Case Number : Case 2807- 9 April 2021 Posted By: Dr. Richard Carr
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
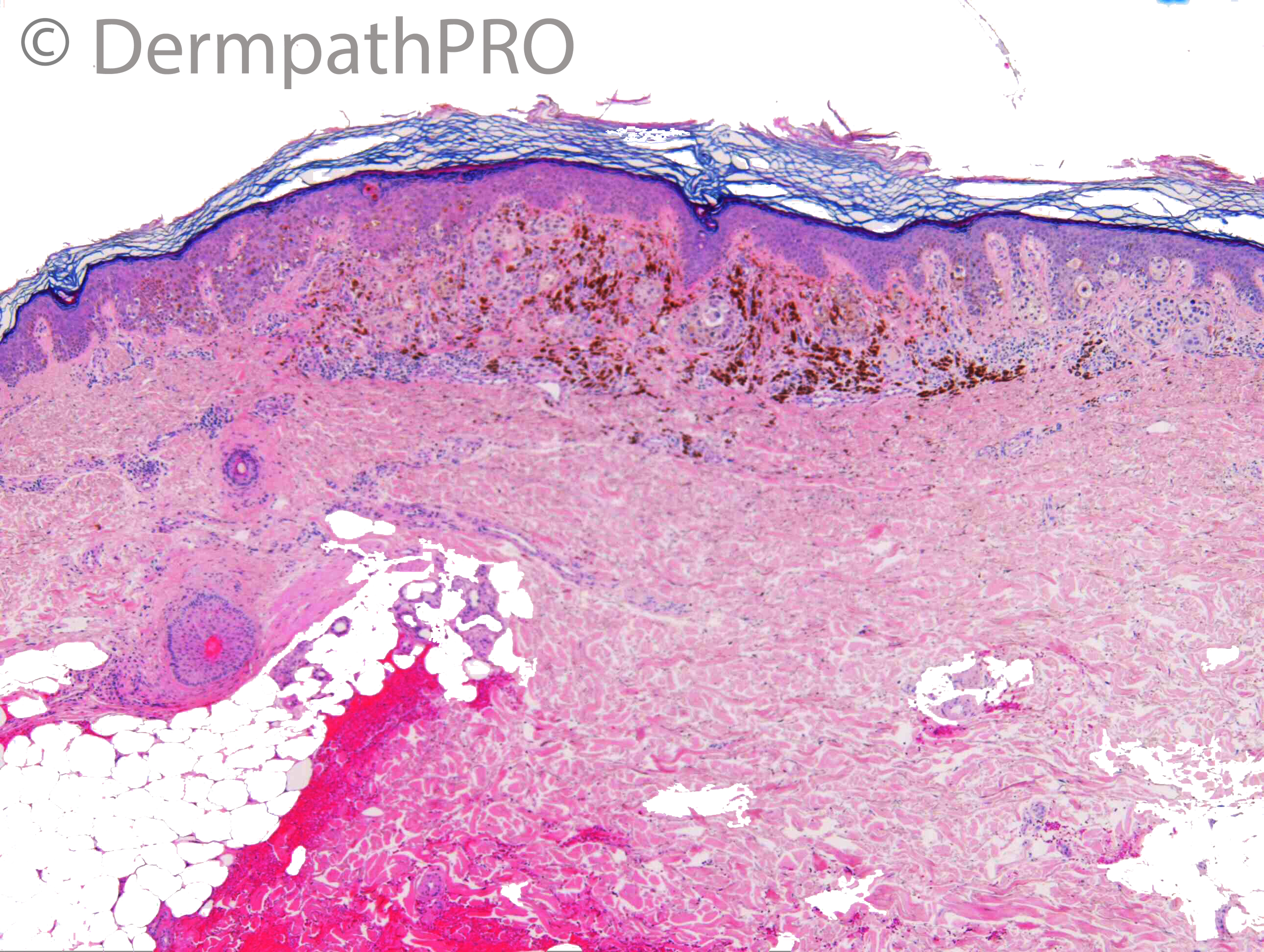
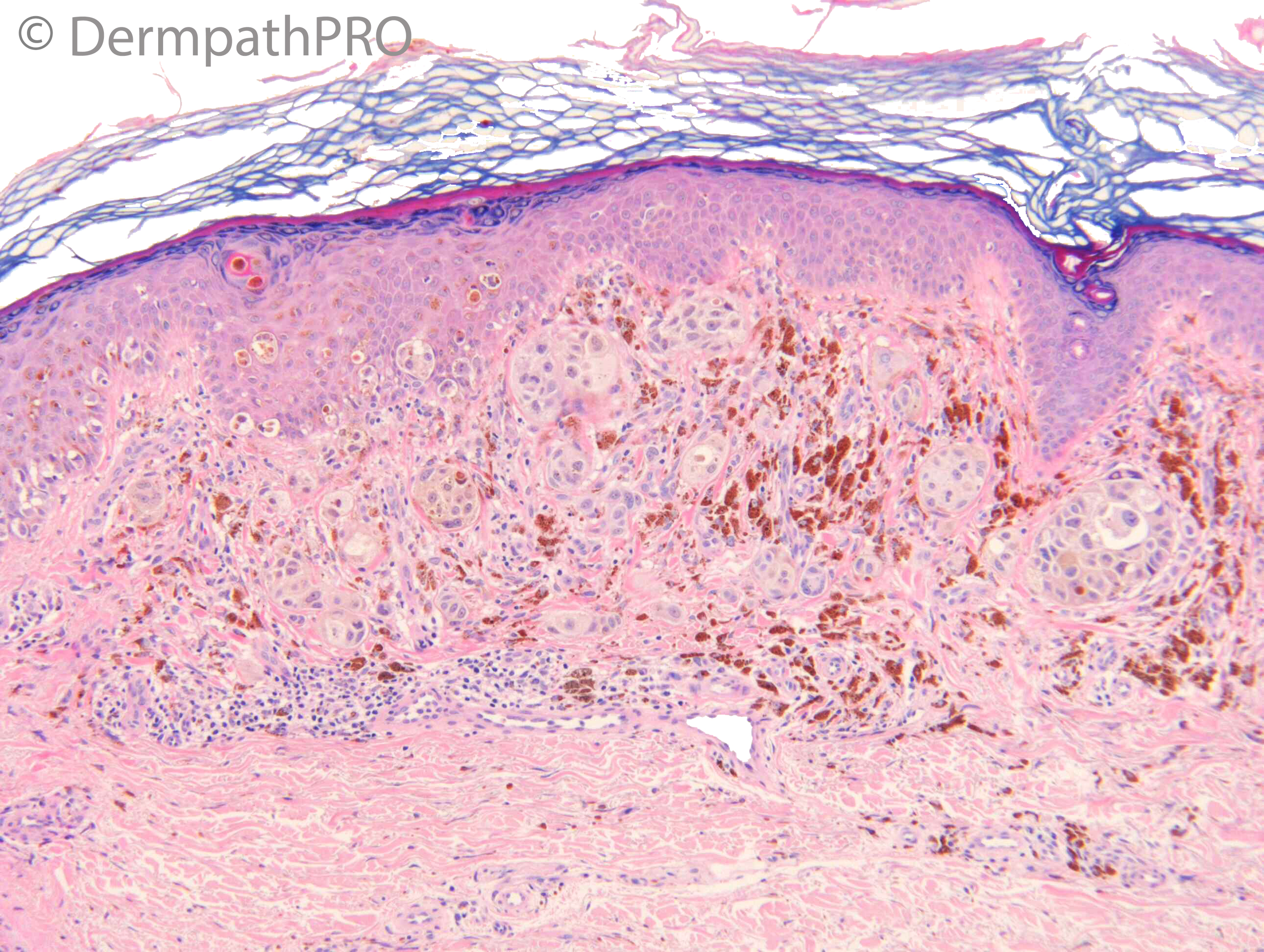
