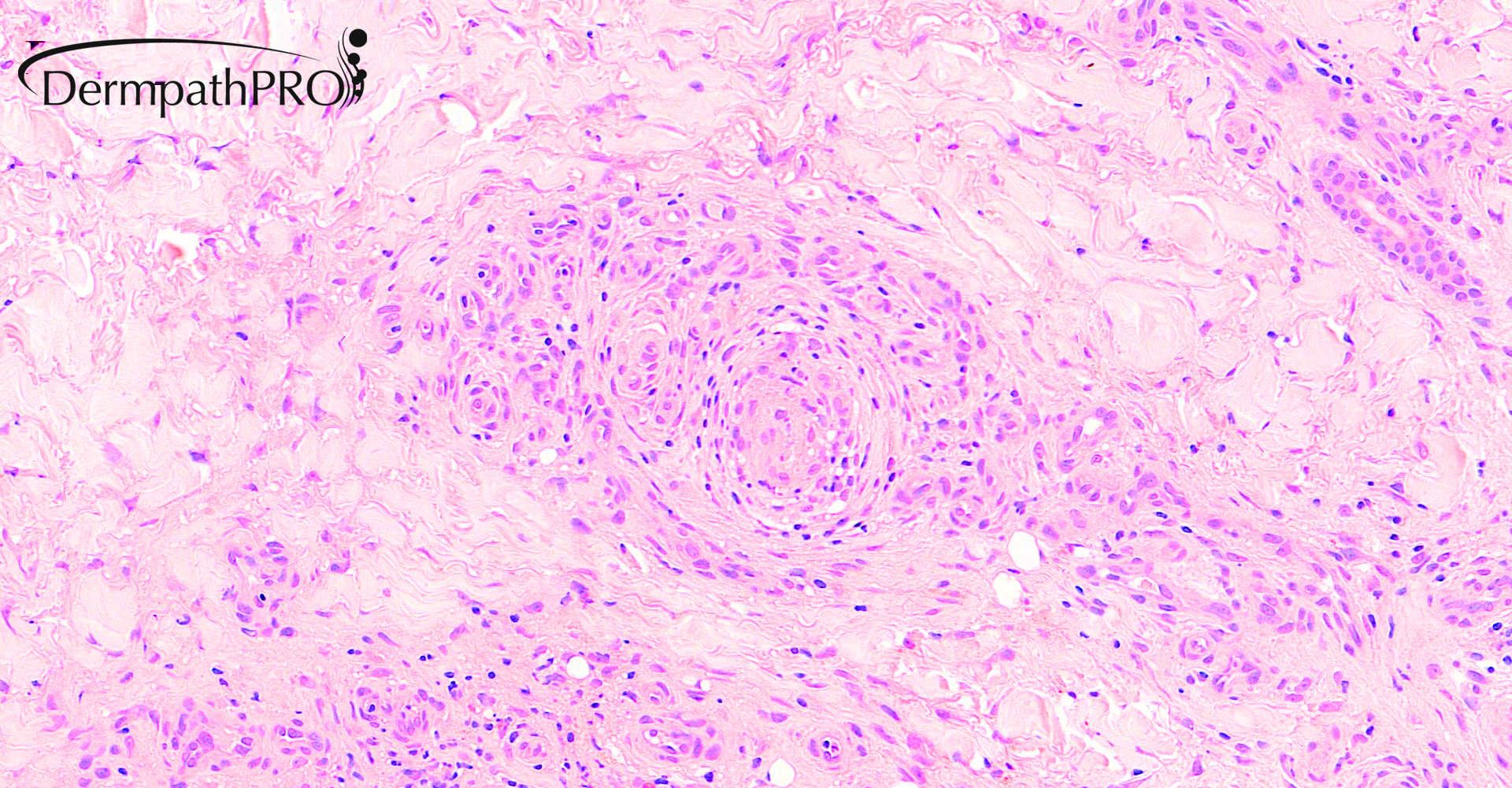
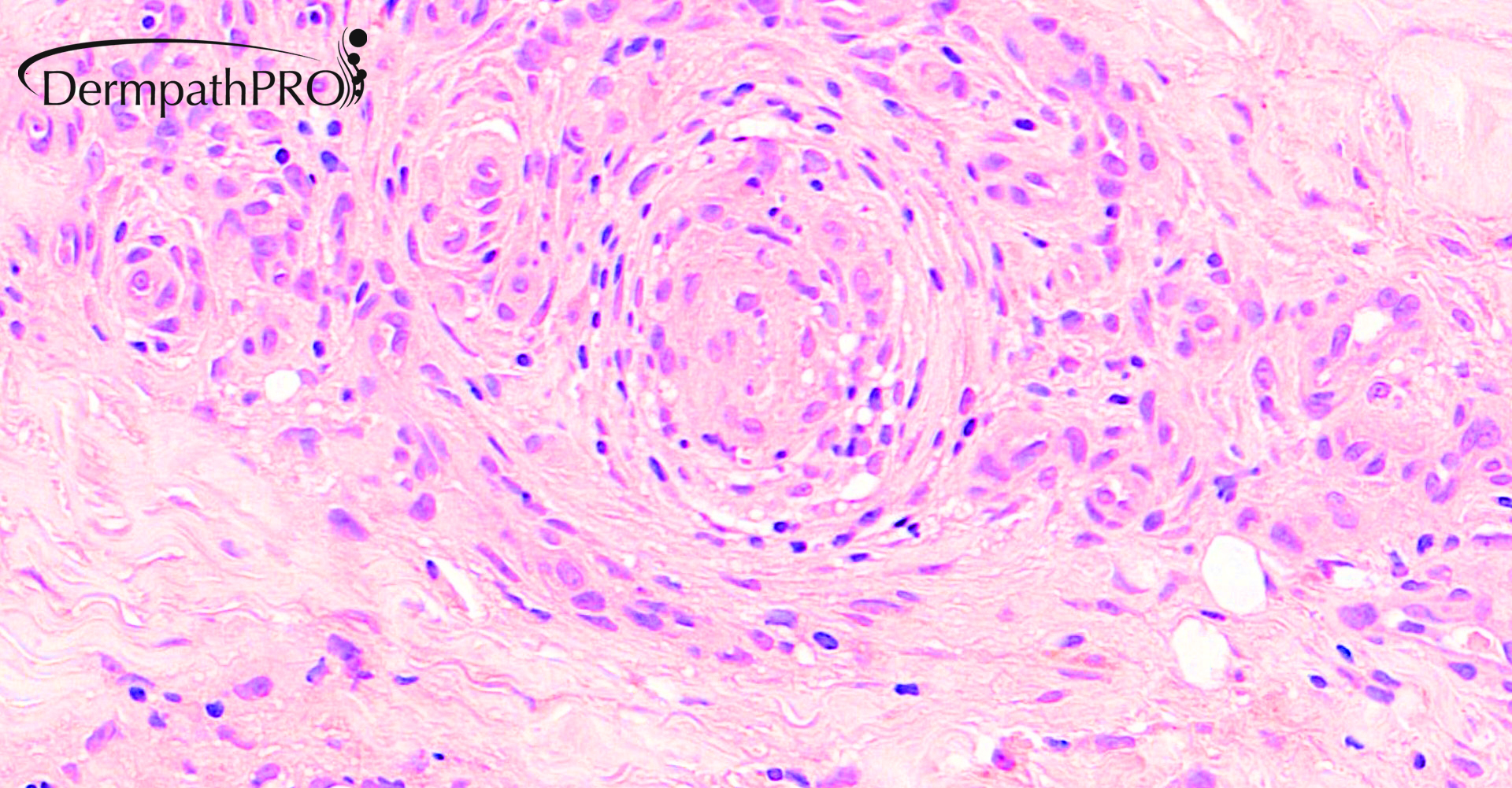
