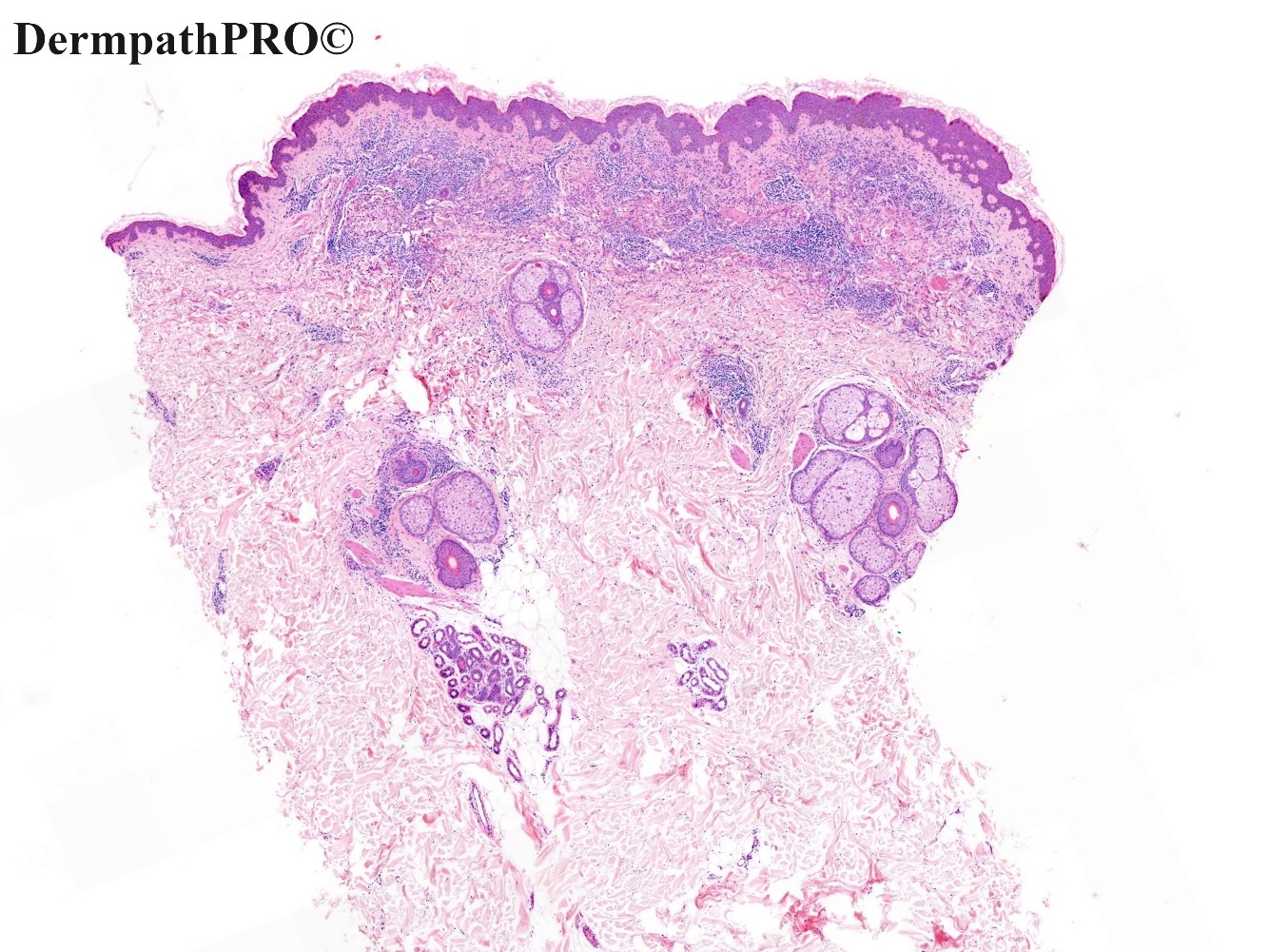
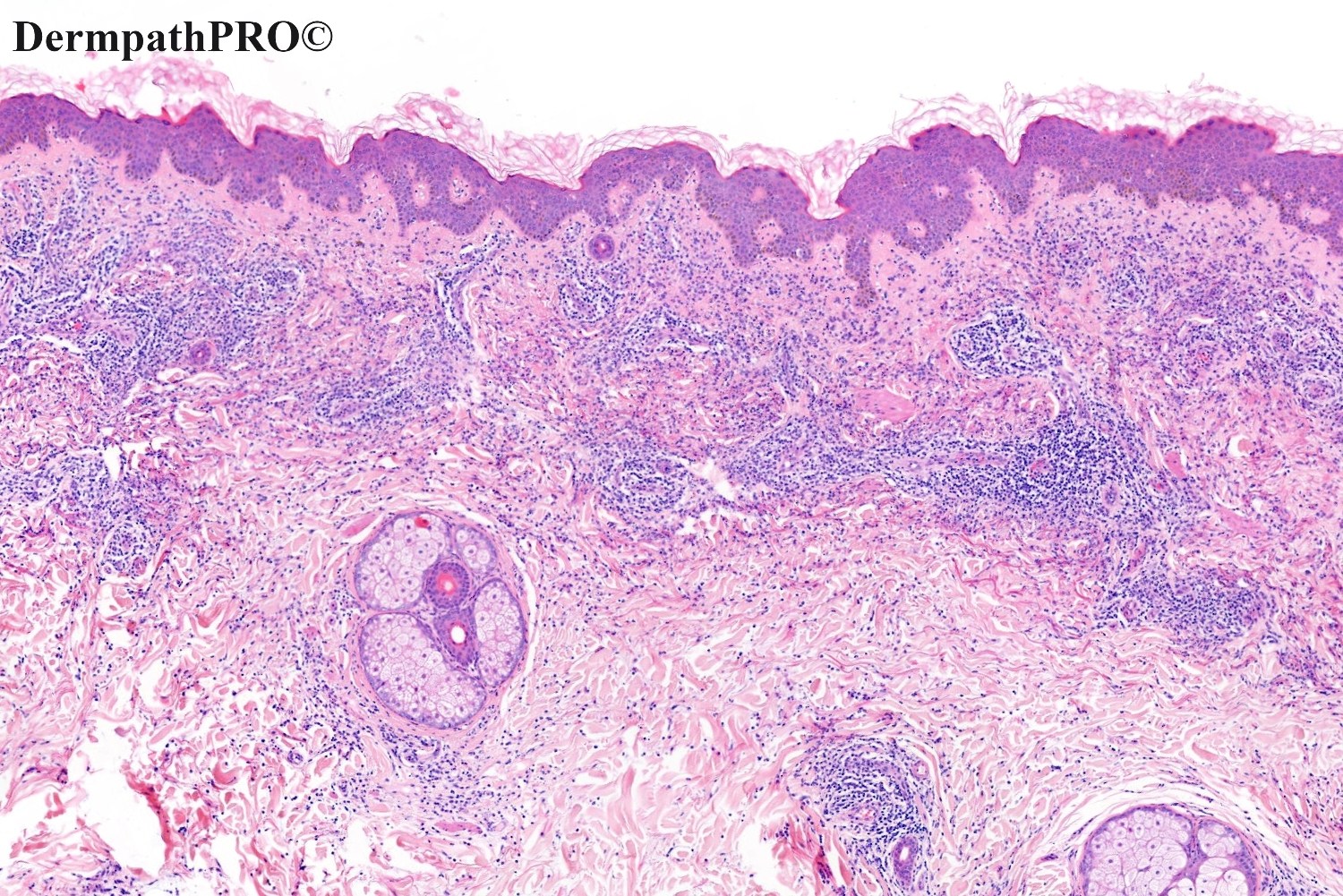