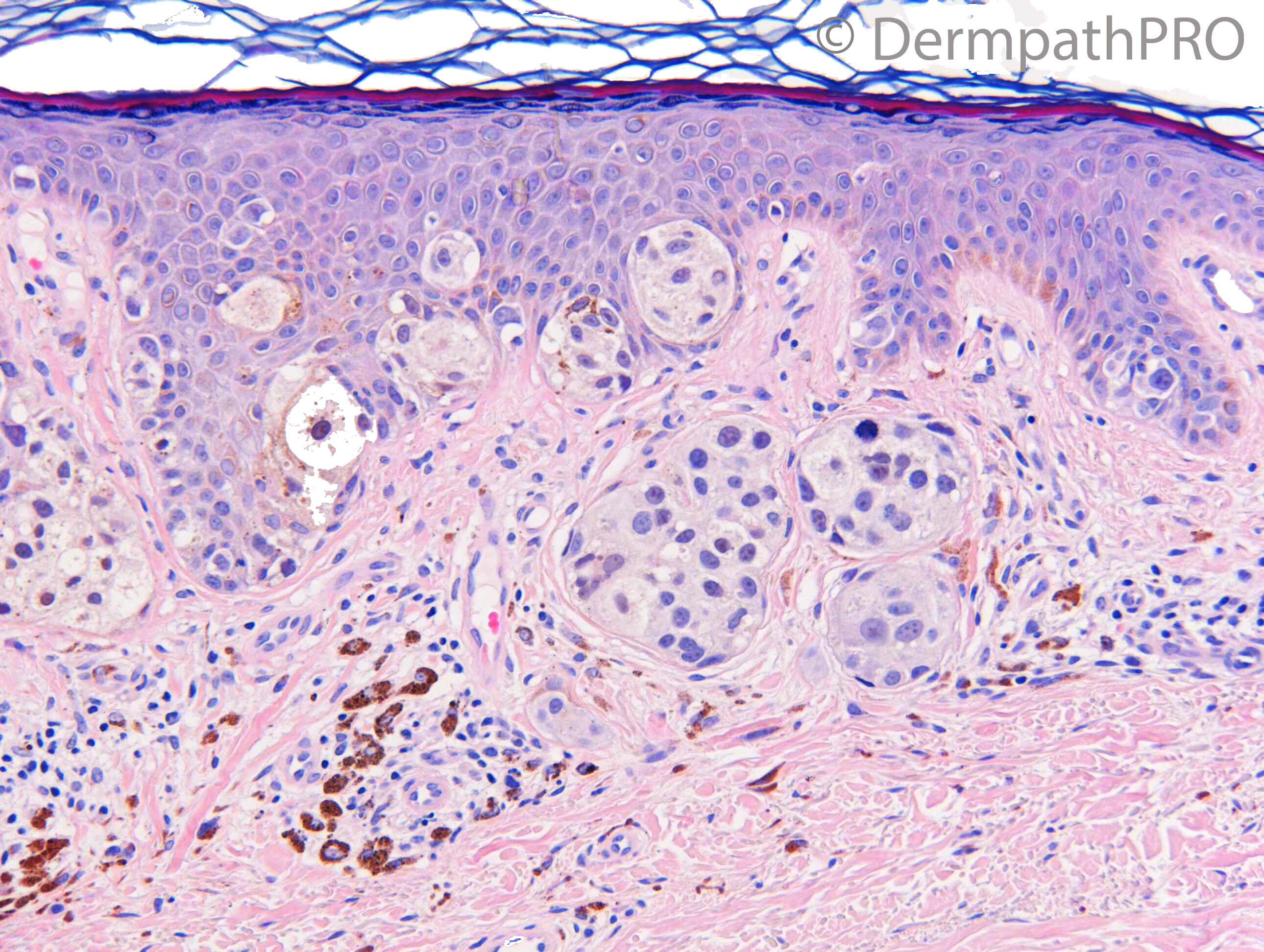
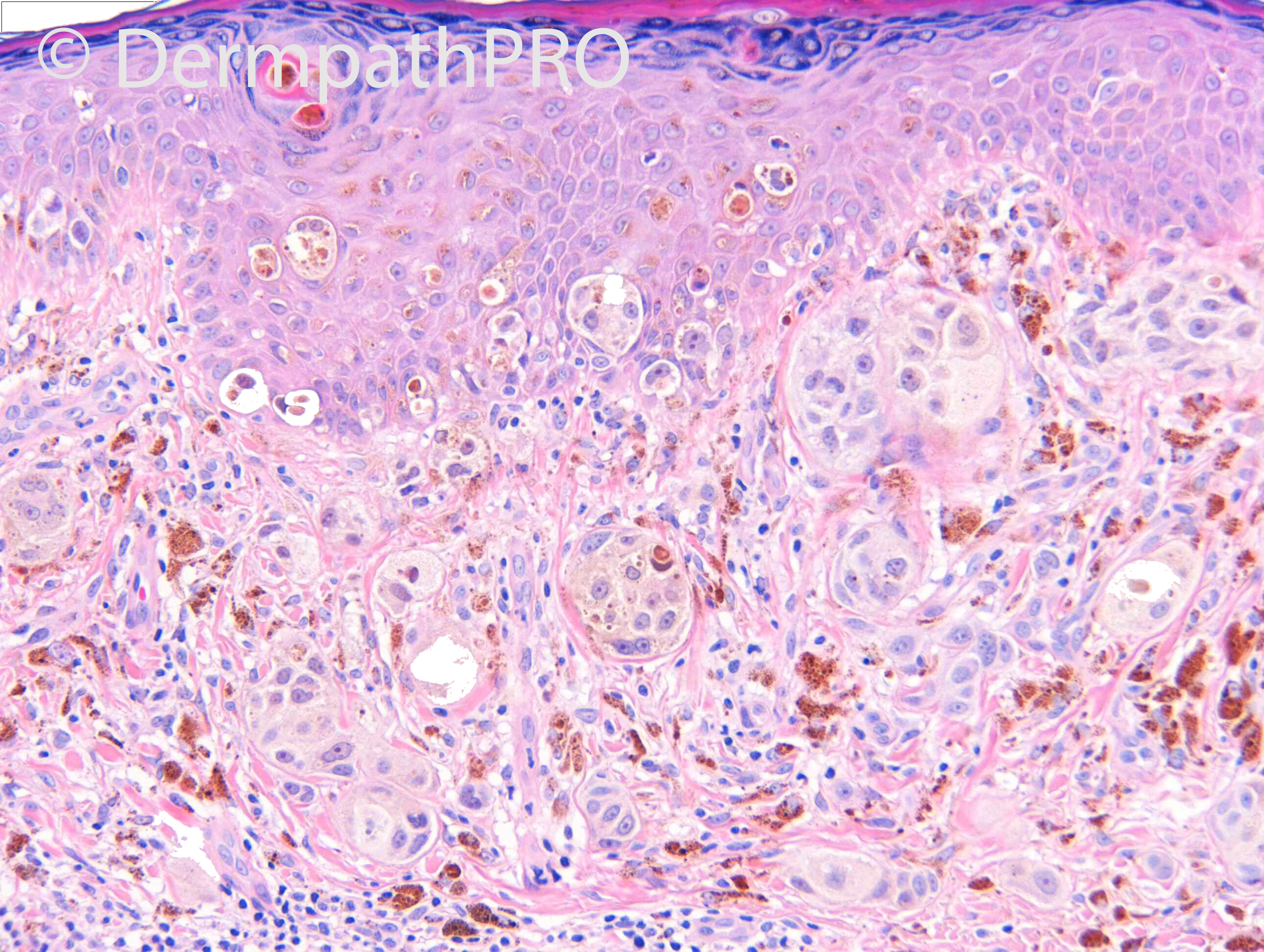
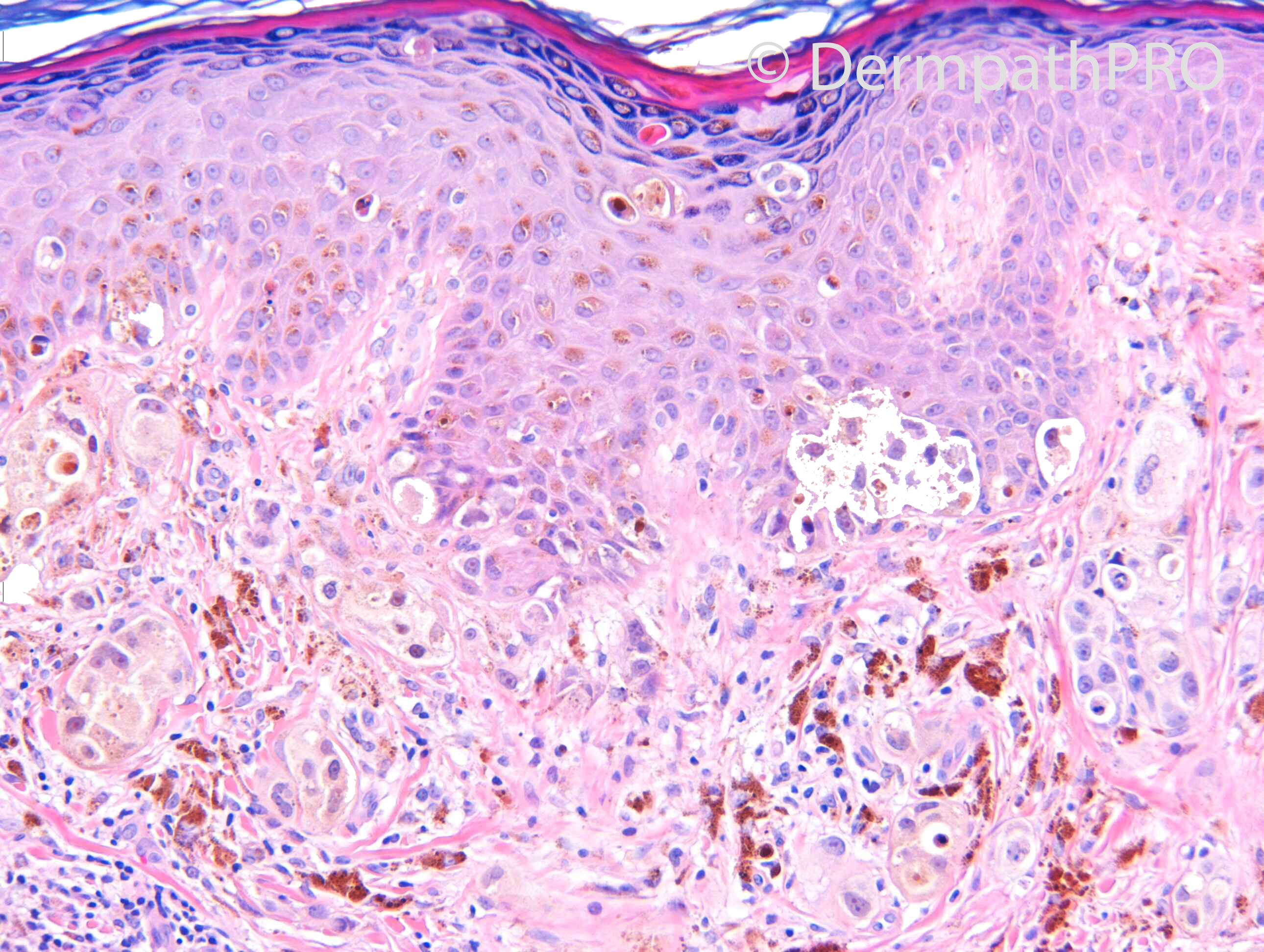
