-
 2
2
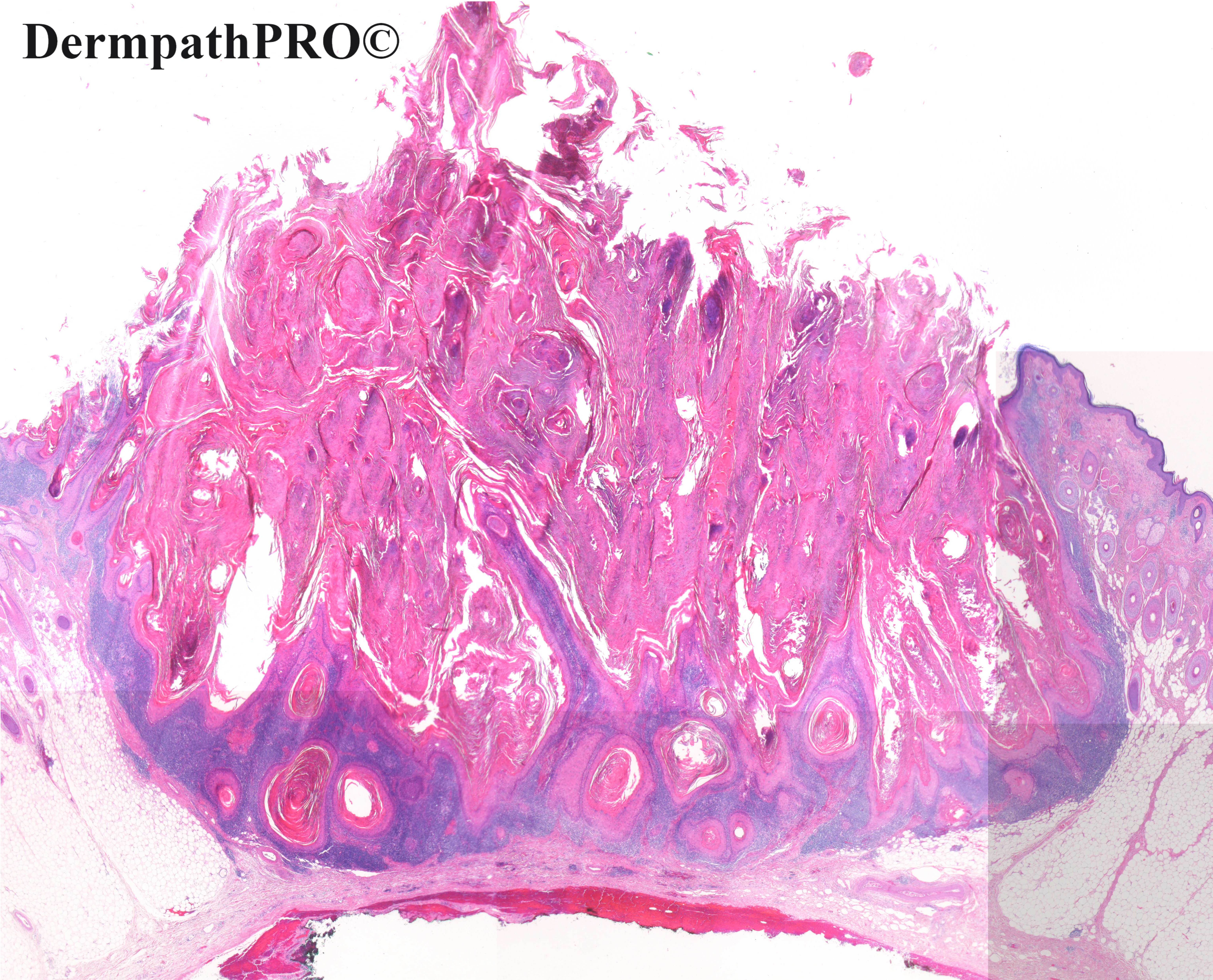
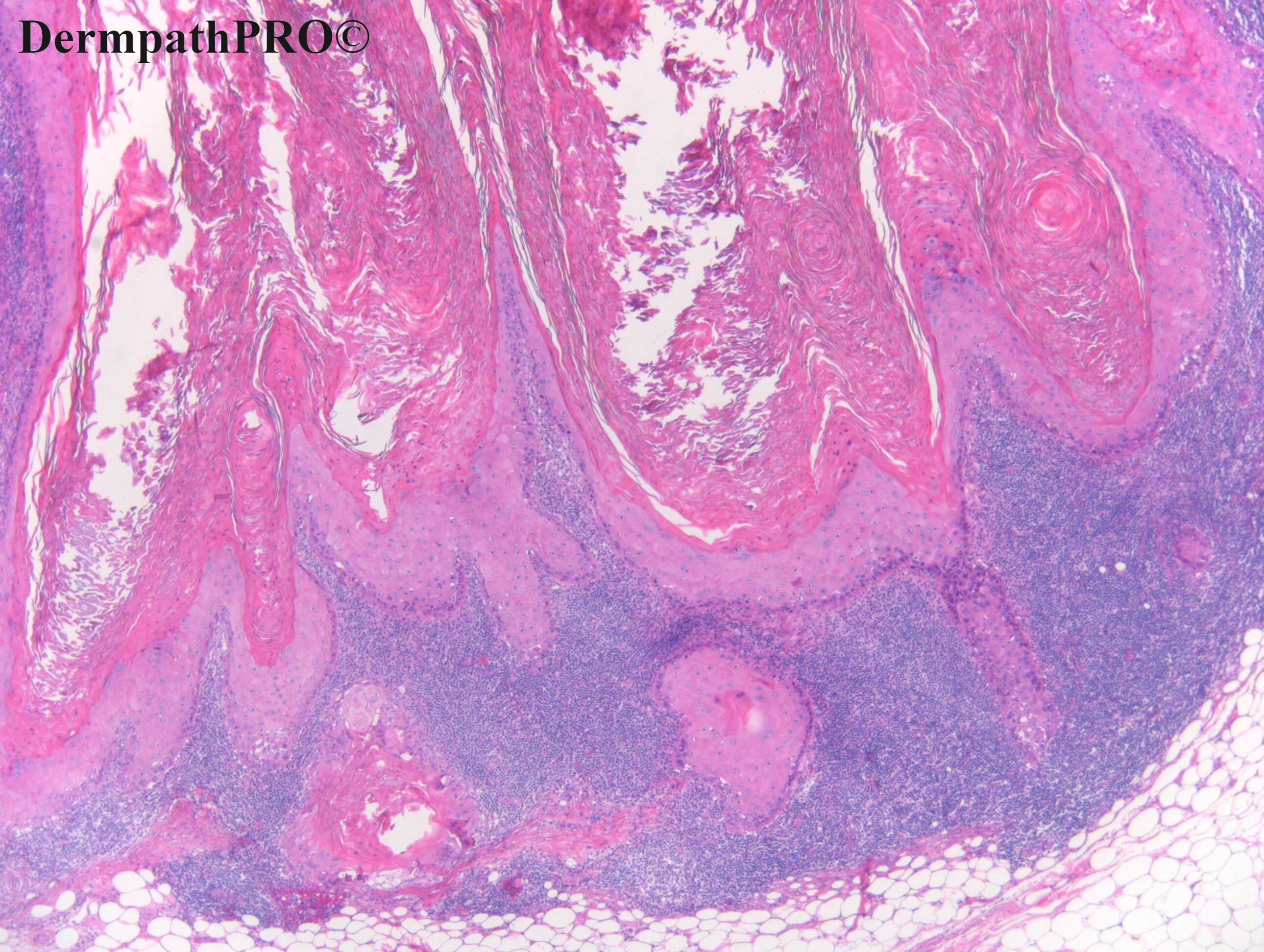