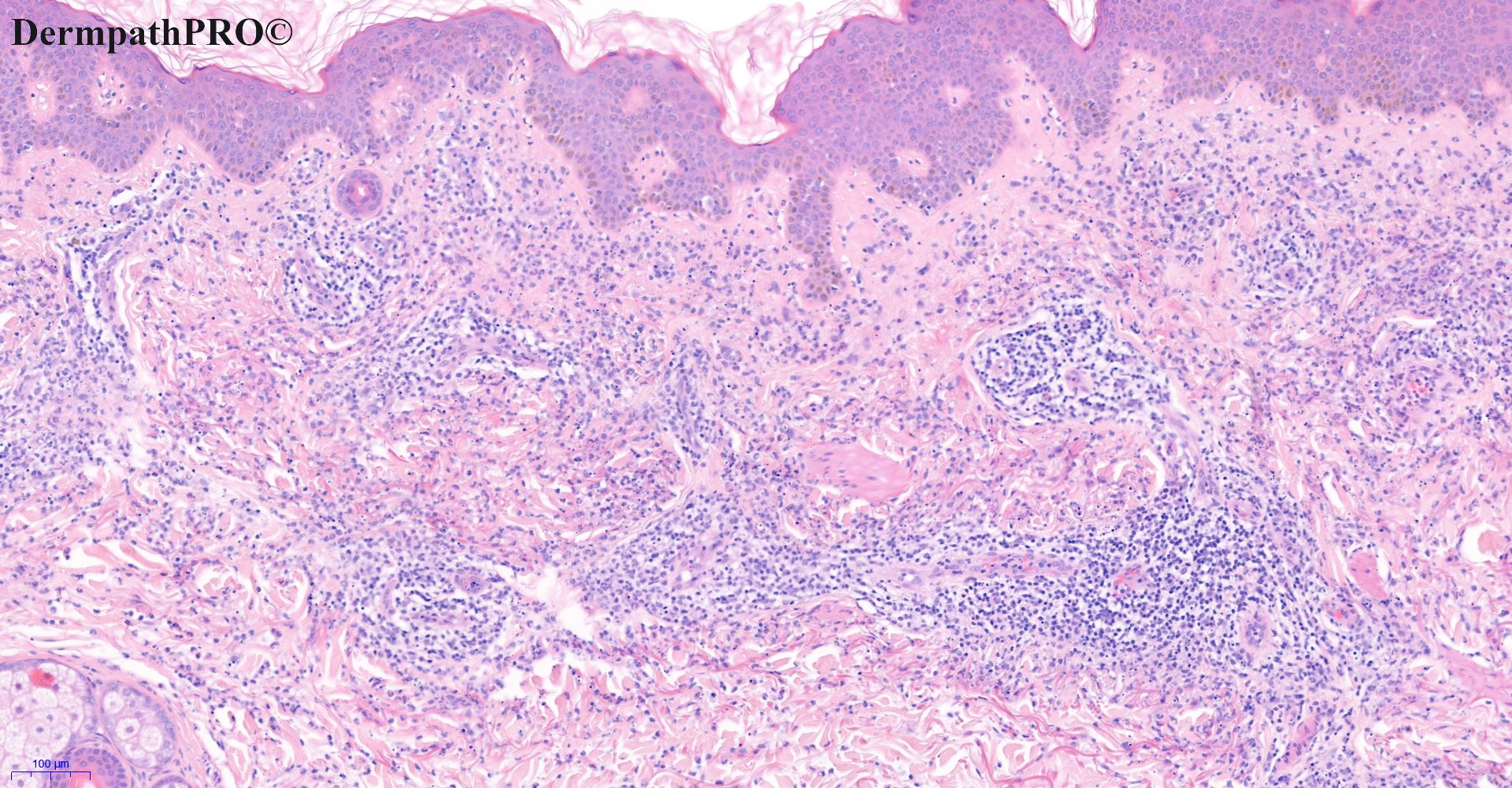
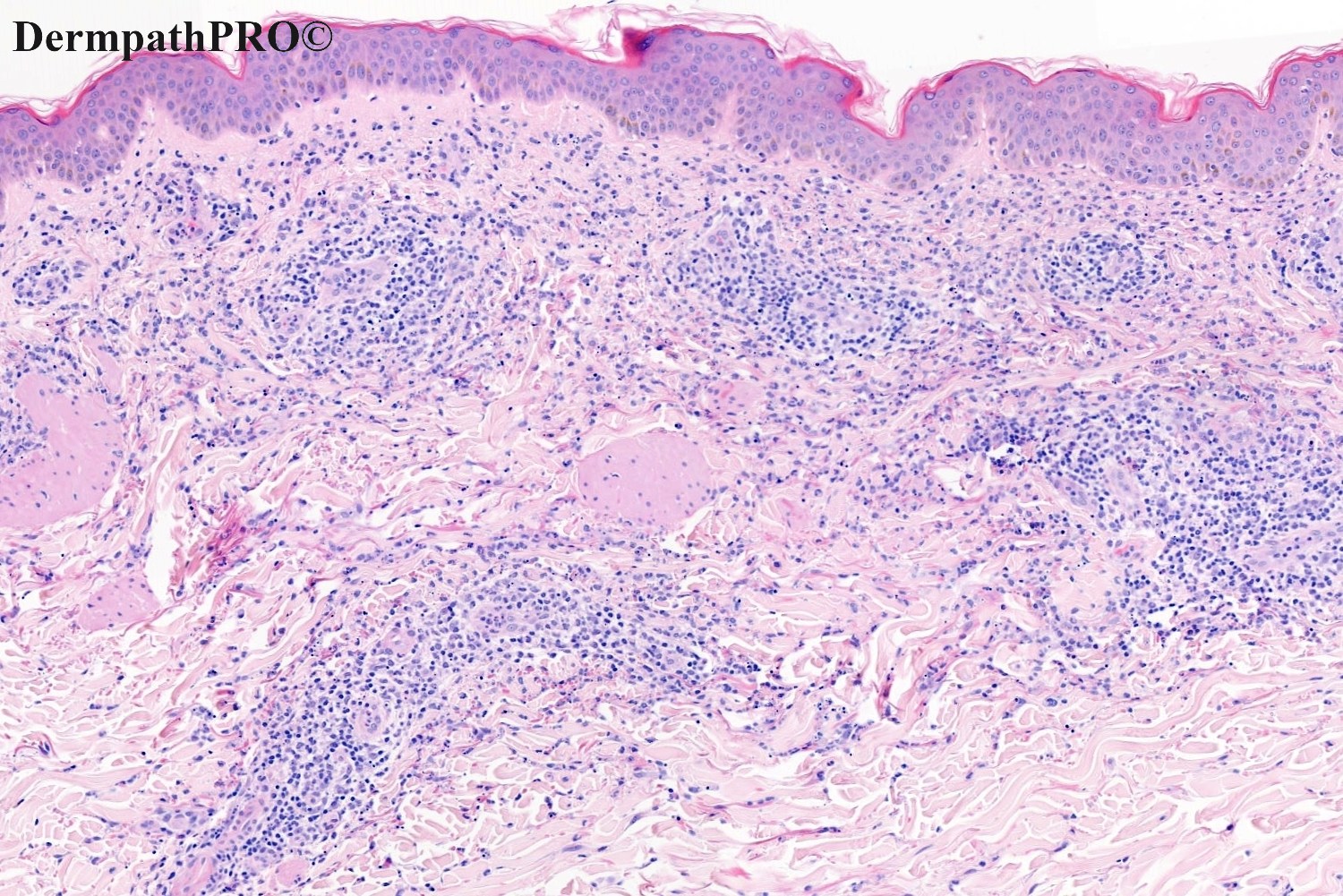