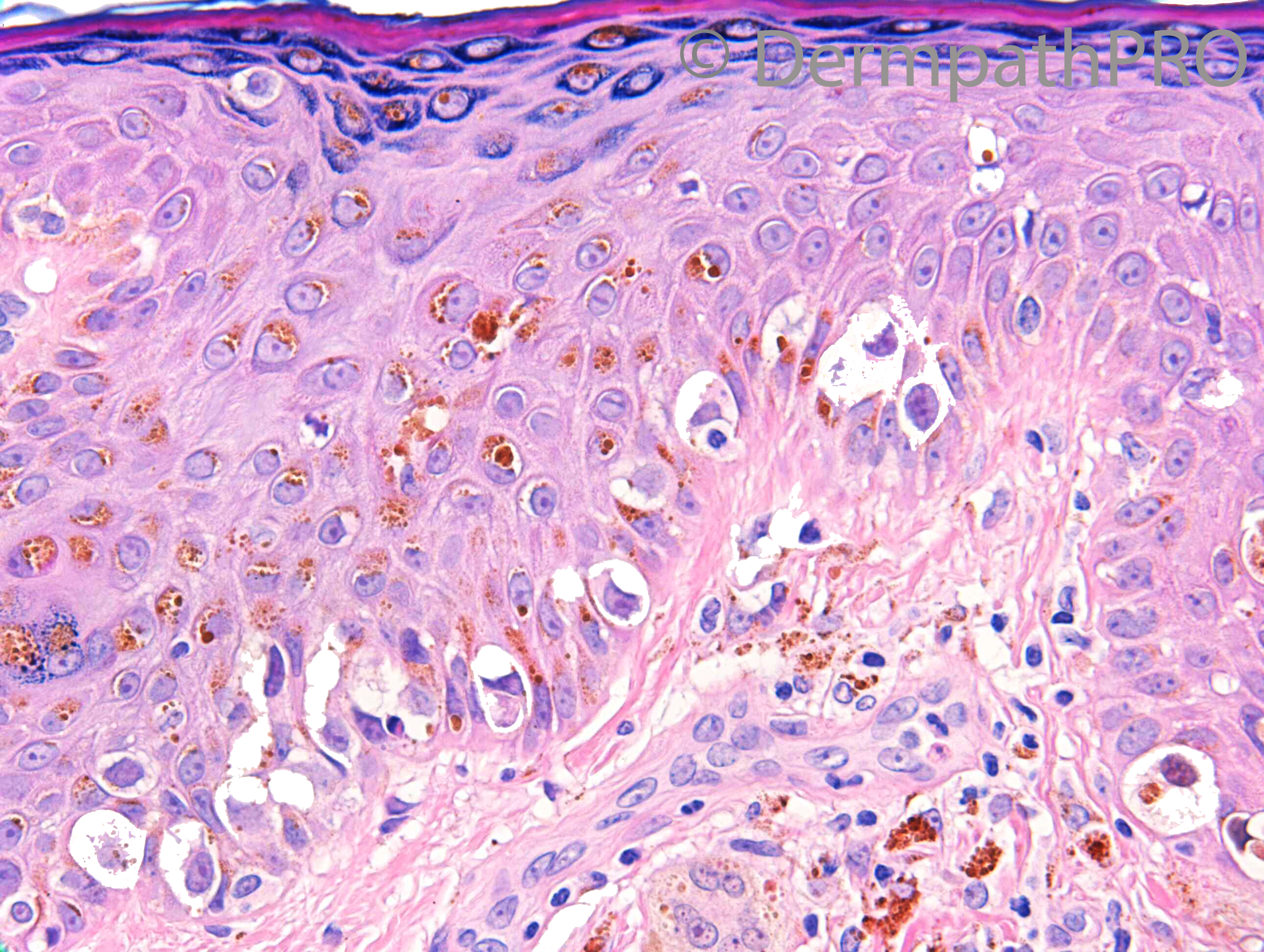
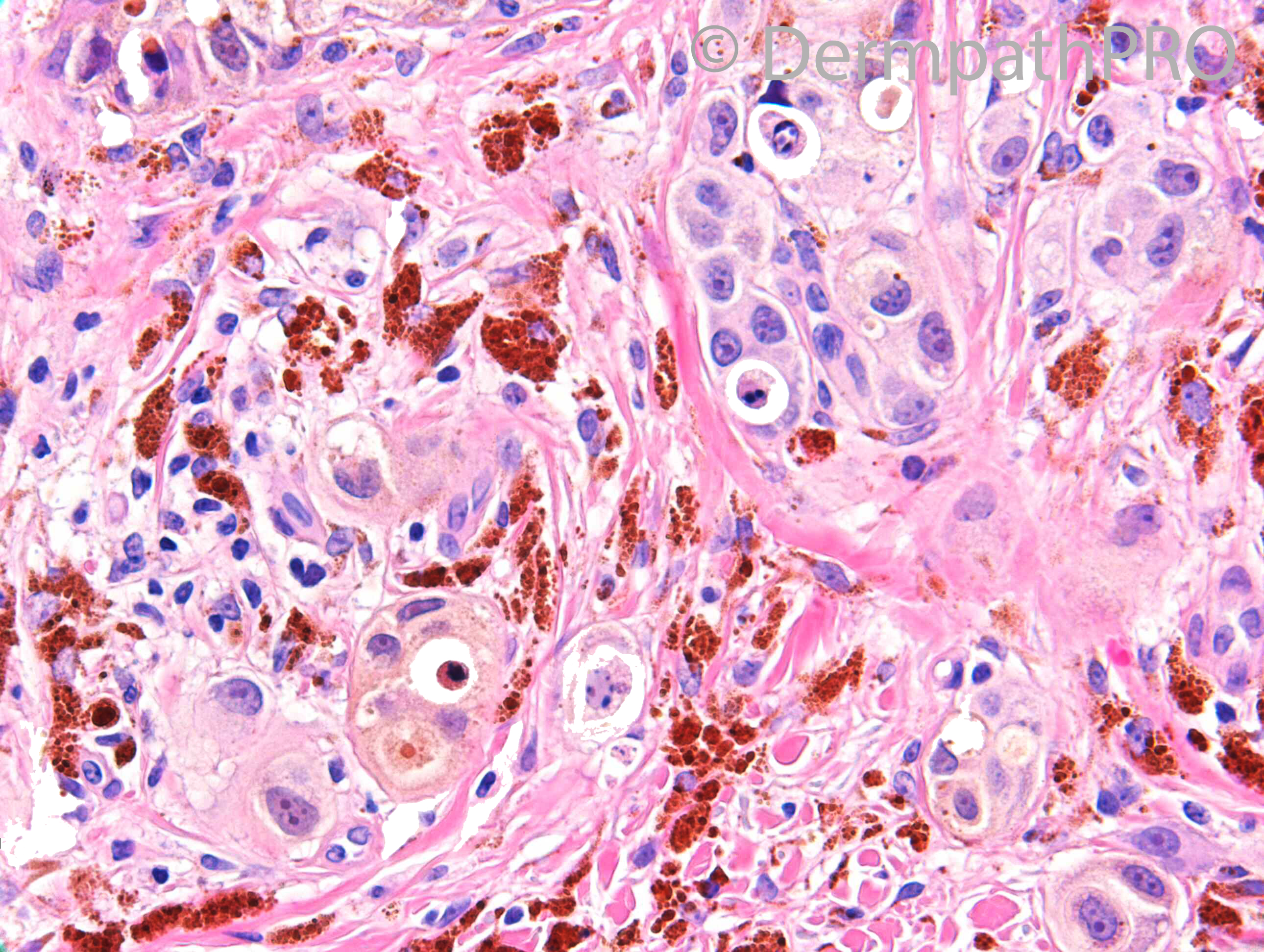
