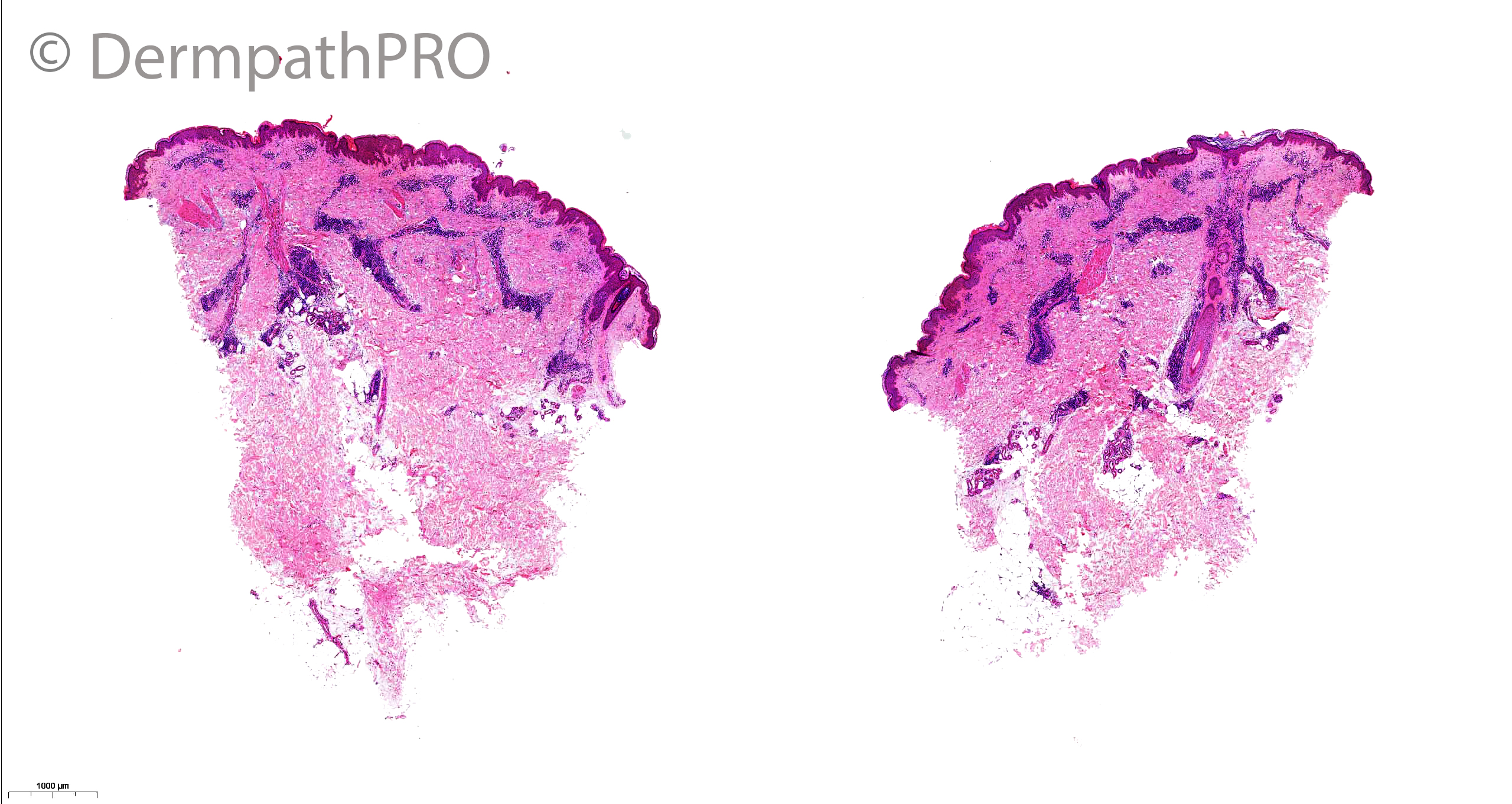
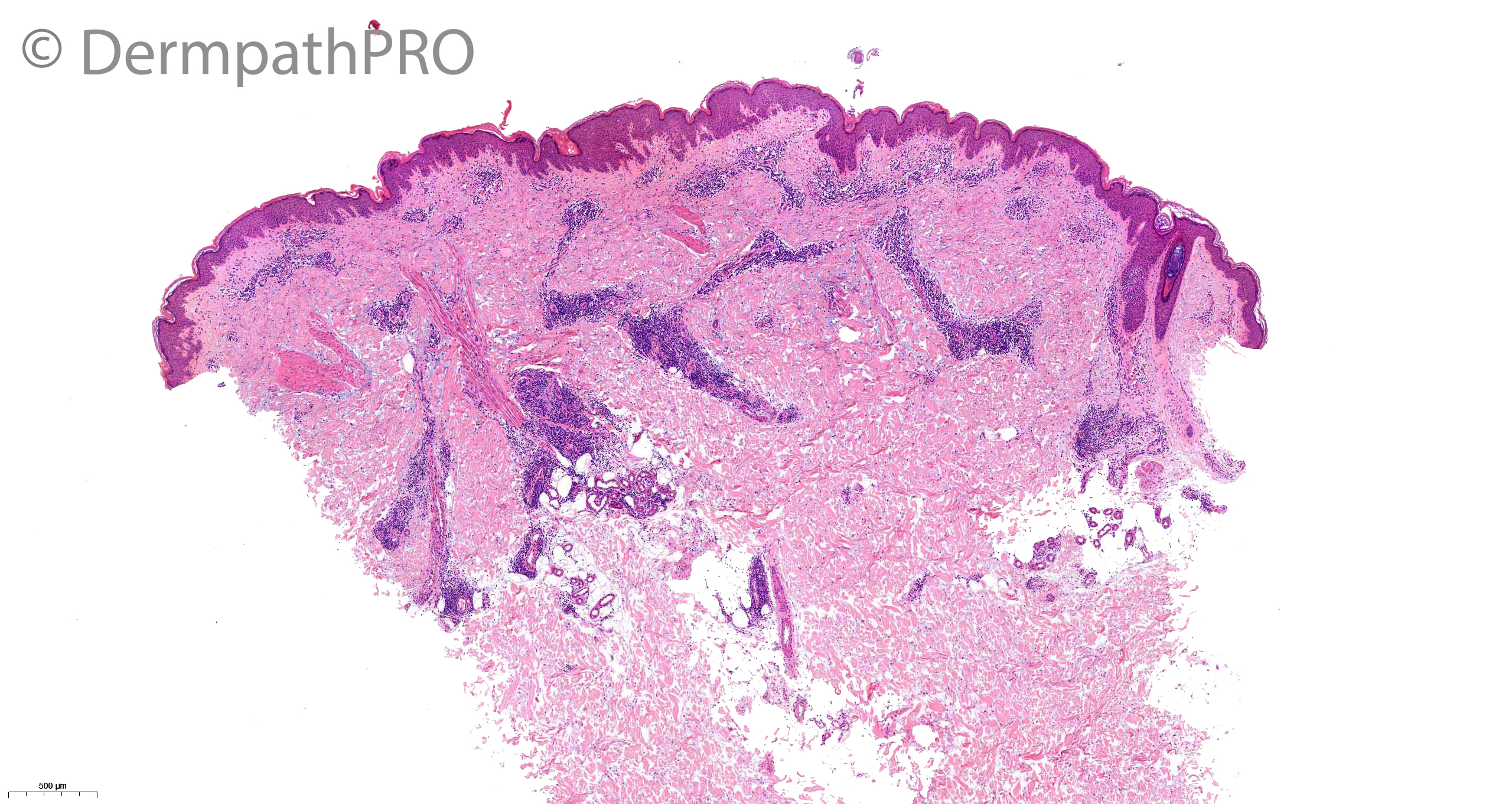