Case Number : Case 2686 - 22 October 2020 Posted By: Saleem Taibjee
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
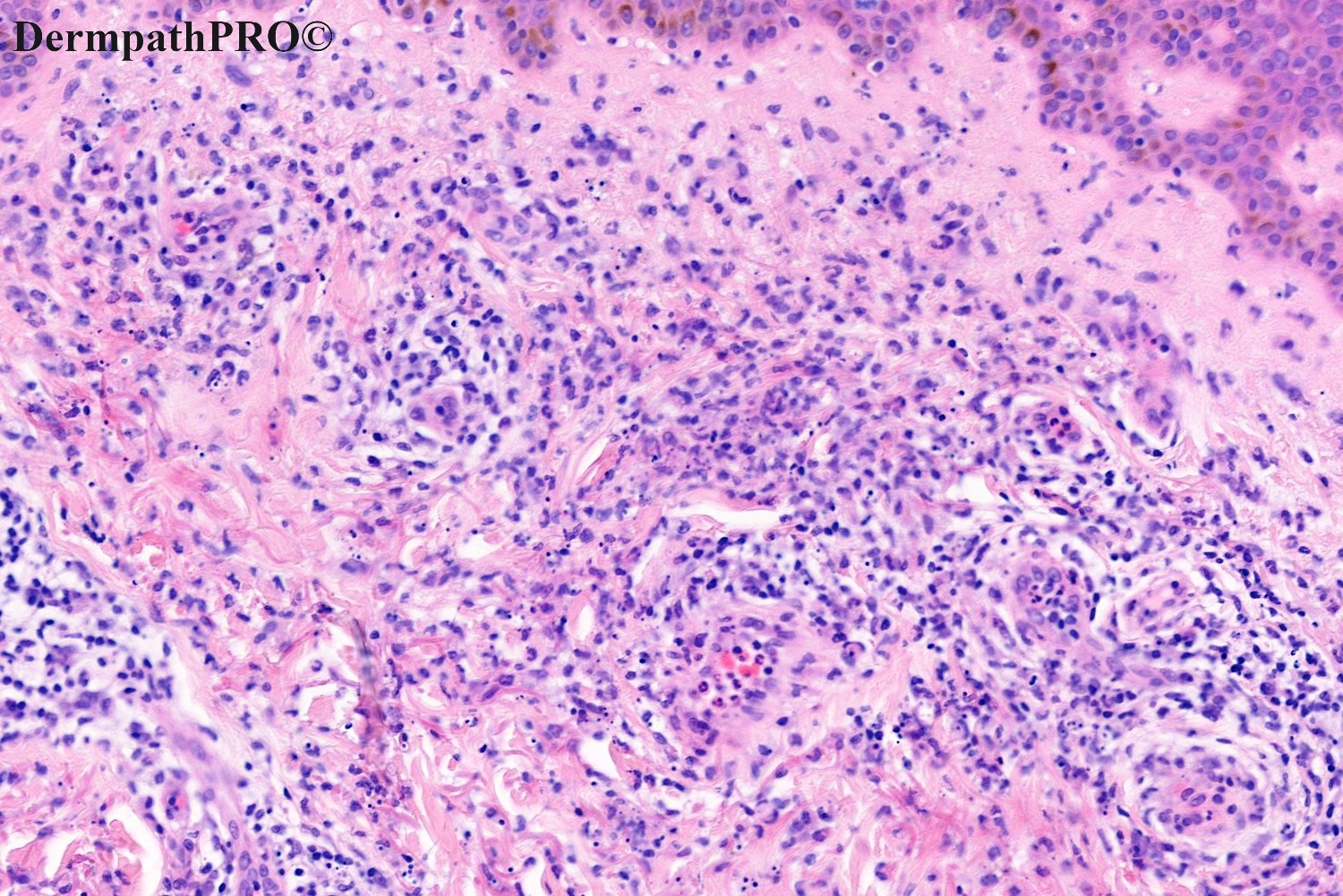
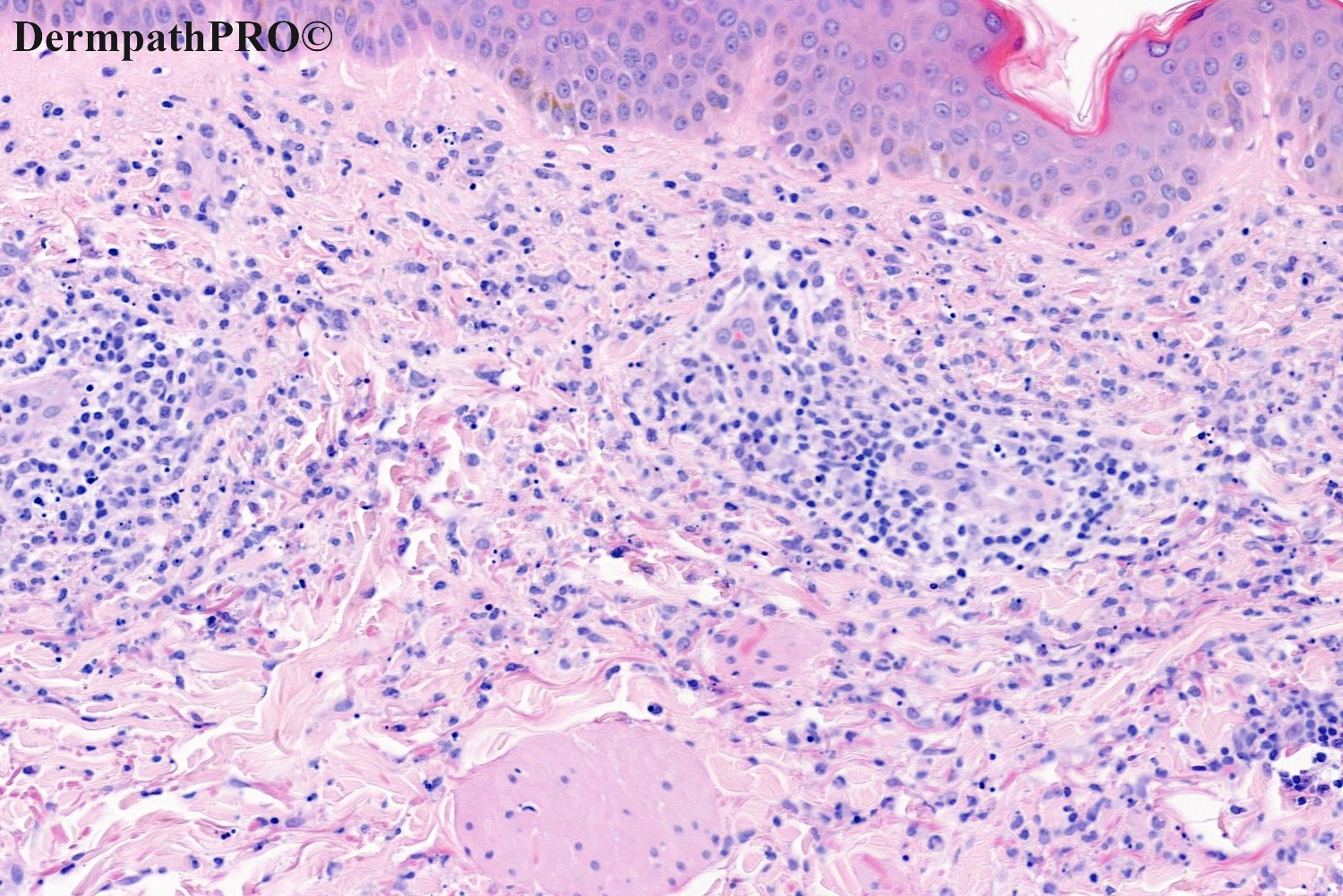