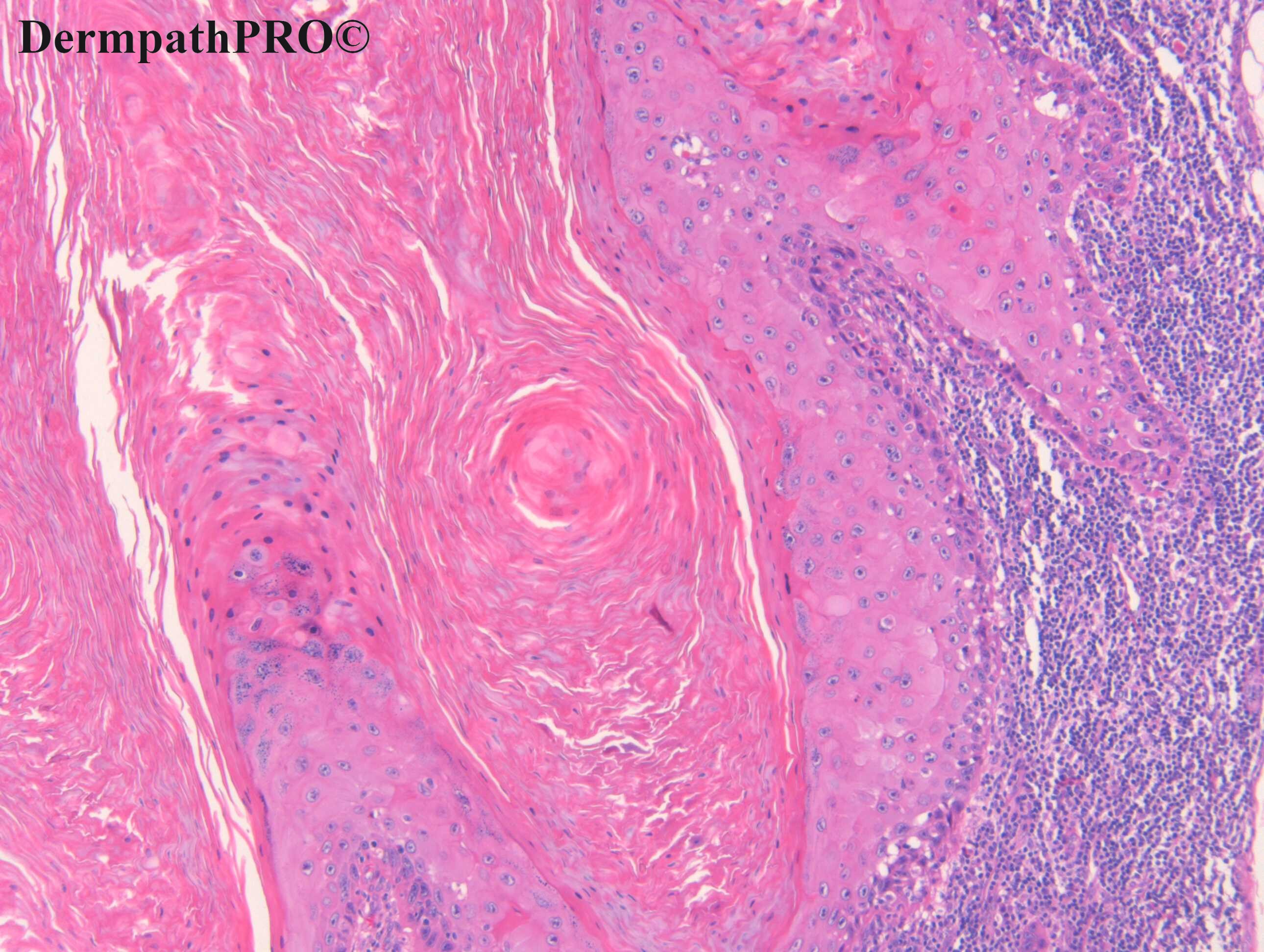
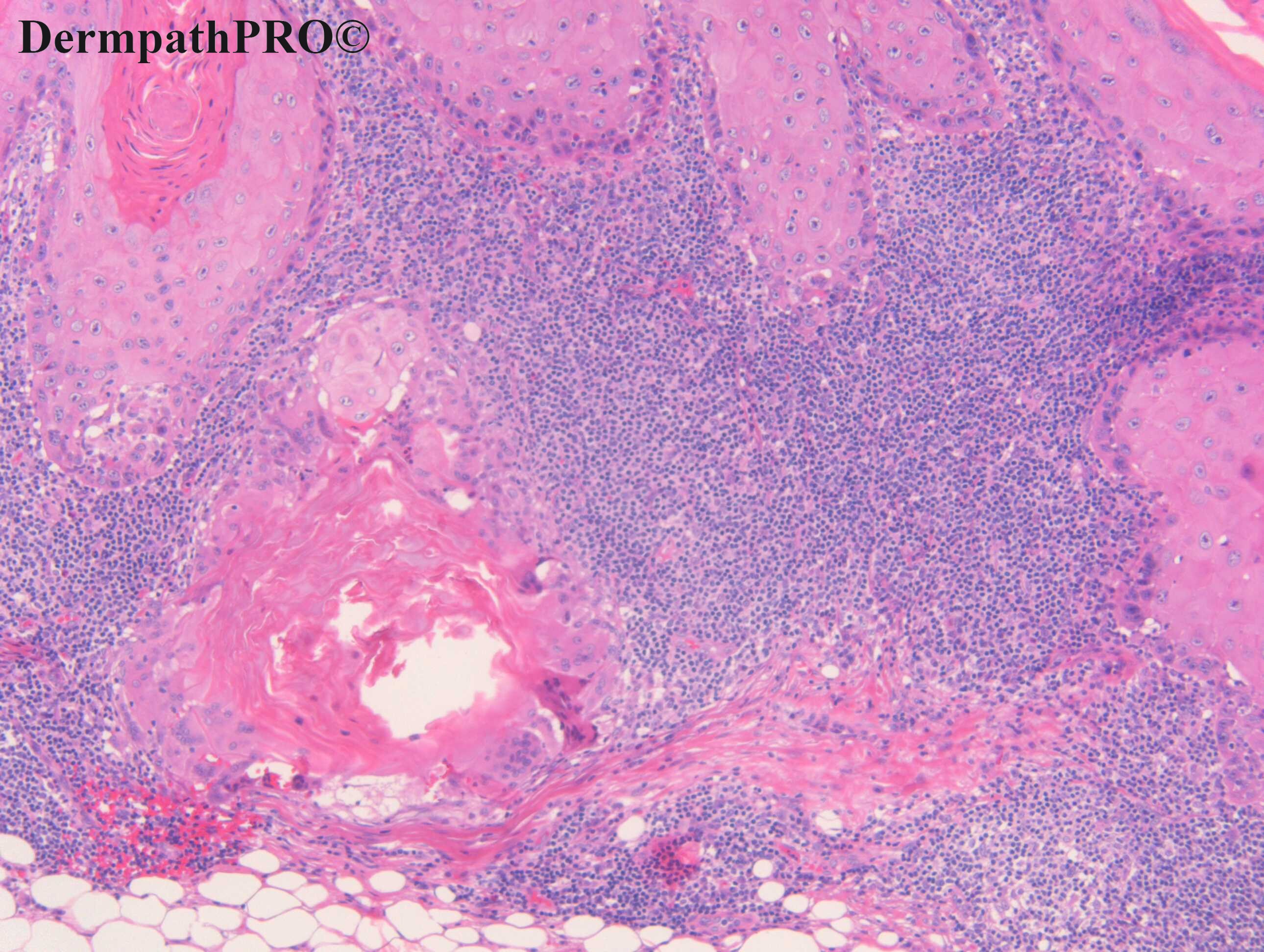
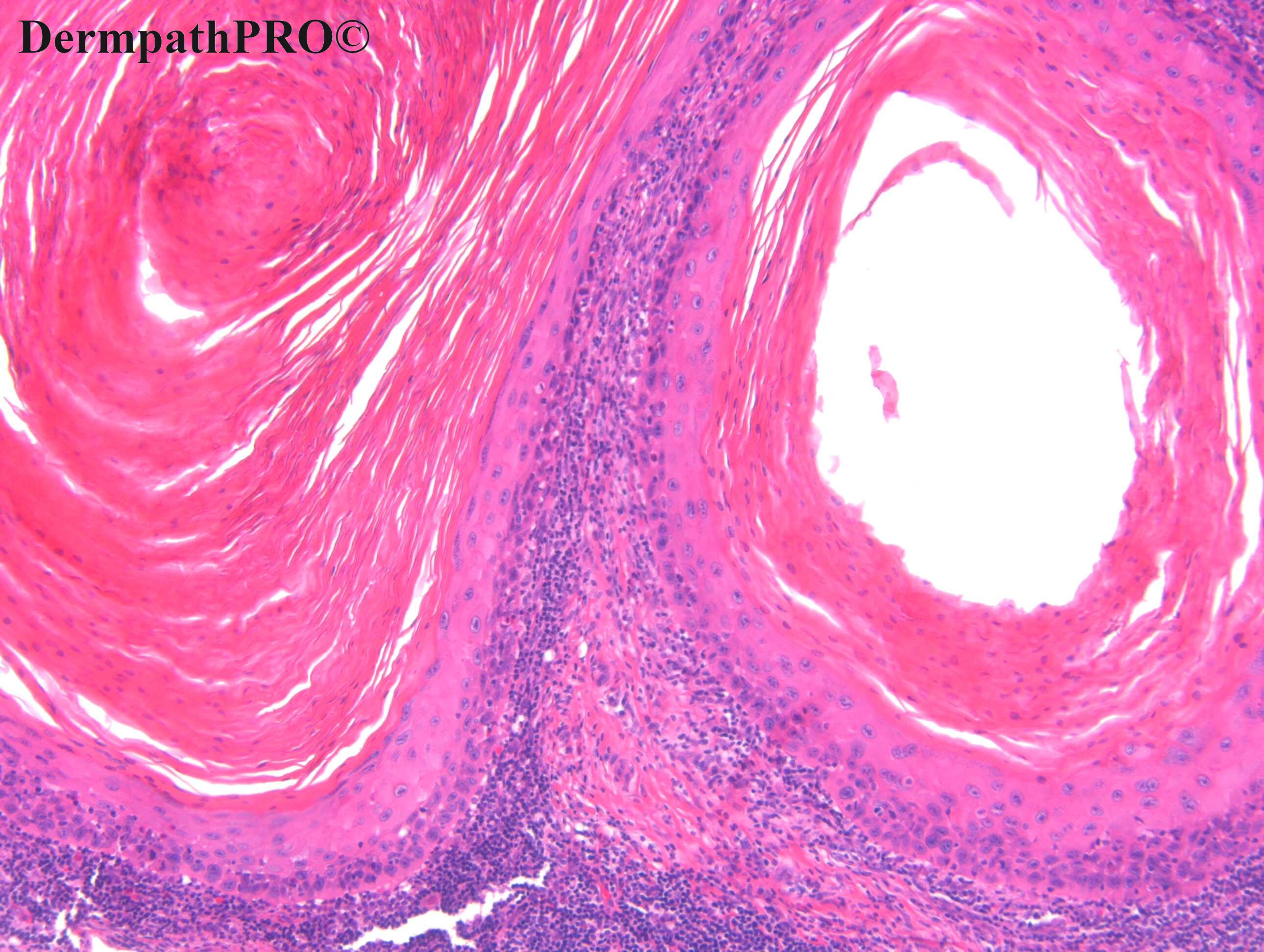