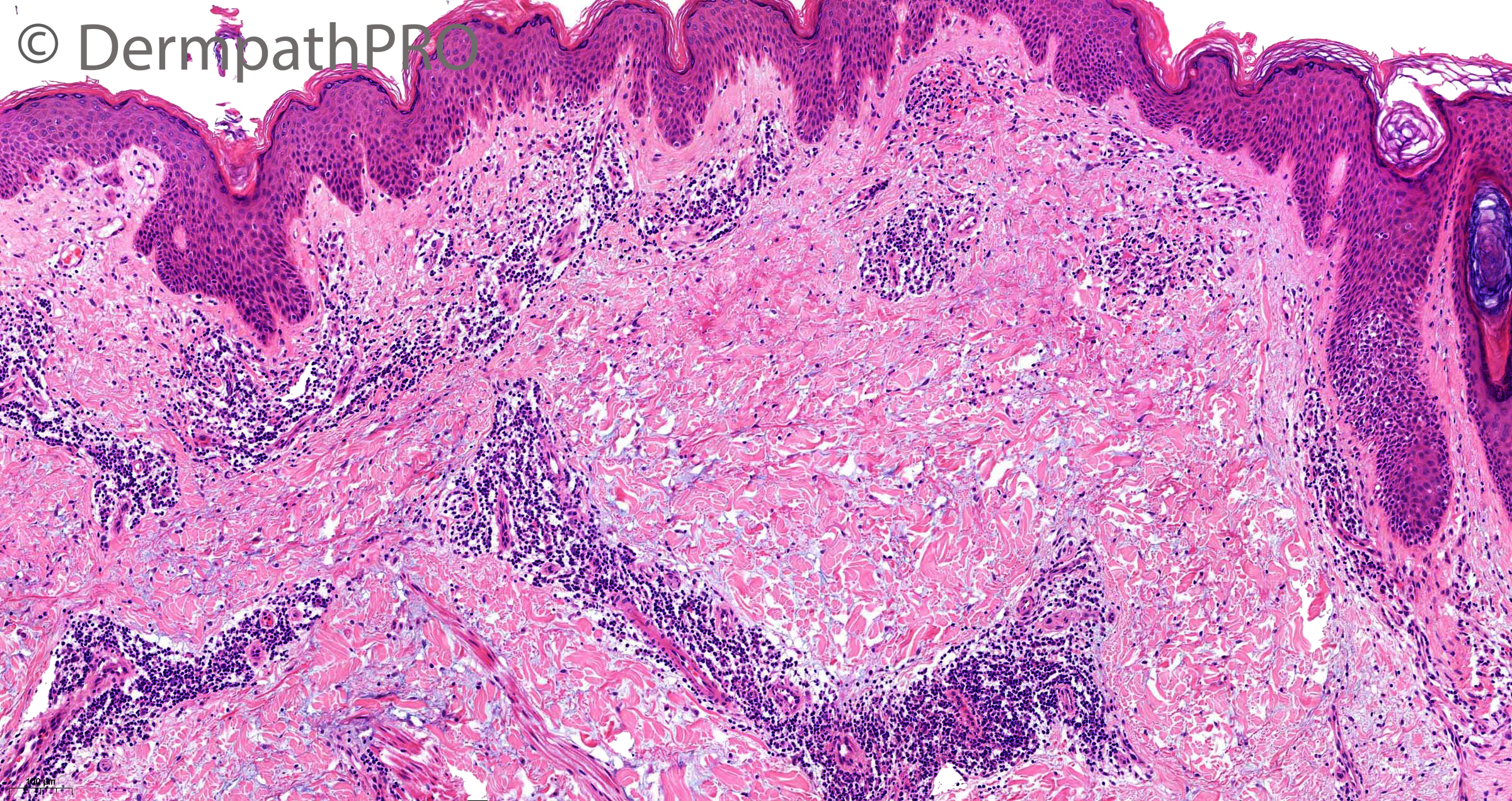