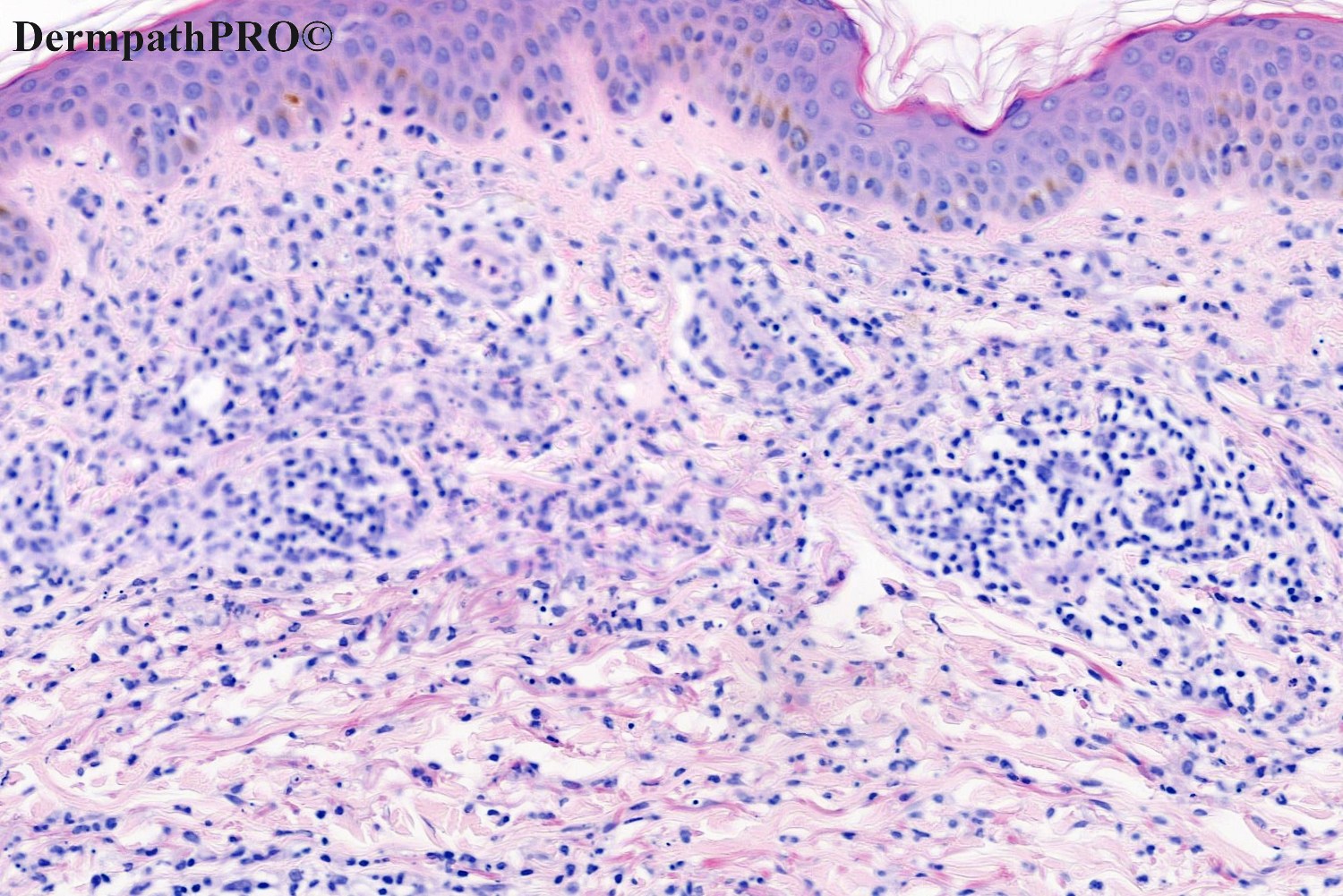
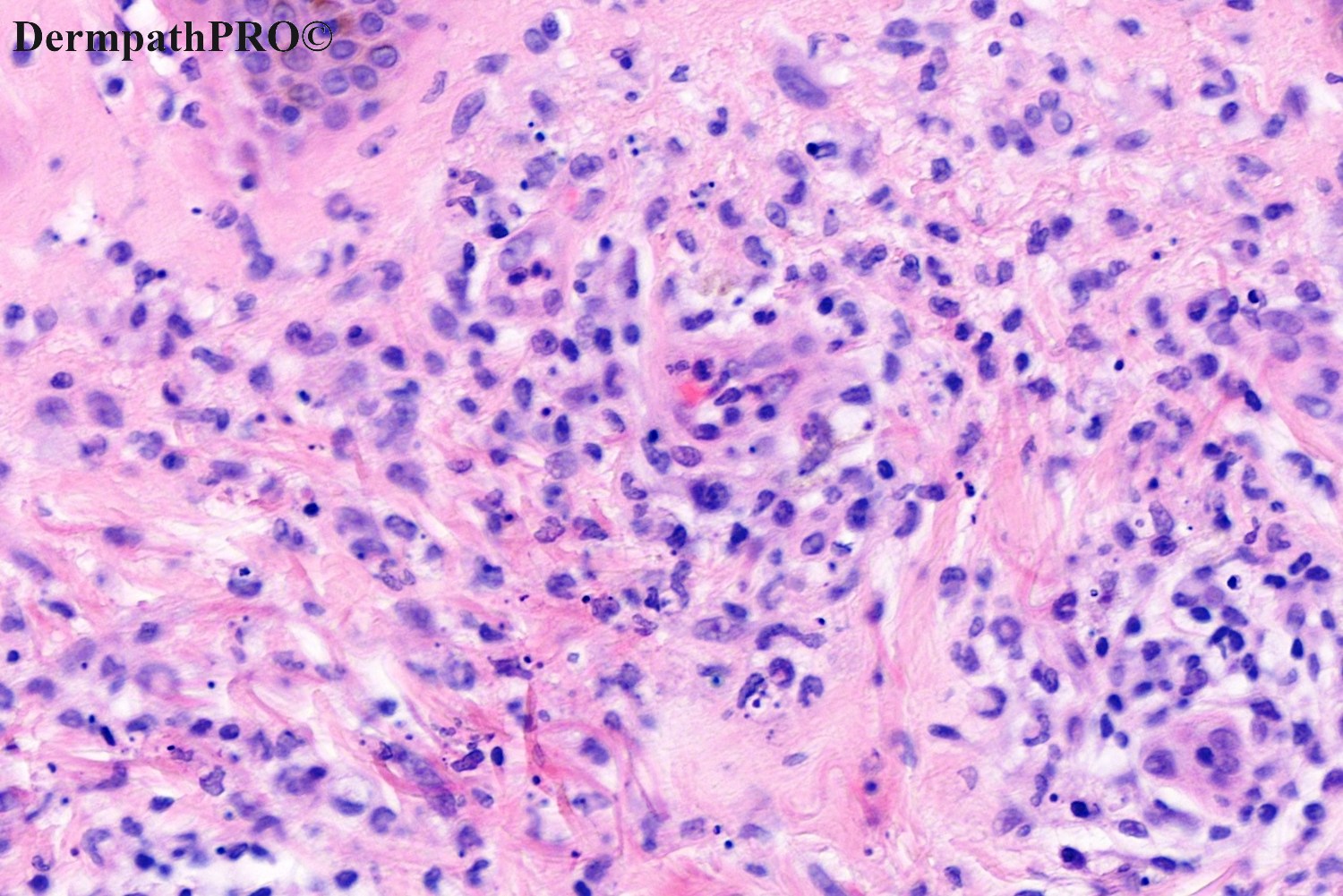