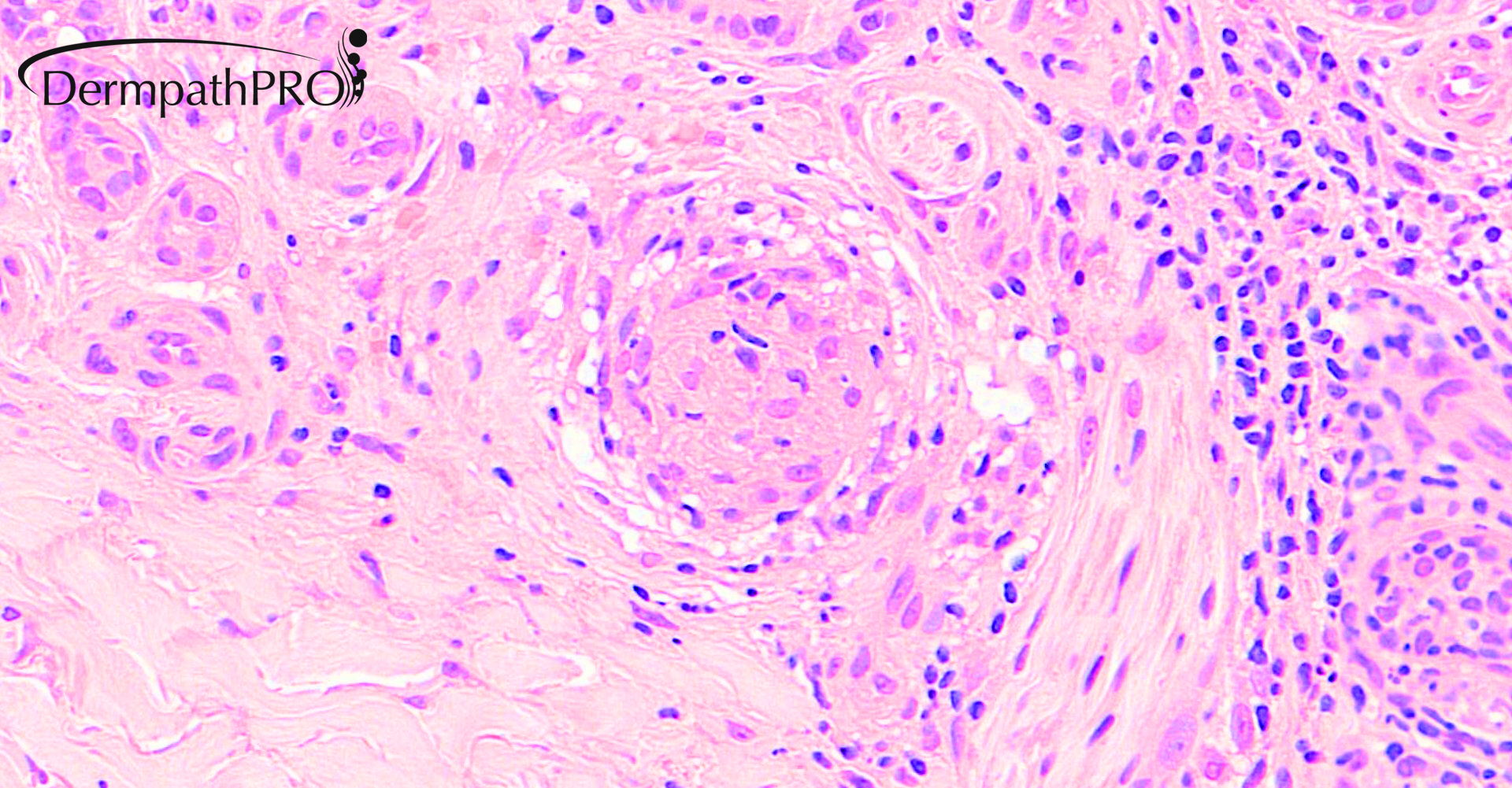
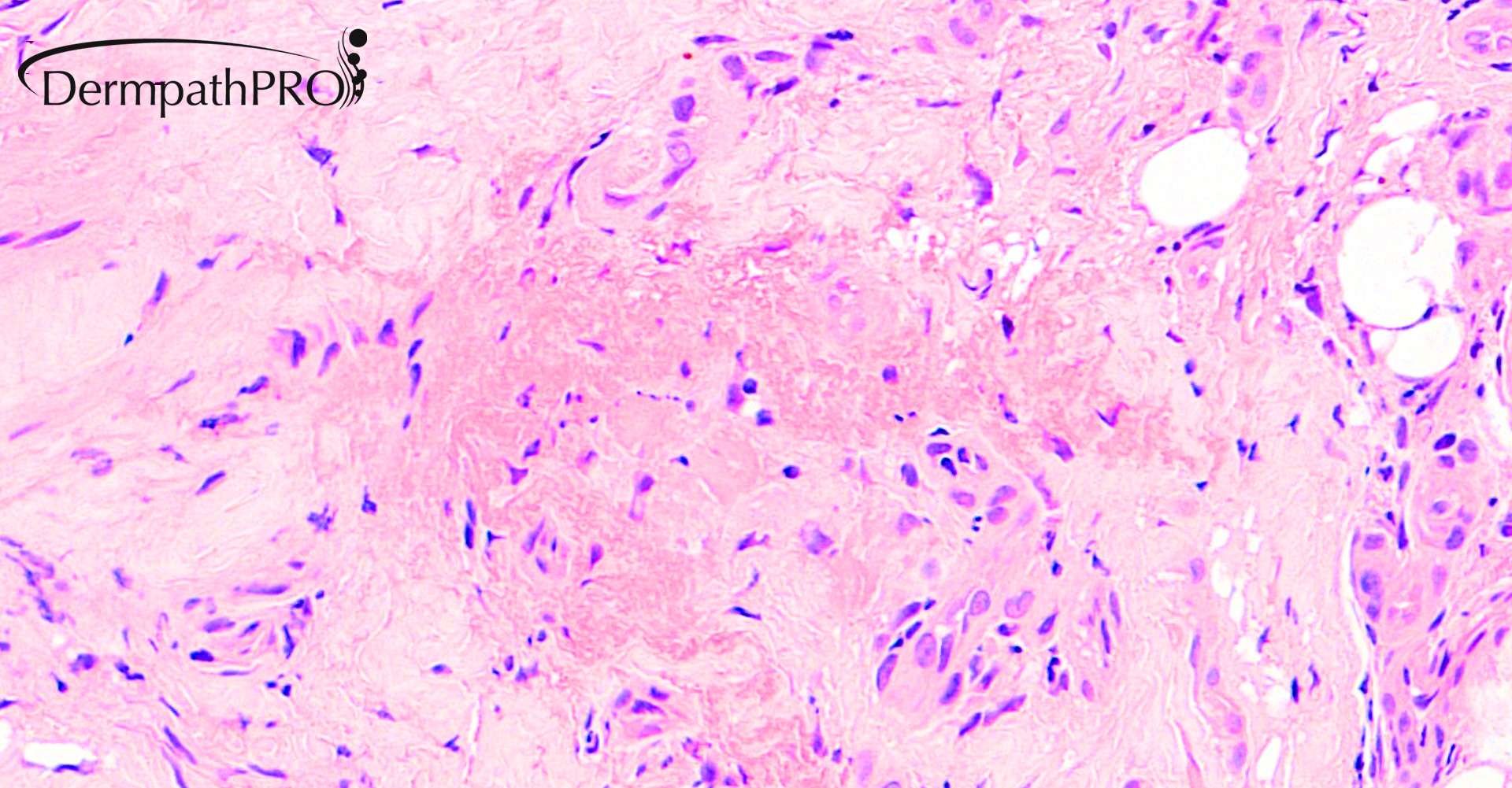