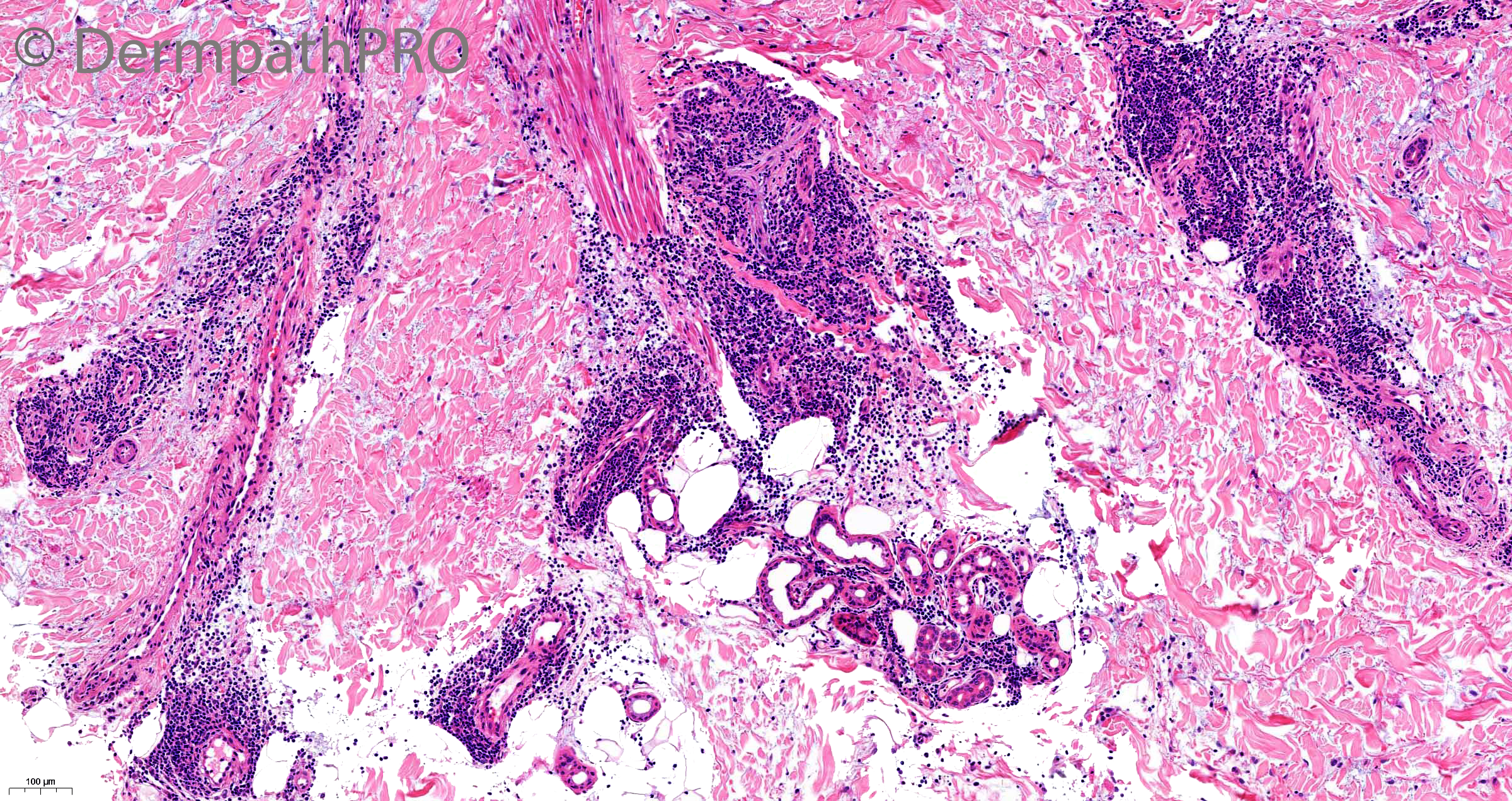
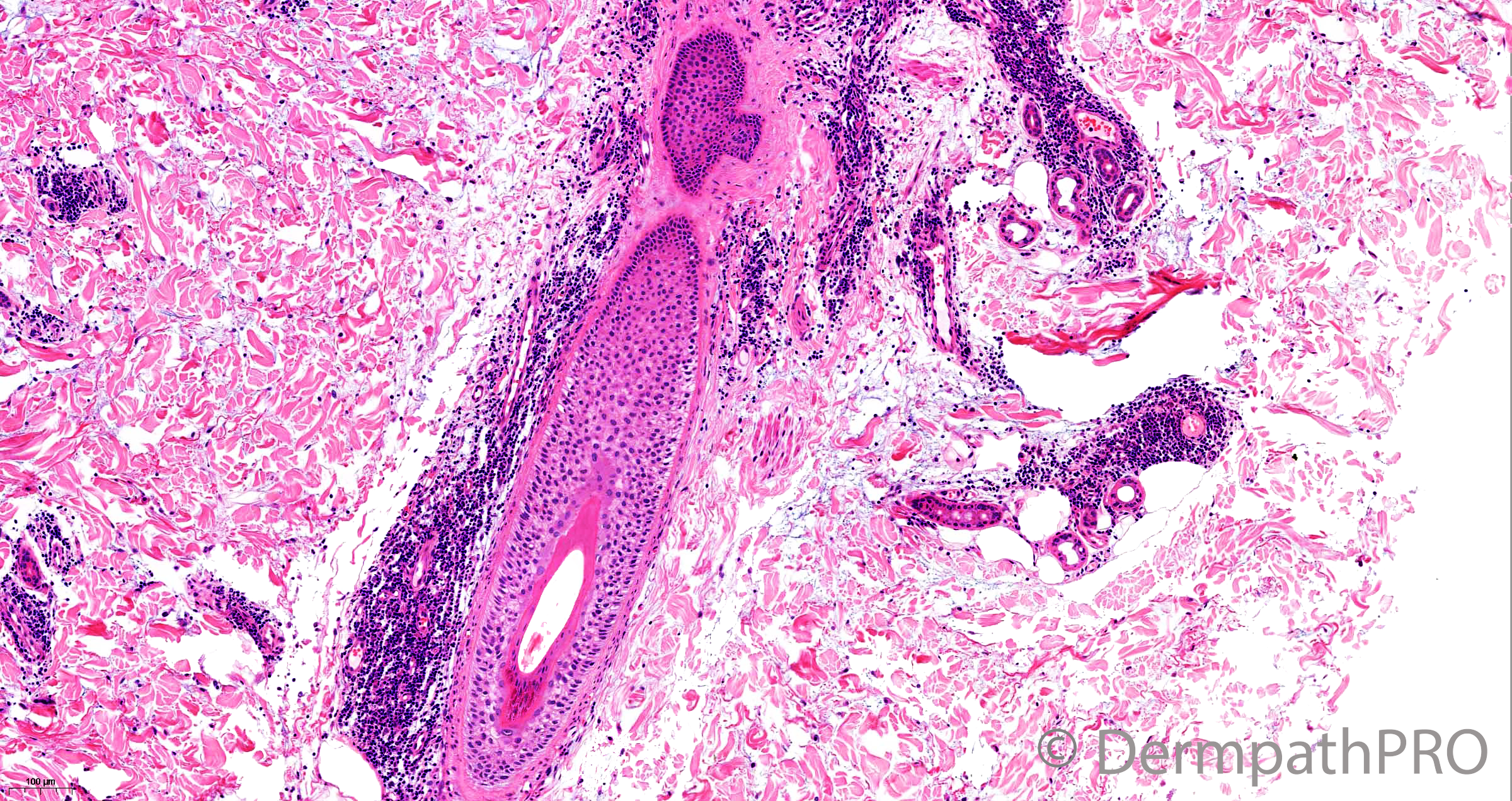