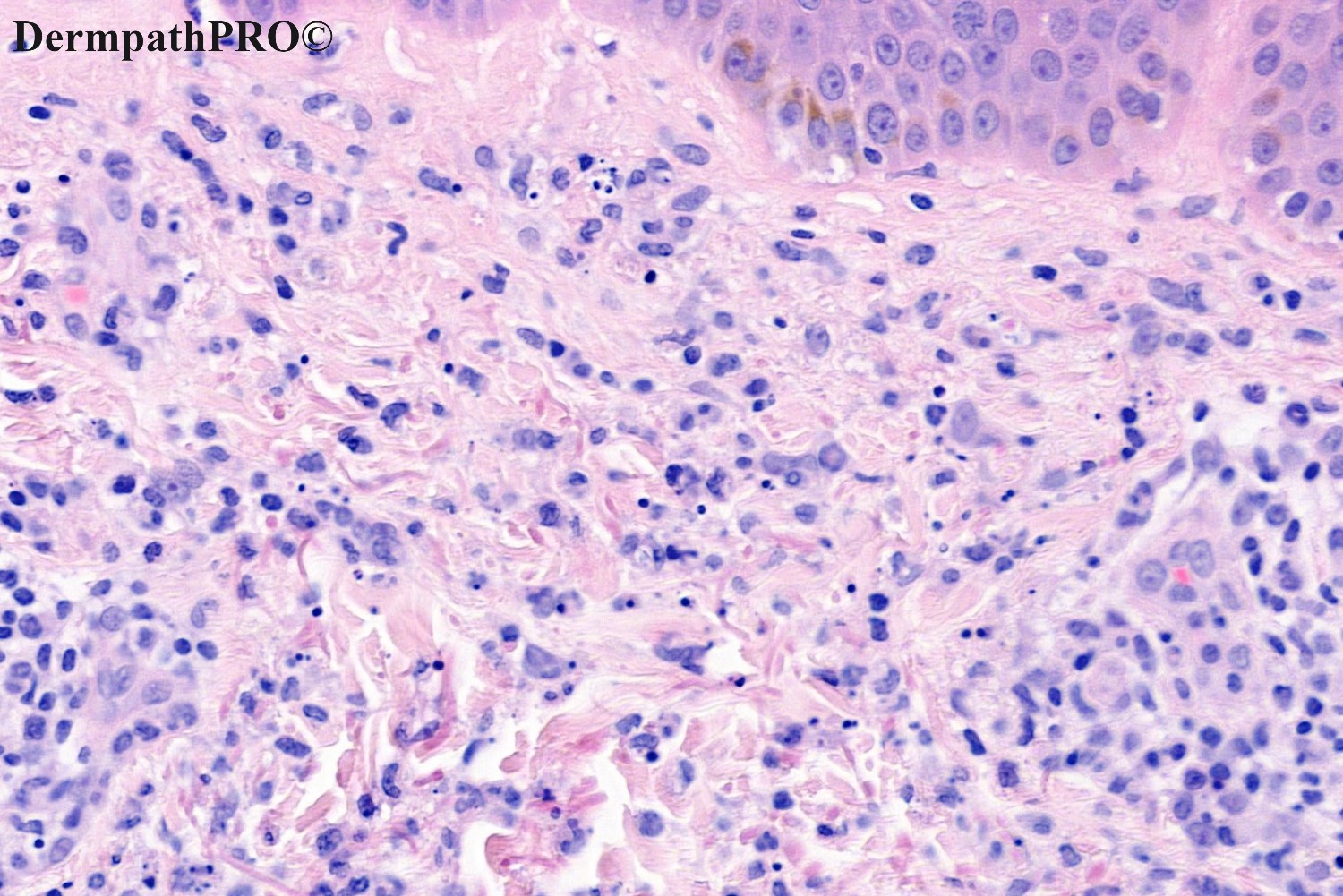
50M, Widespread rash. On etanercept for seronegative arthritis.




Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.