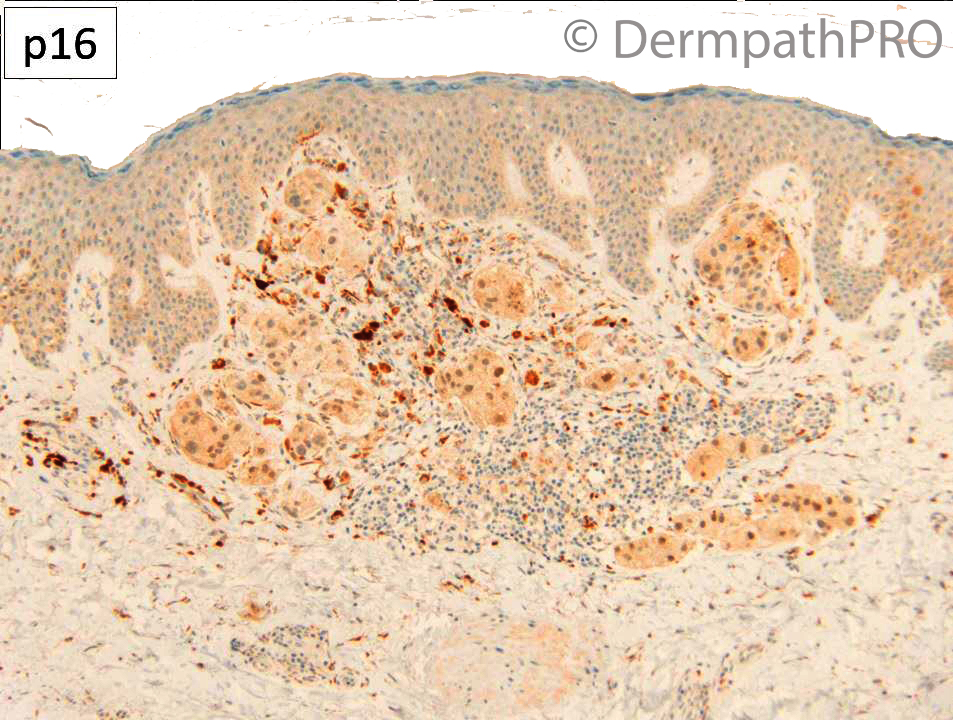
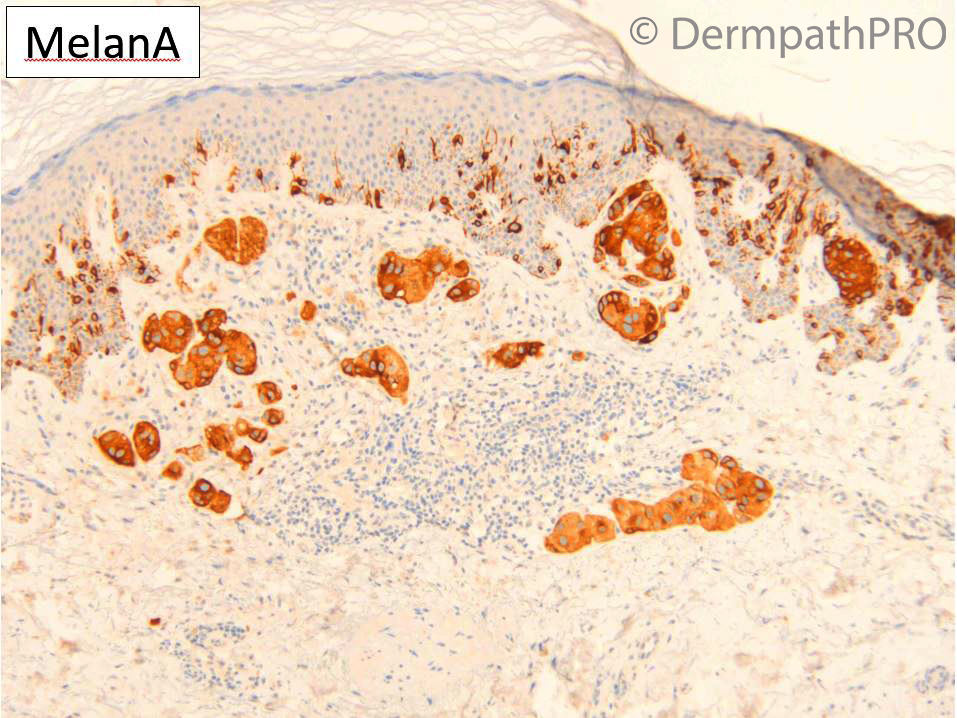
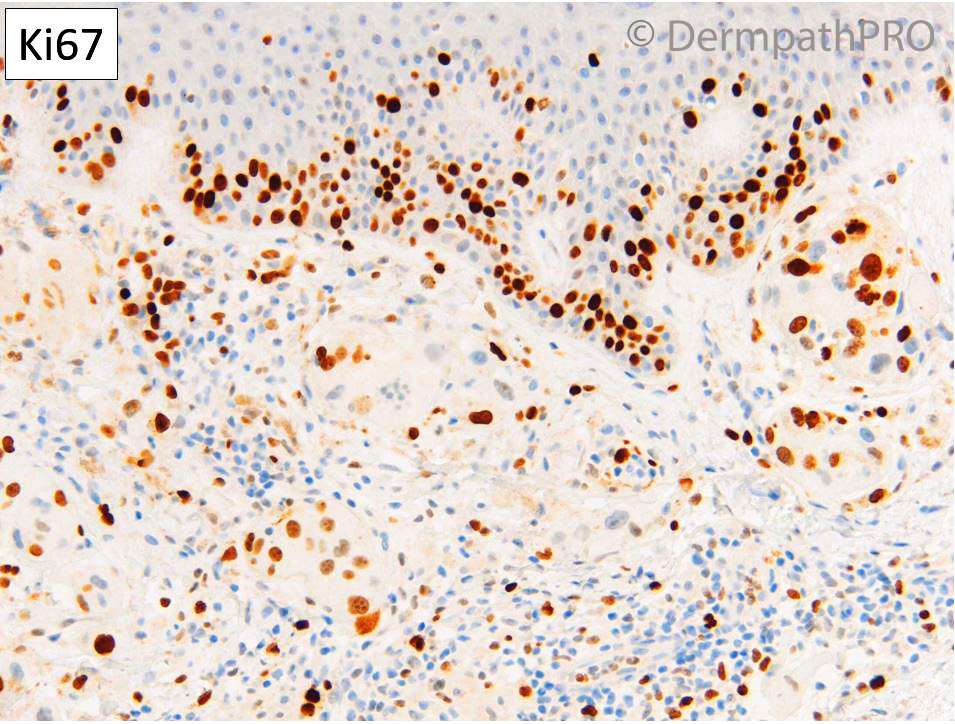