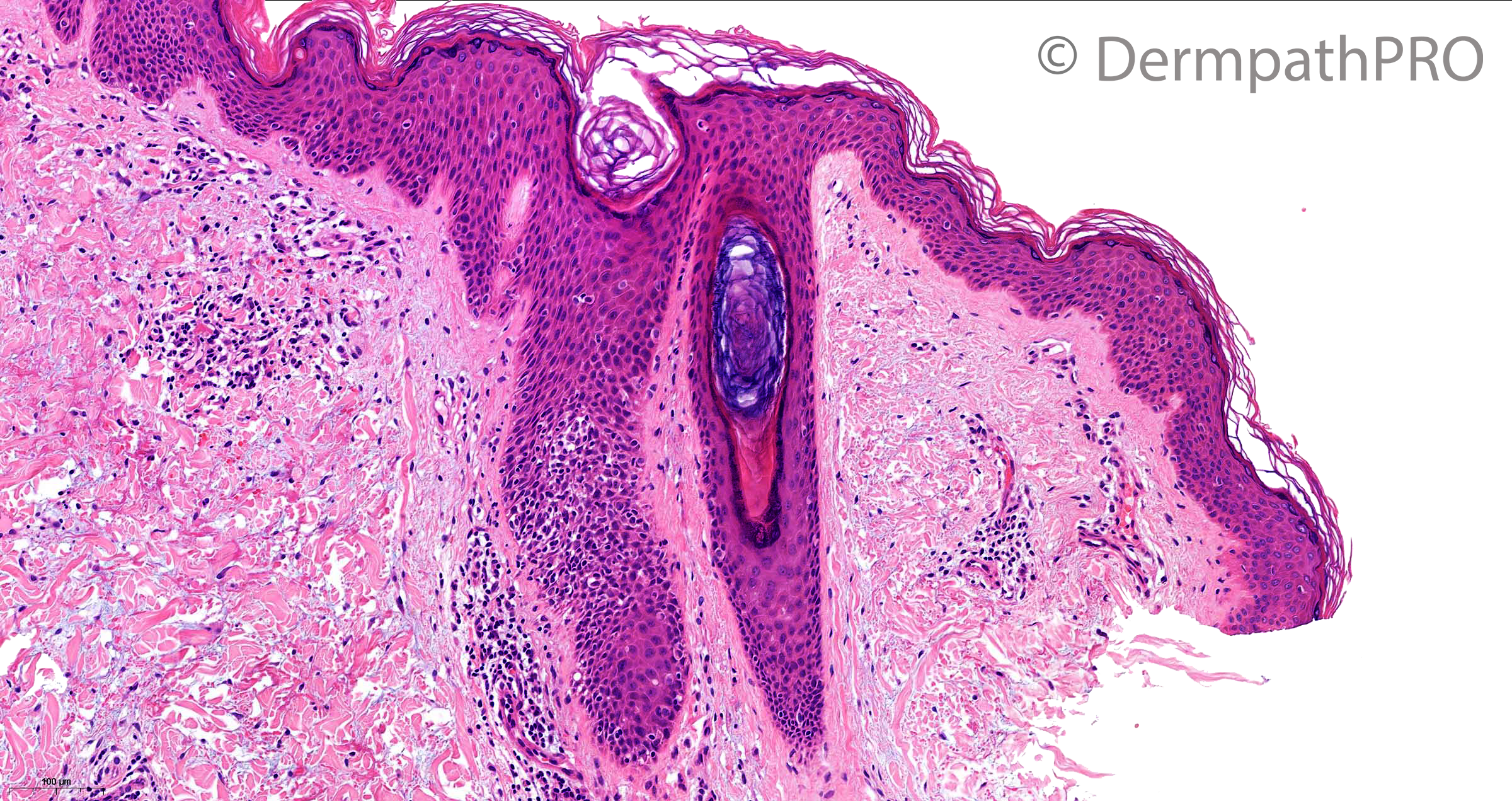
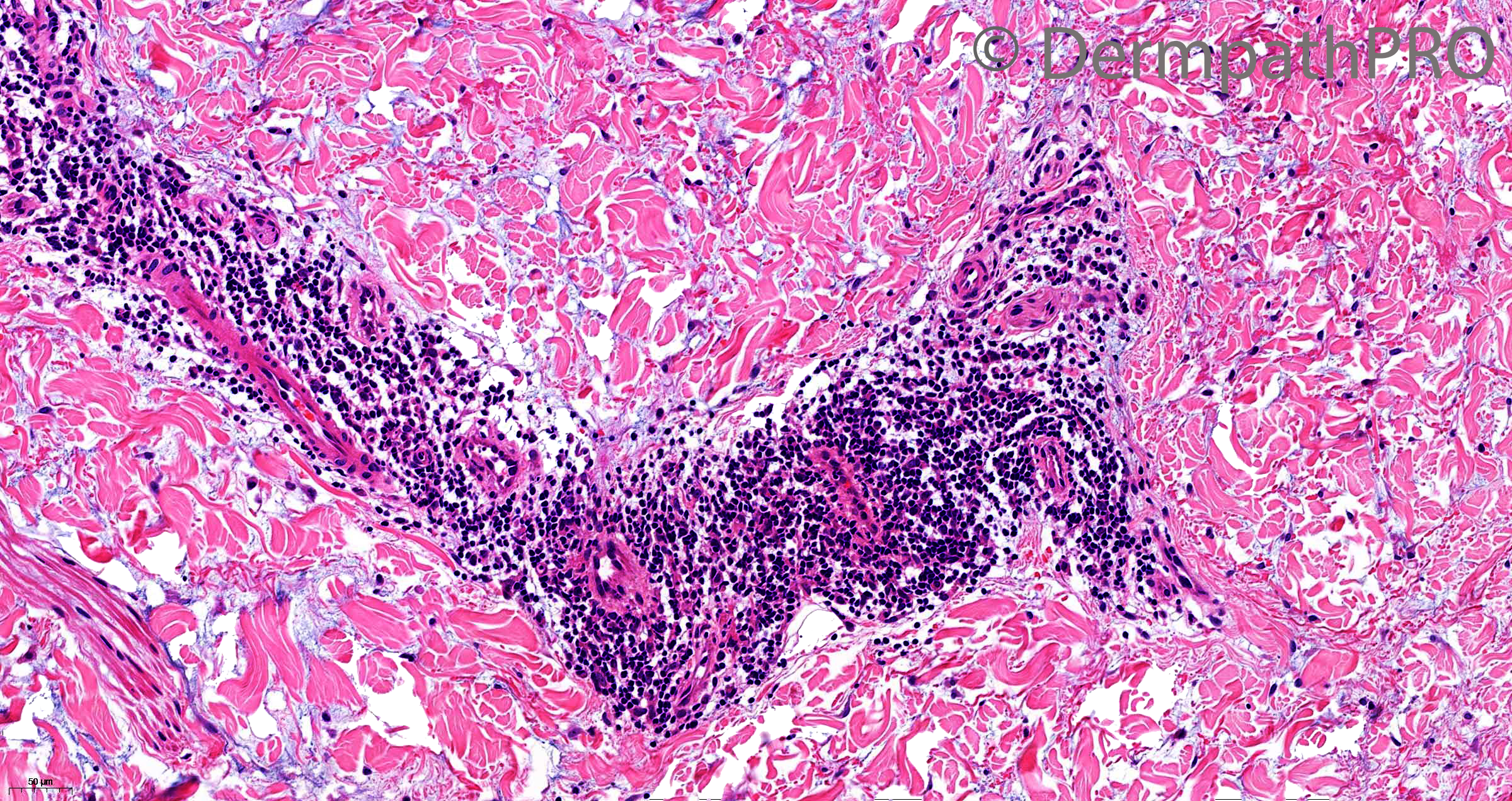
