Case Number : Case 2976 - 2 December 2021 Posted By: Saleem Taibjee
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
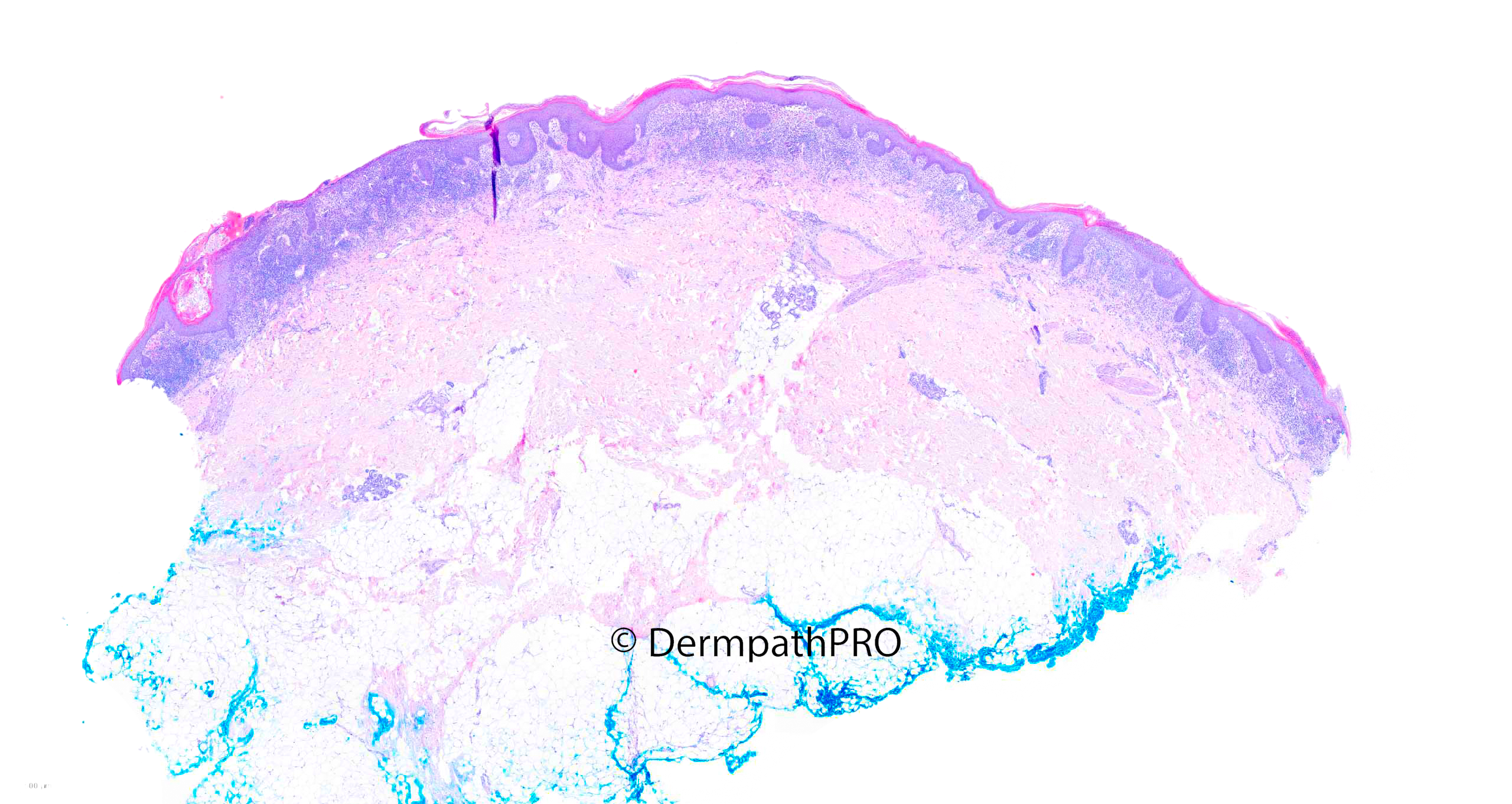