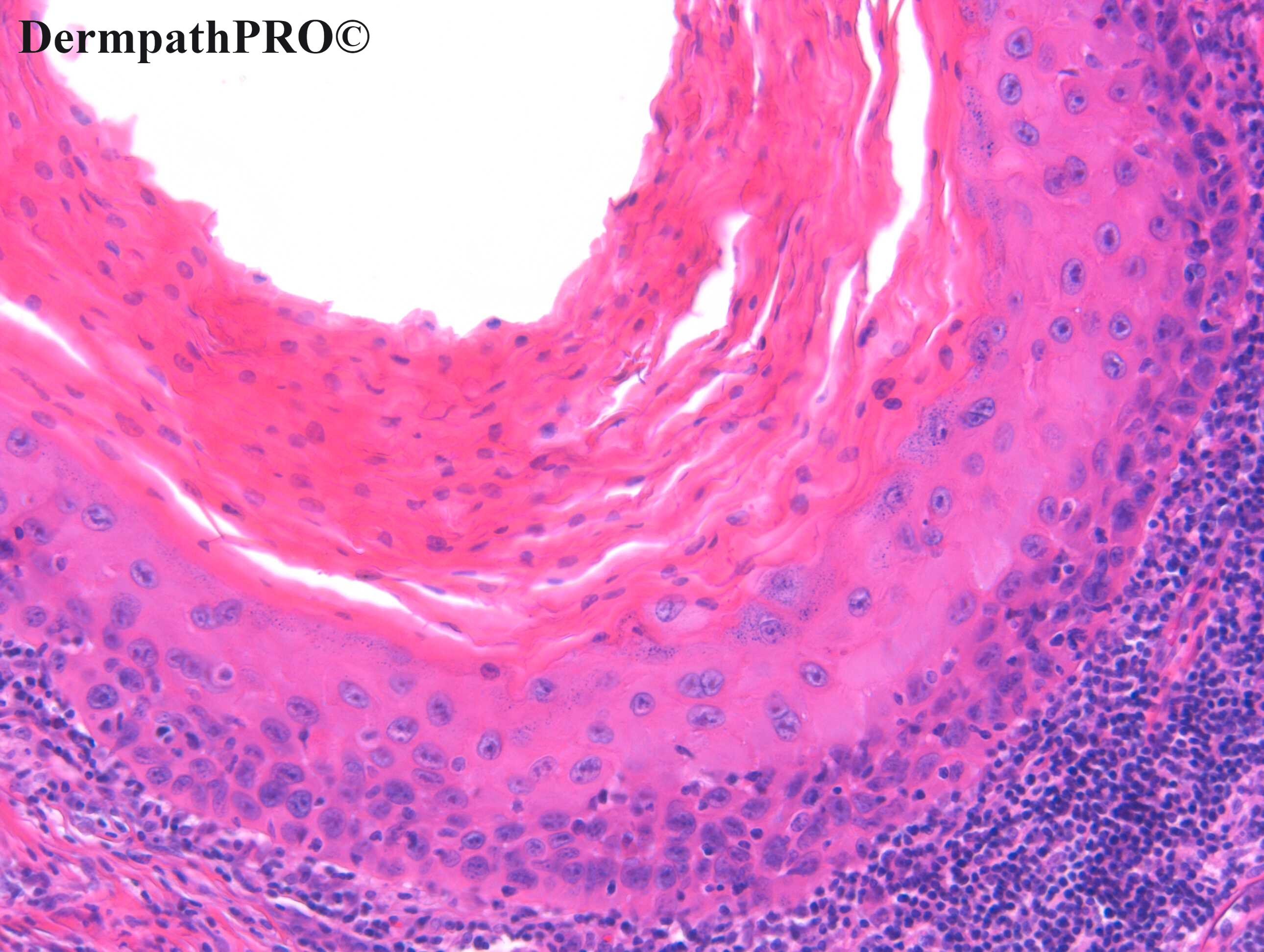
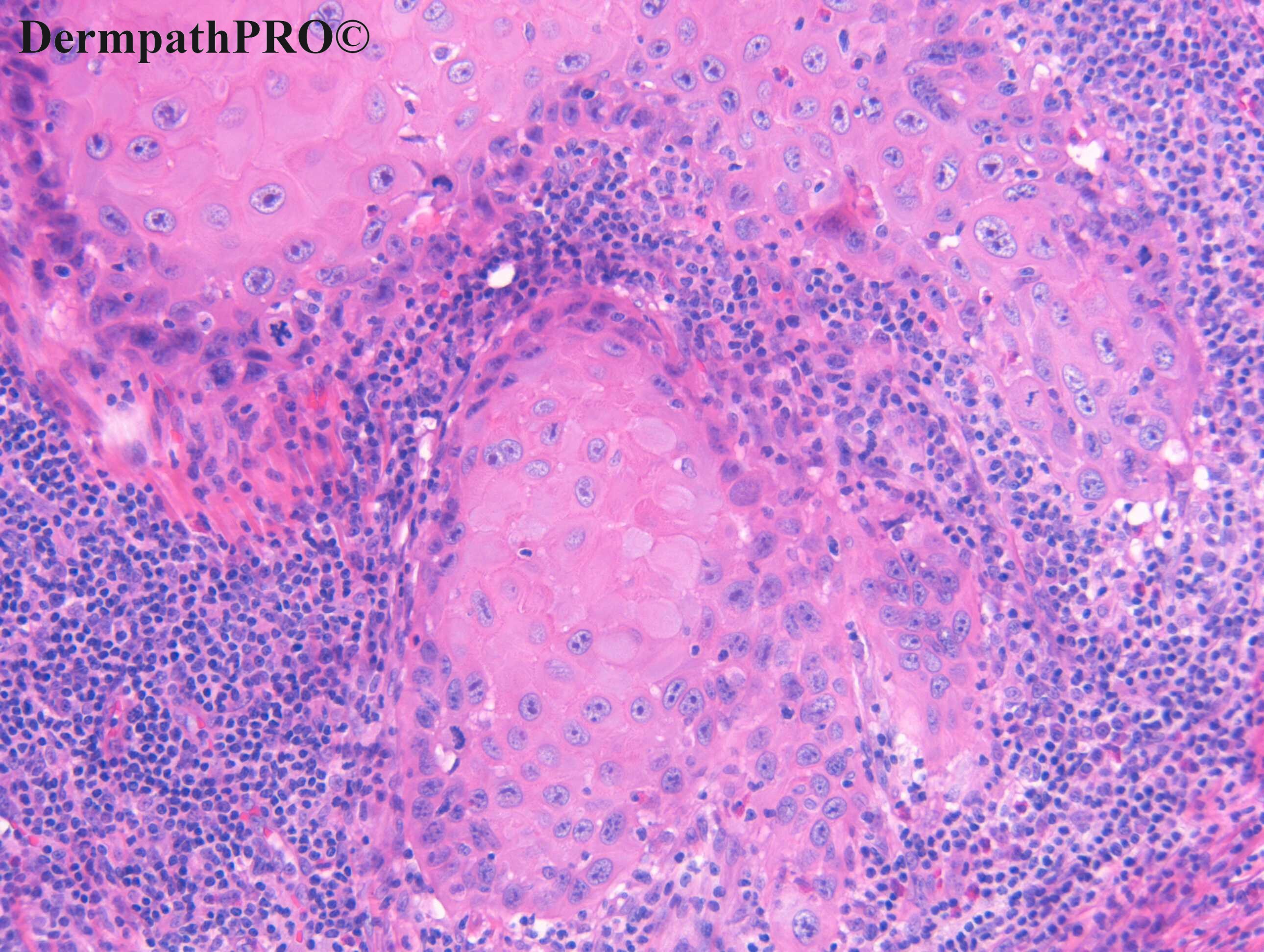