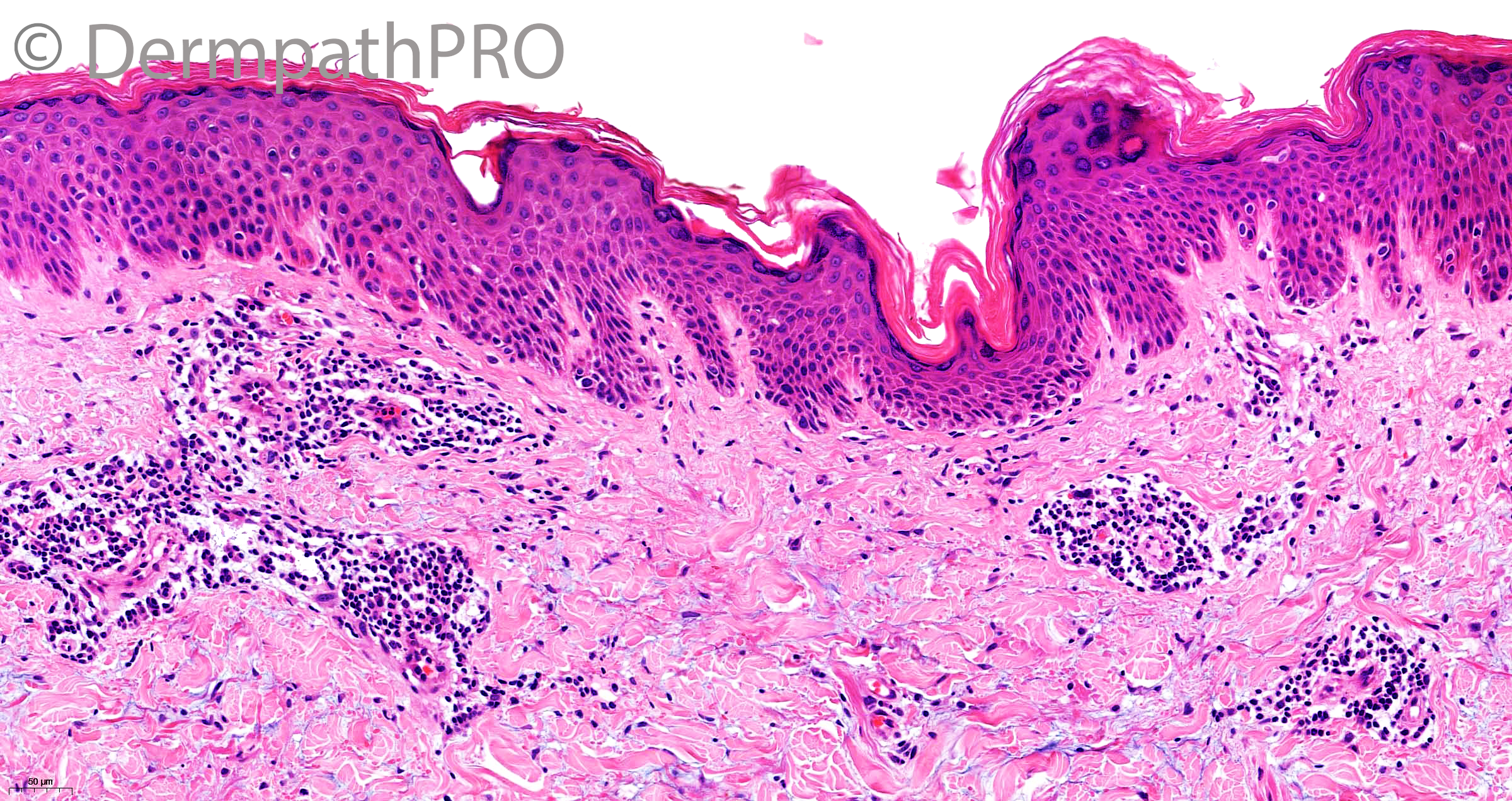
Case Number : Case 2821- 29 