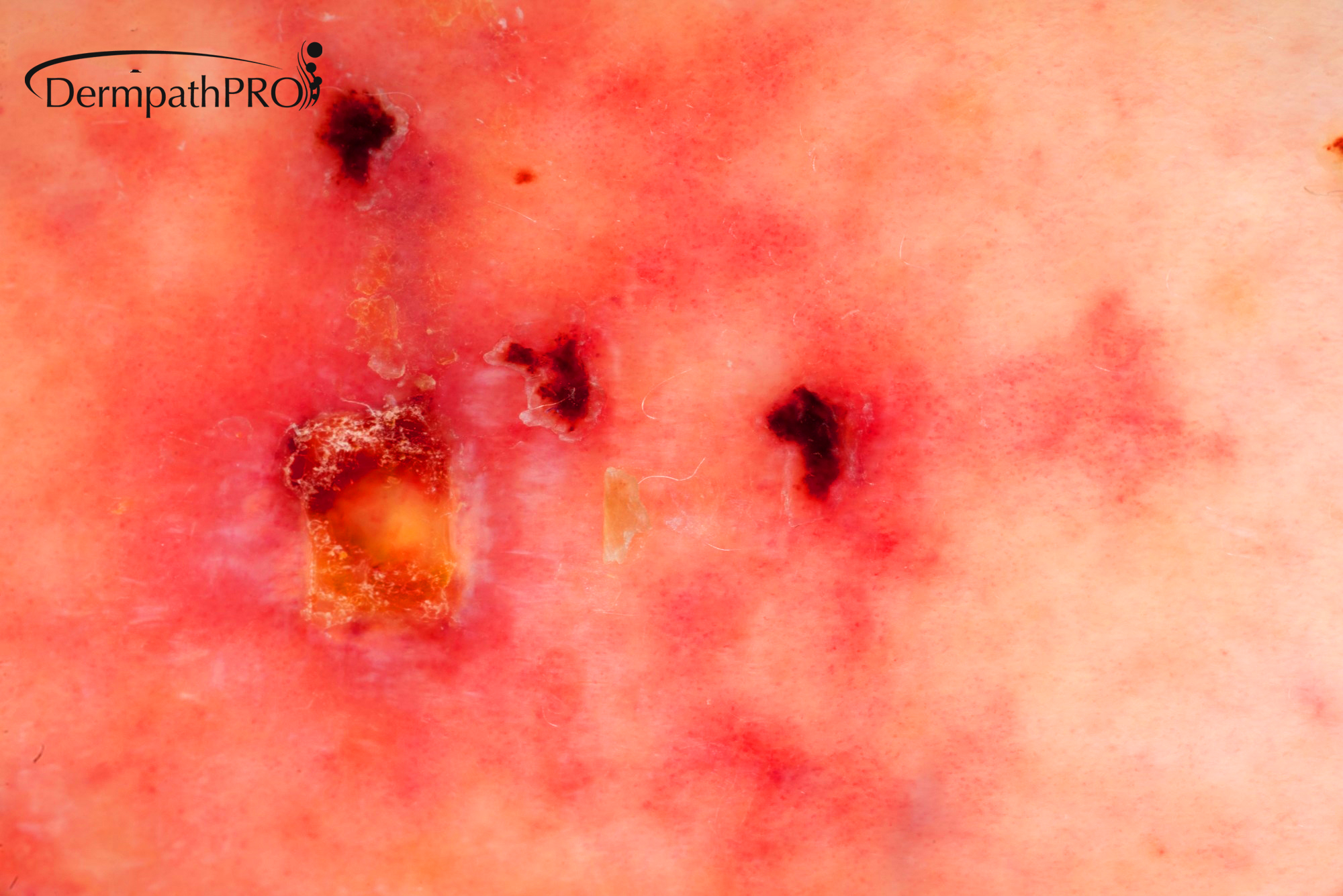
Case Number : Case 2576 - 21 May 2020 Posted By: Saleem Taibjee
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
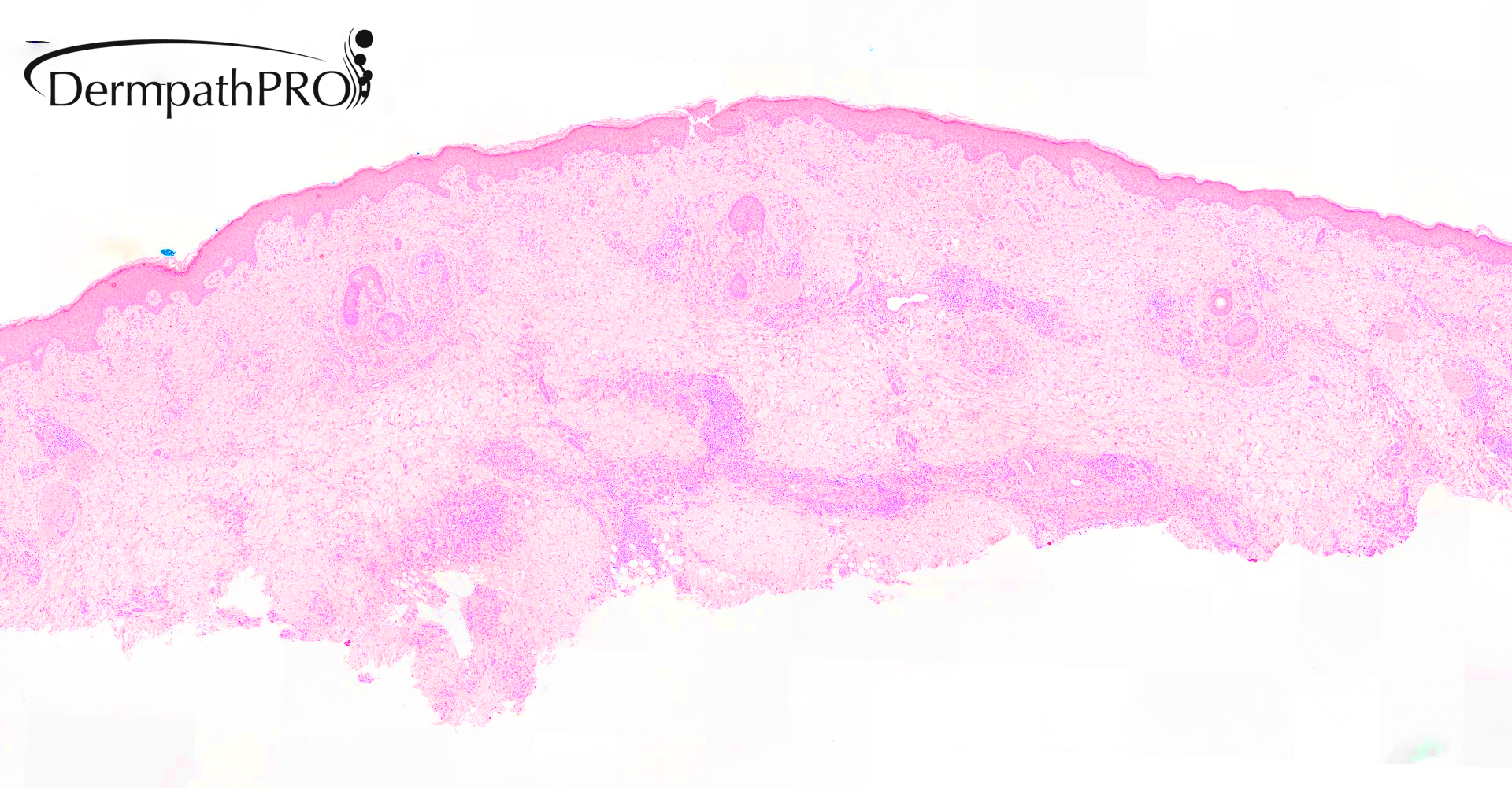