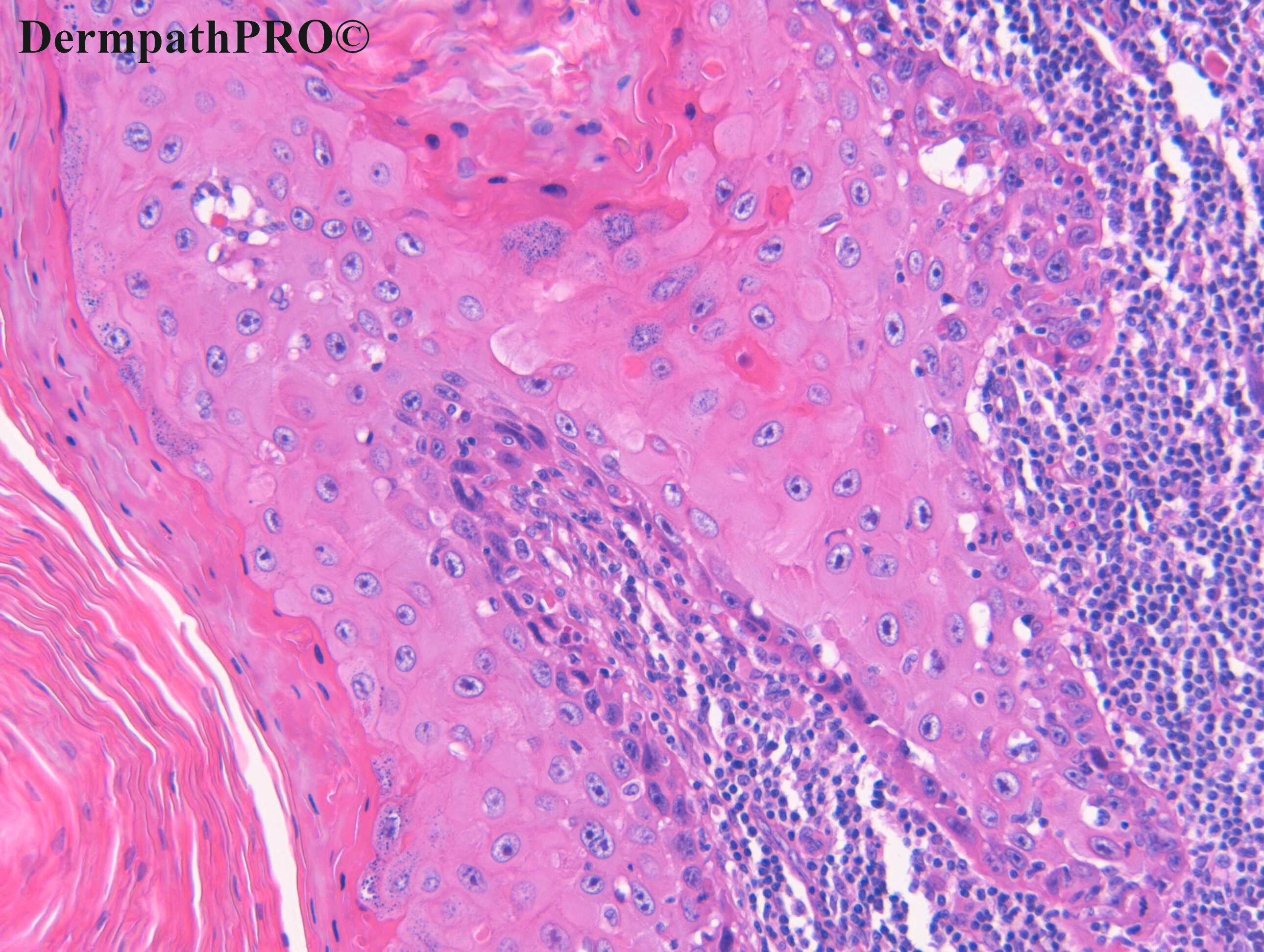
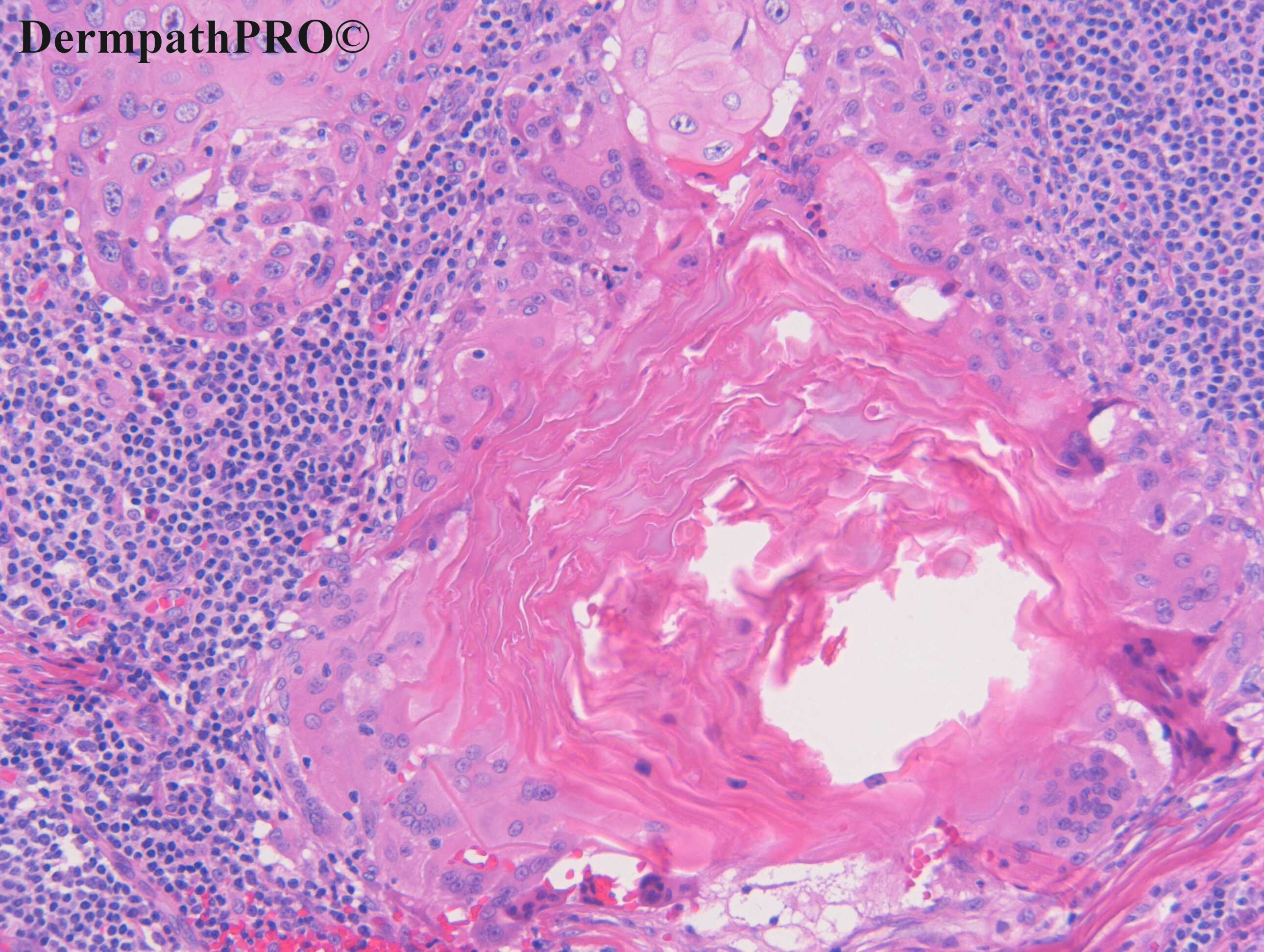