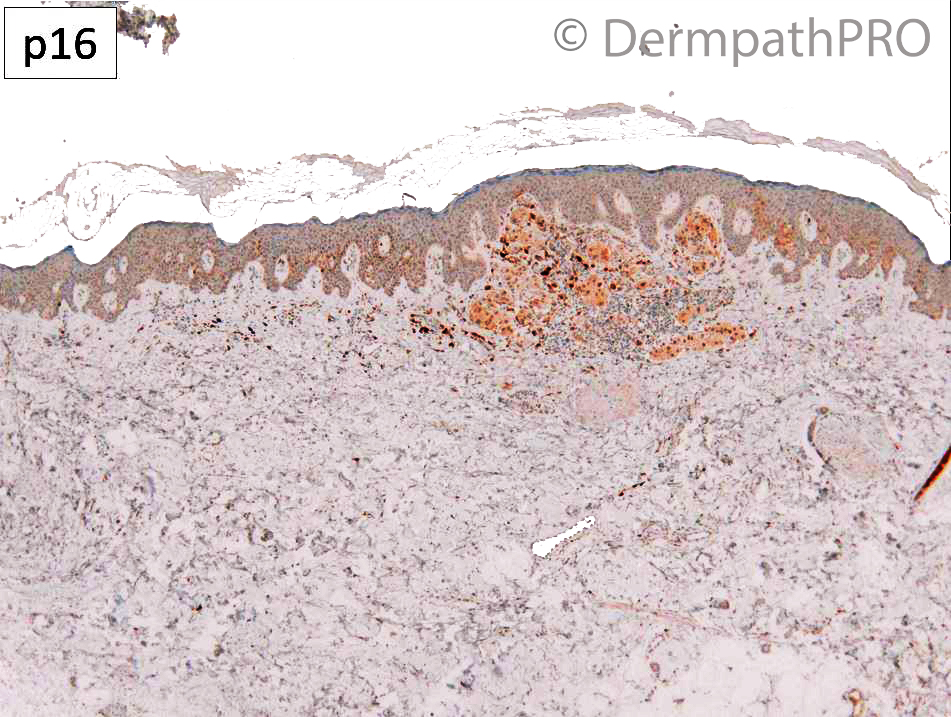
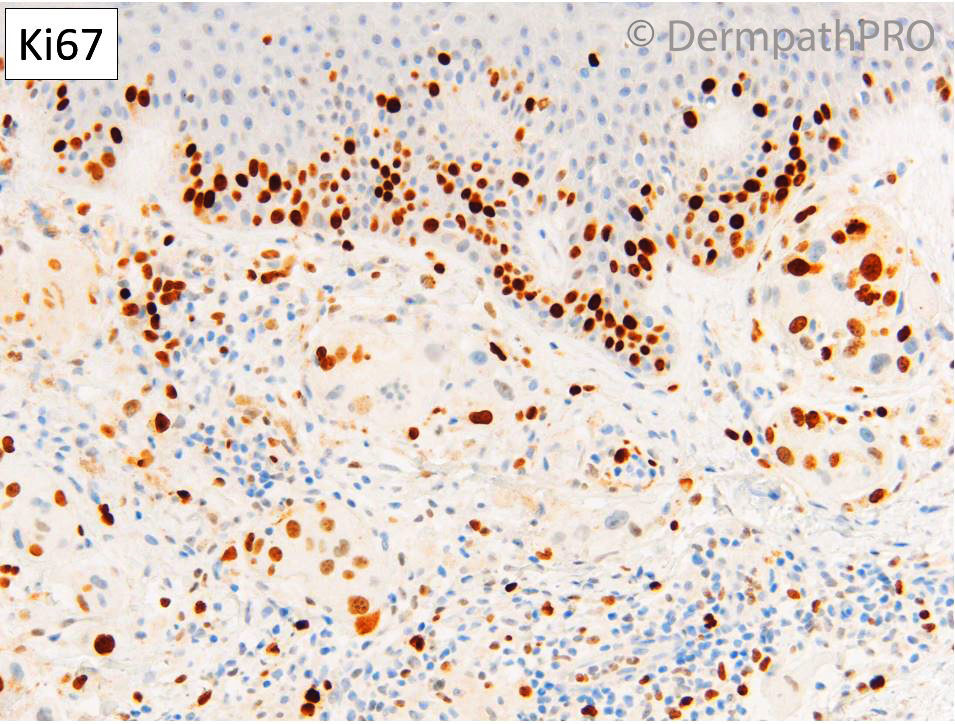
F60. Right lateral thigh. 1 year history of a darkly pigmented cutaneous nodule. ?MM, ?Dermatofibroma.
H&Ex8; IHCx5 at 6pm please
H&Ex8; IHCx5 at 6pm please

Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.