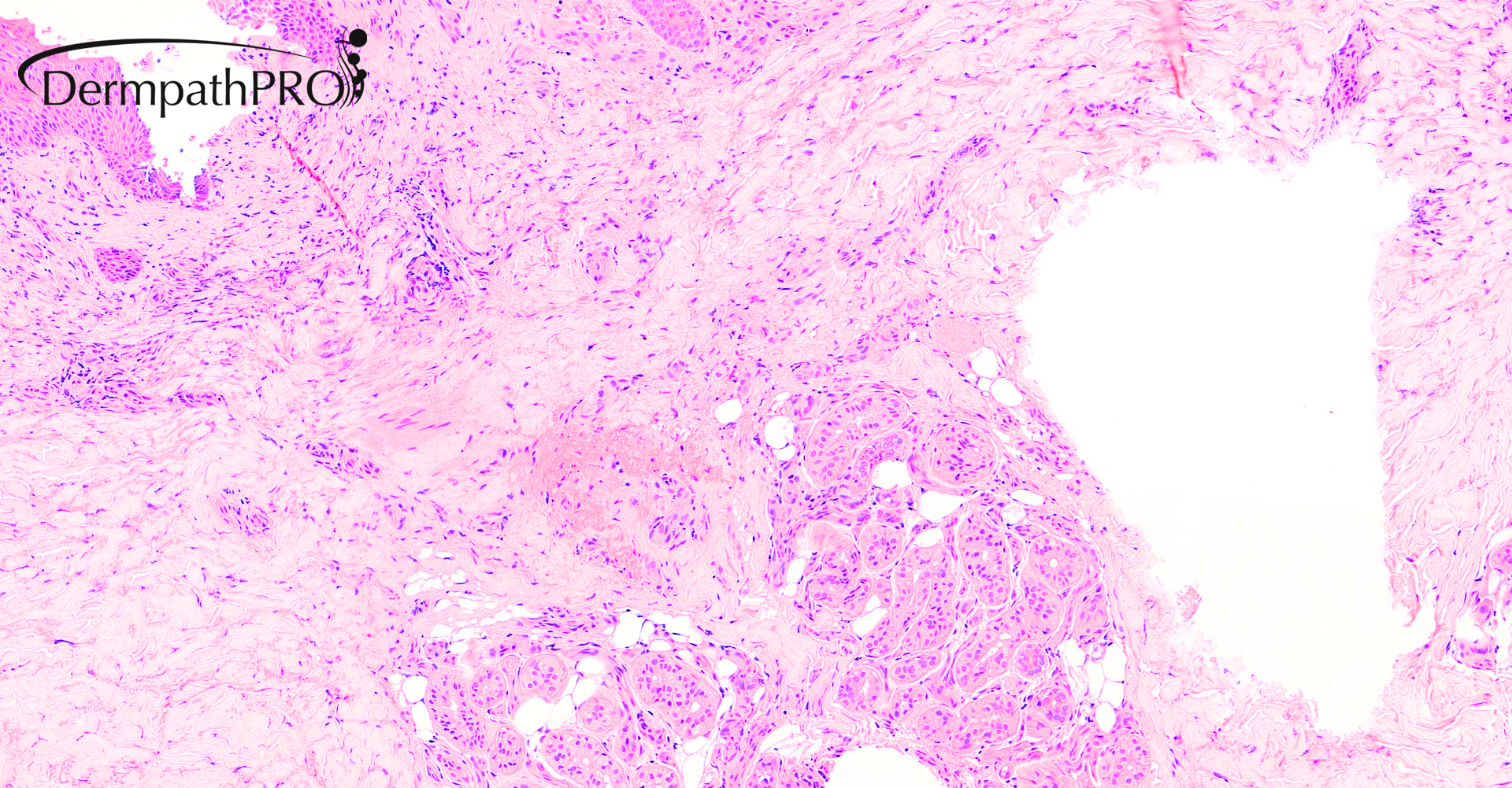
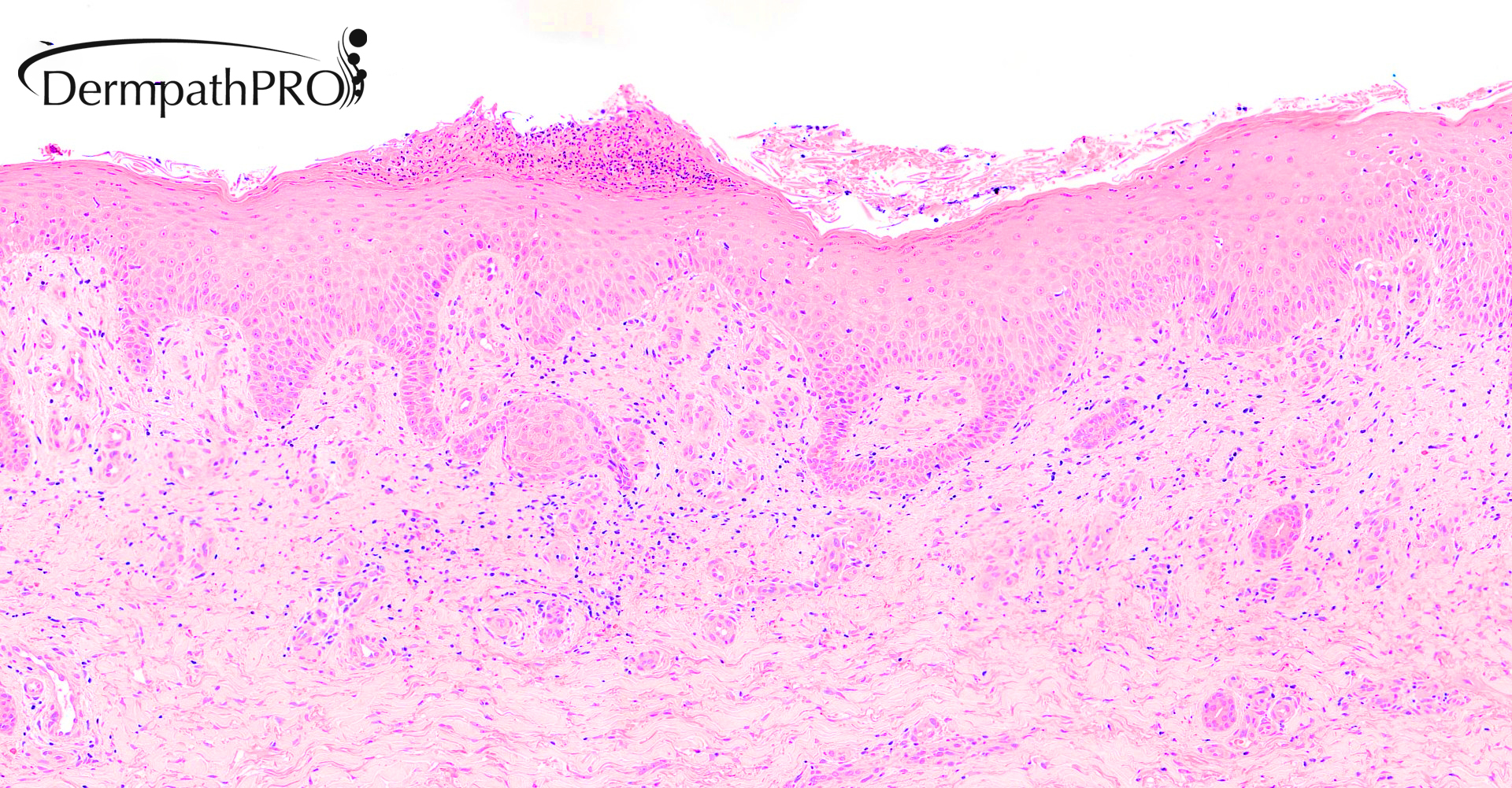