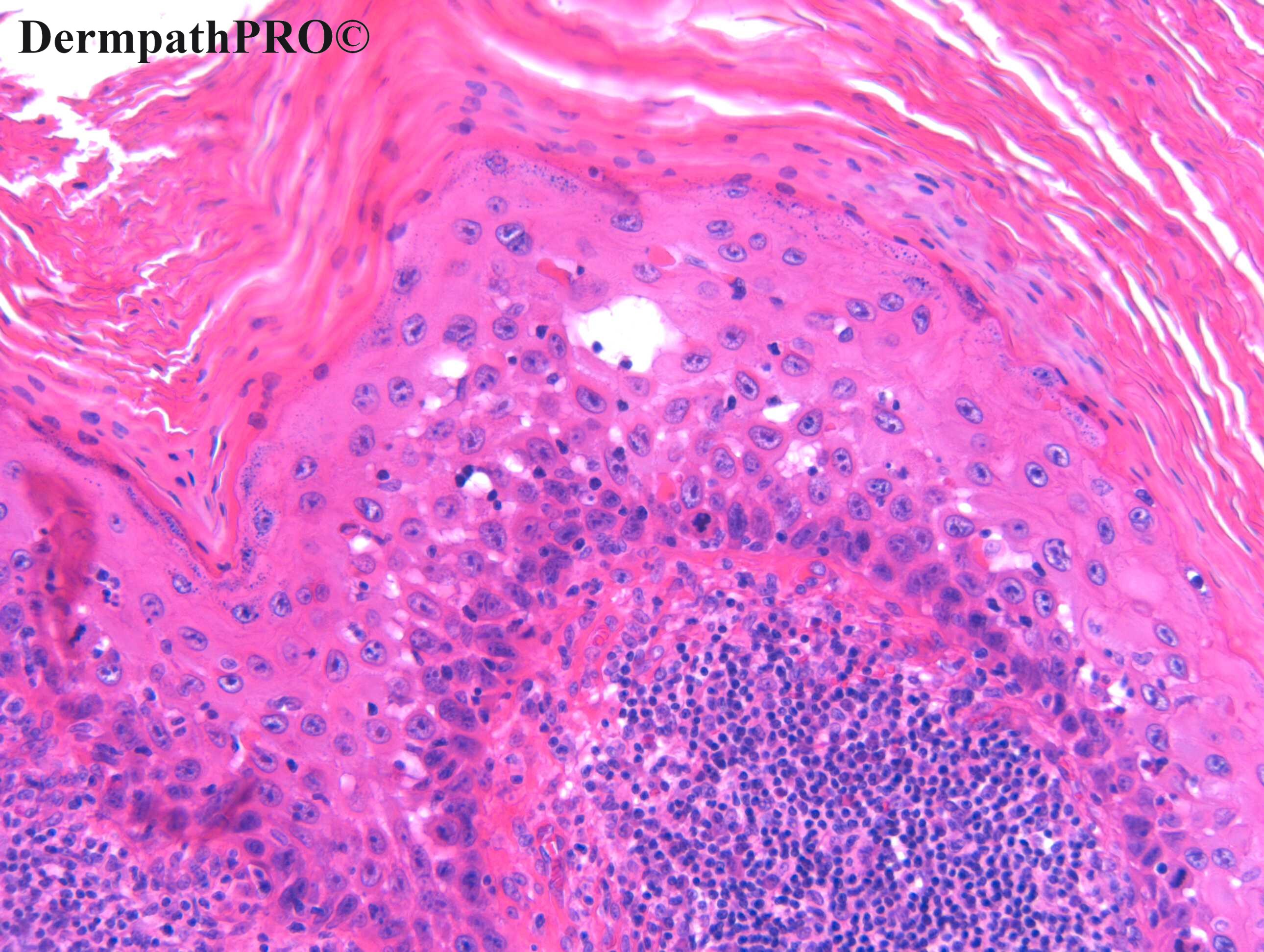
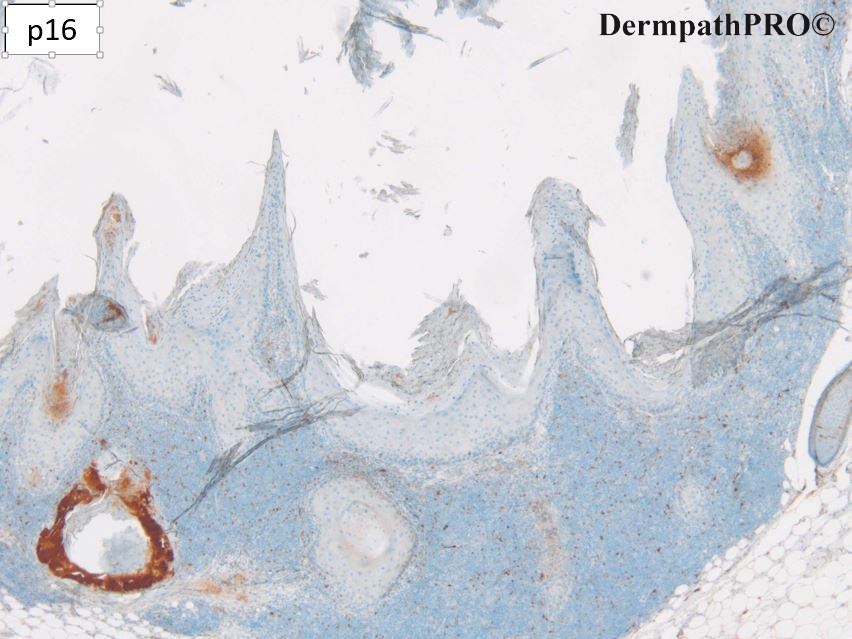
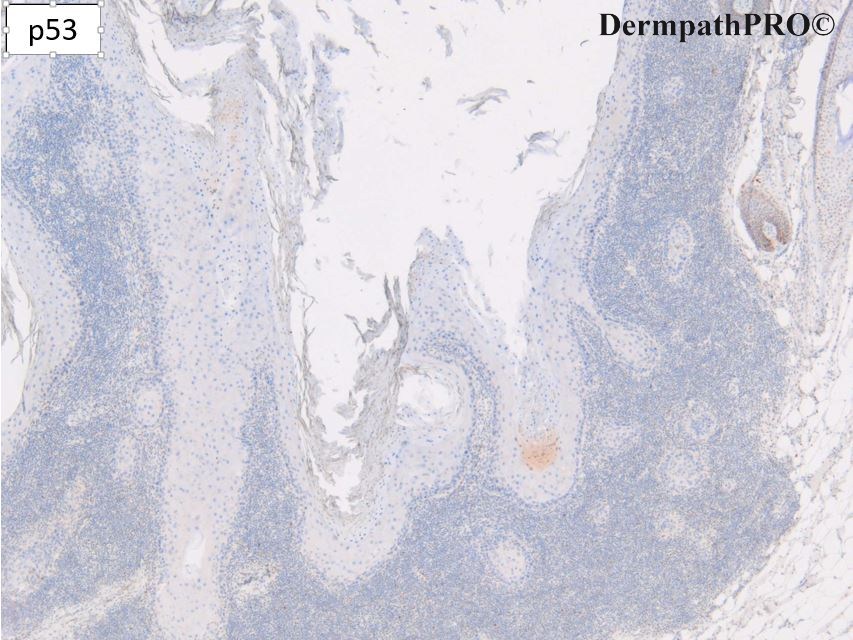