April 2021 Posted By: Saleem Taibjee
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
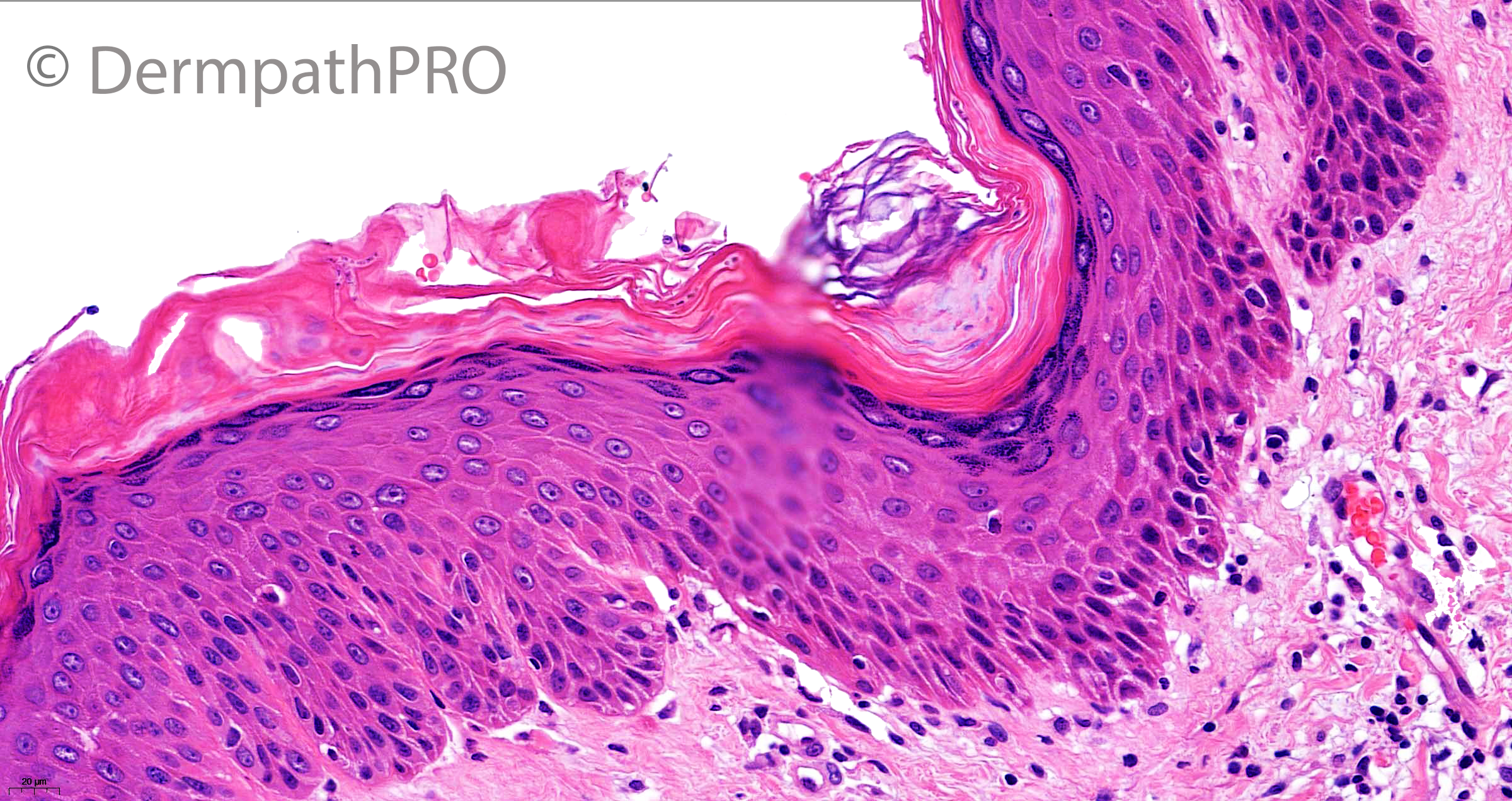
38F, itchy erythematous rash

Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.