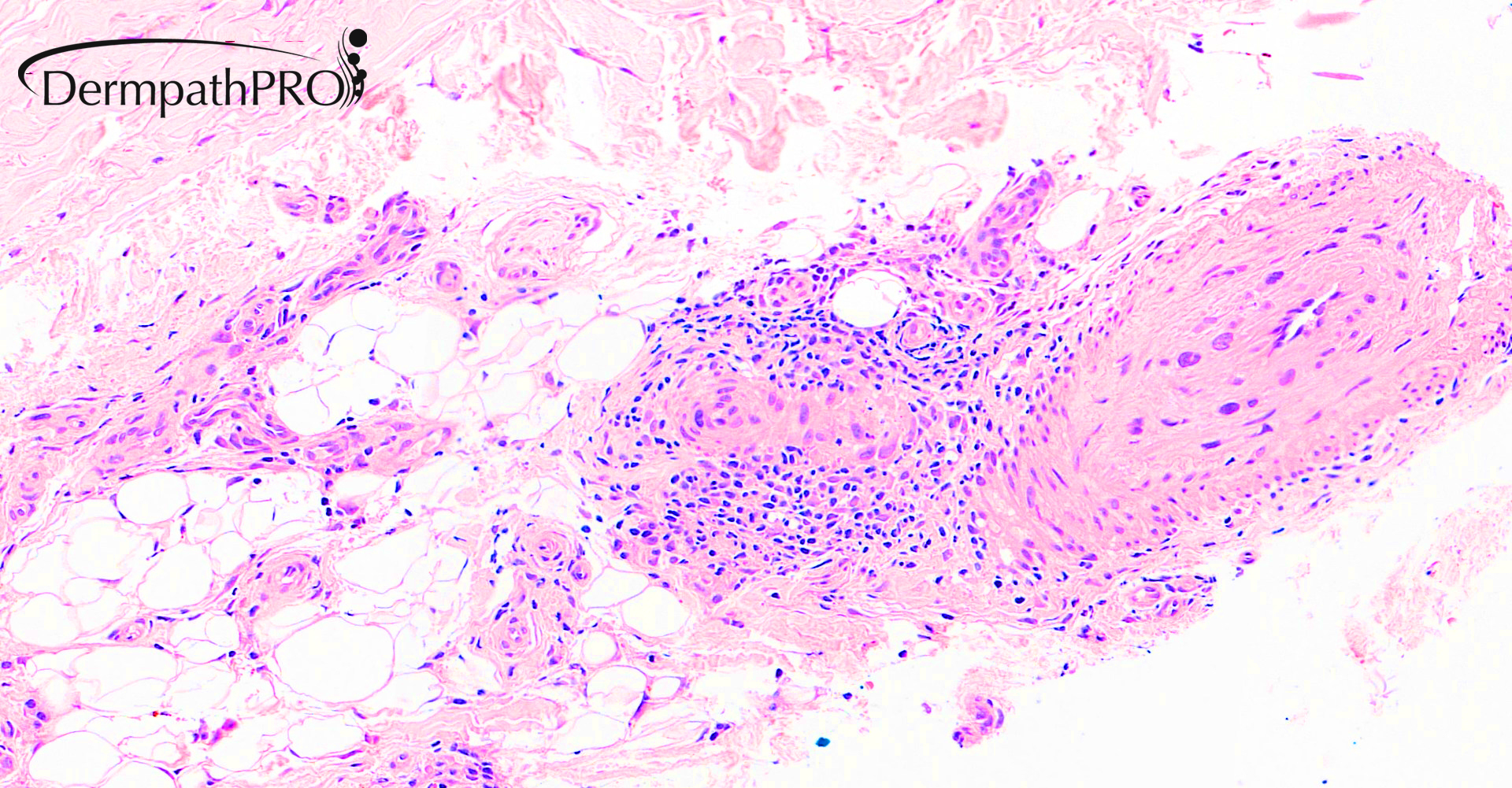
79M, erythematous changes and superficial ulceration right lower leg.


Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.