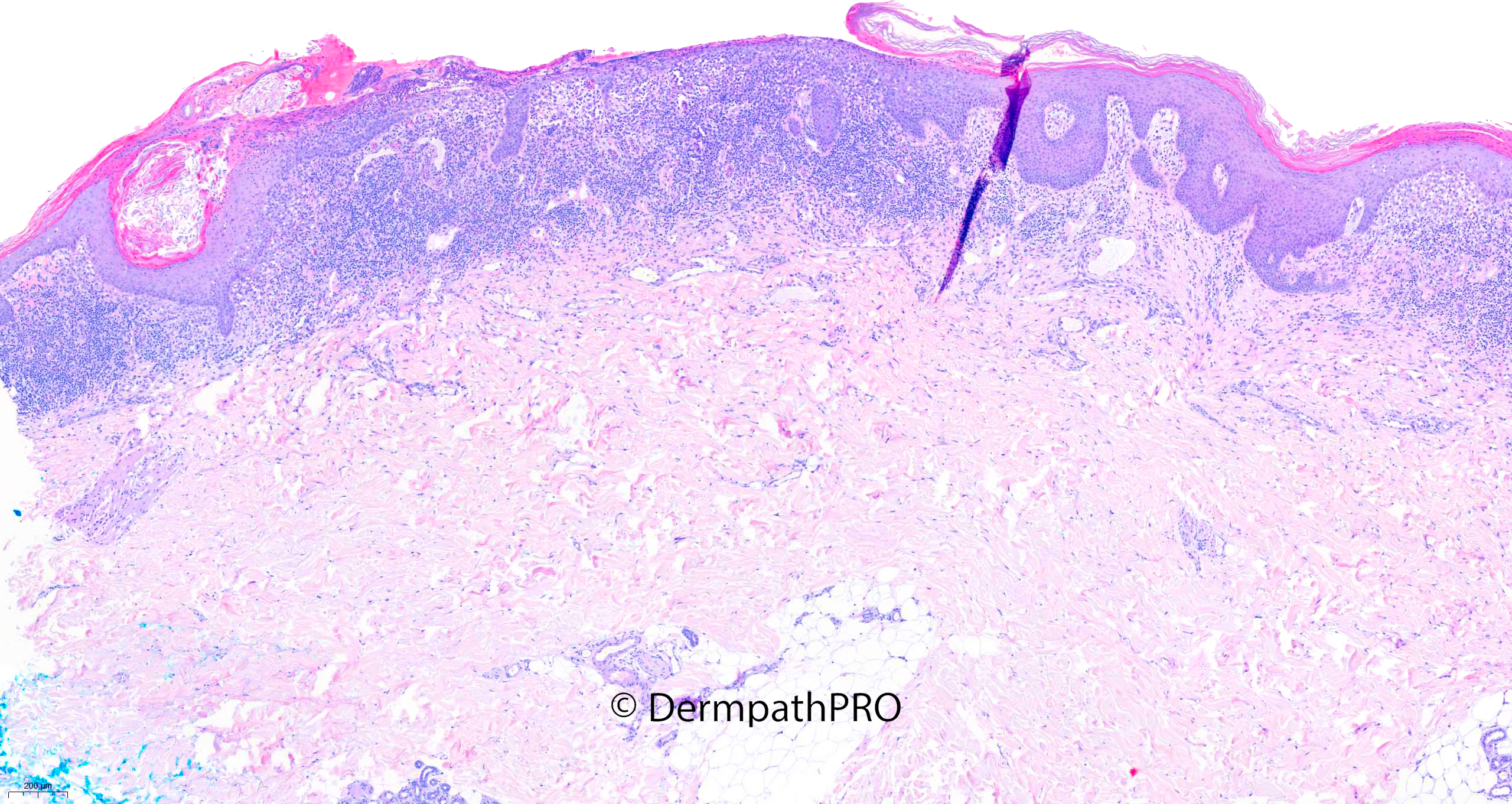