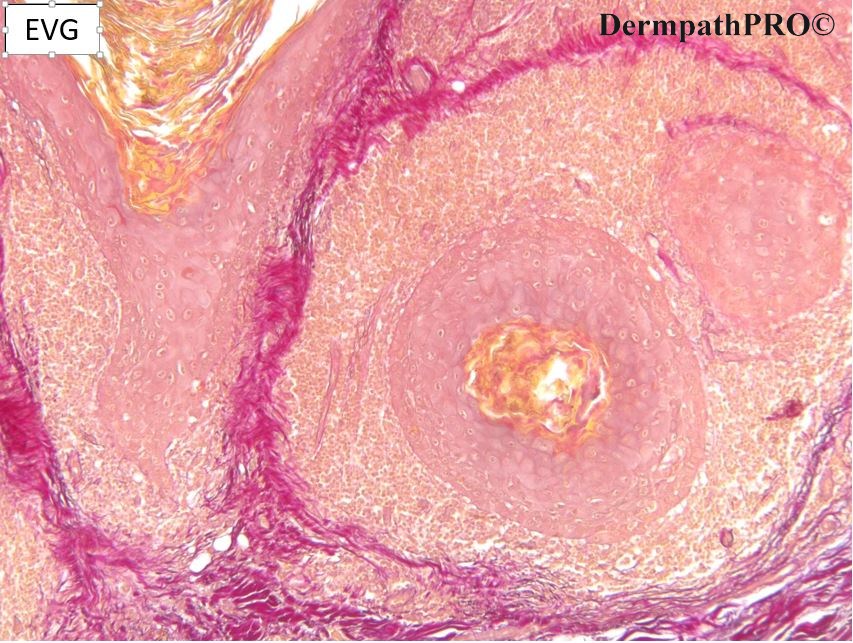
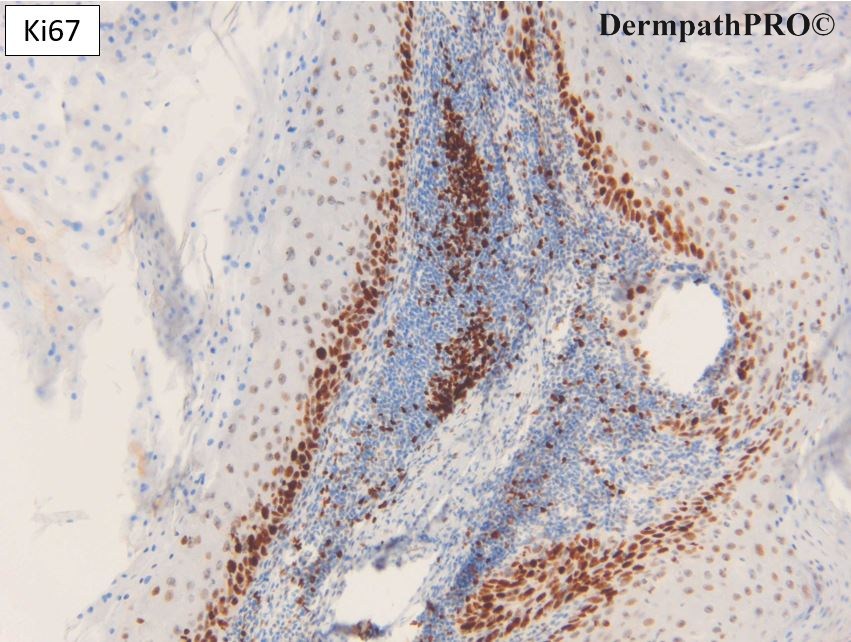
Case Number : Case 2707 - 20 November 2020 Posted By: Dr. Richard Carr
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
F75 Scalp. ?KA ?SCC

Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.