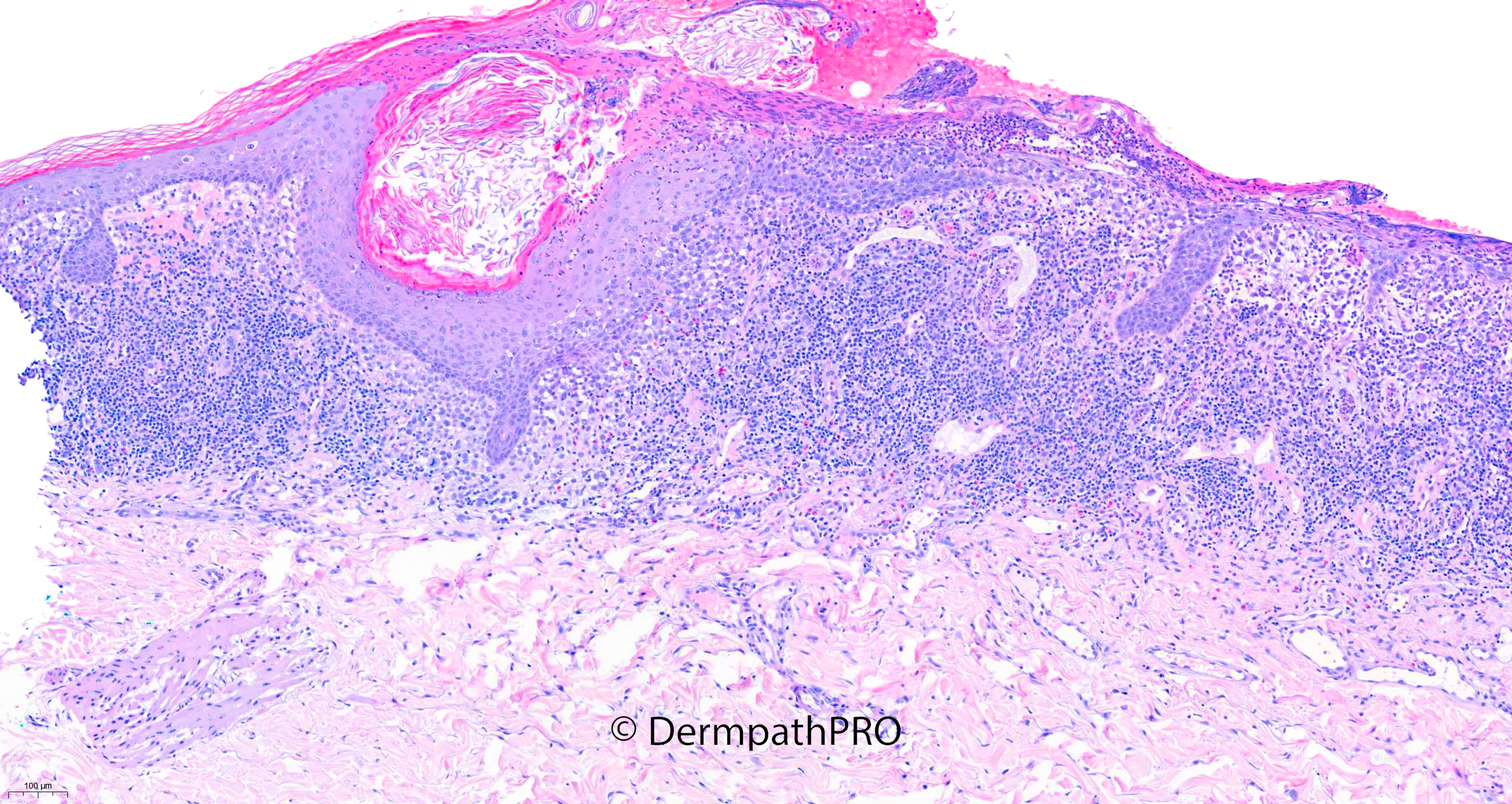
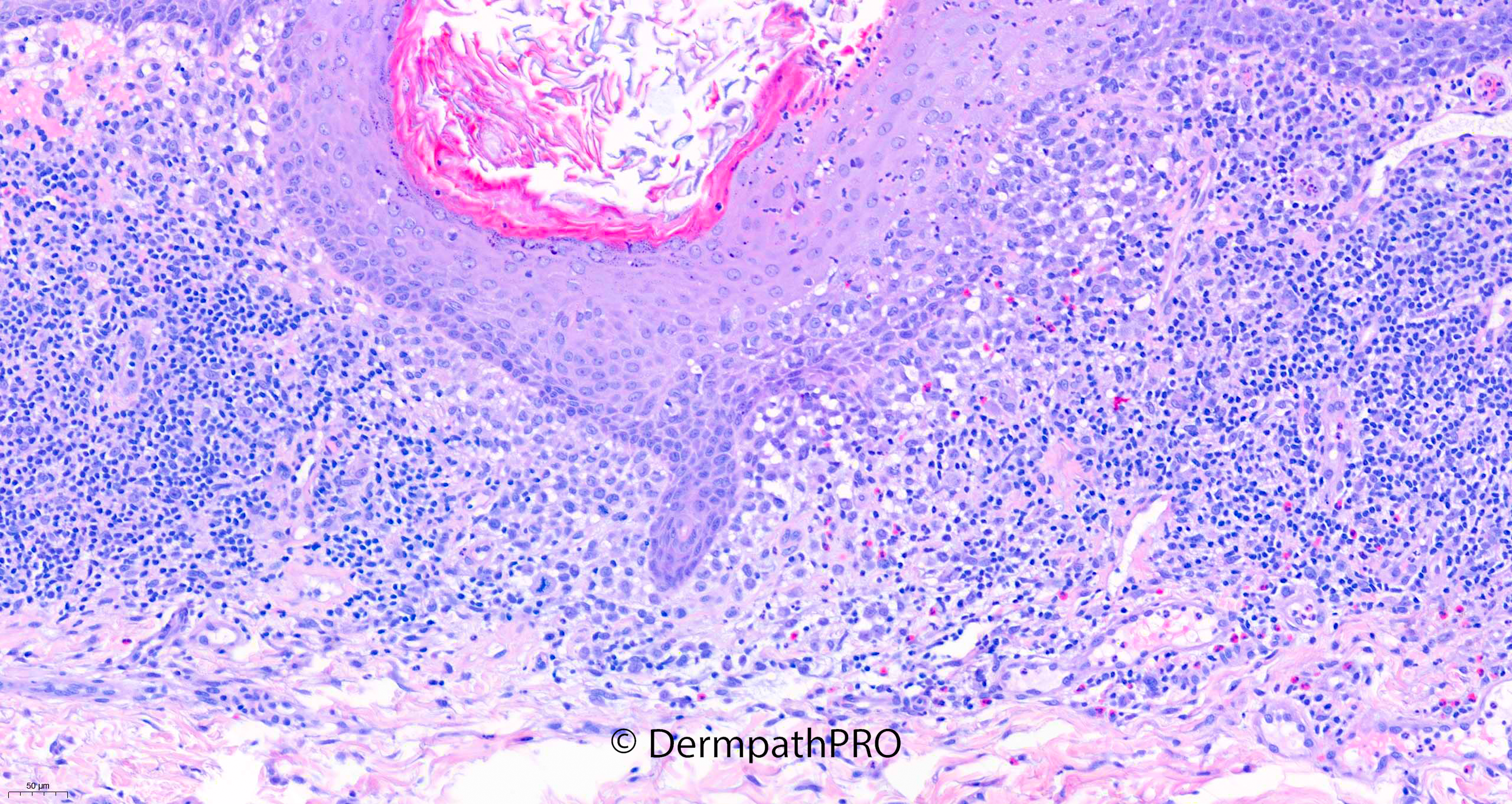
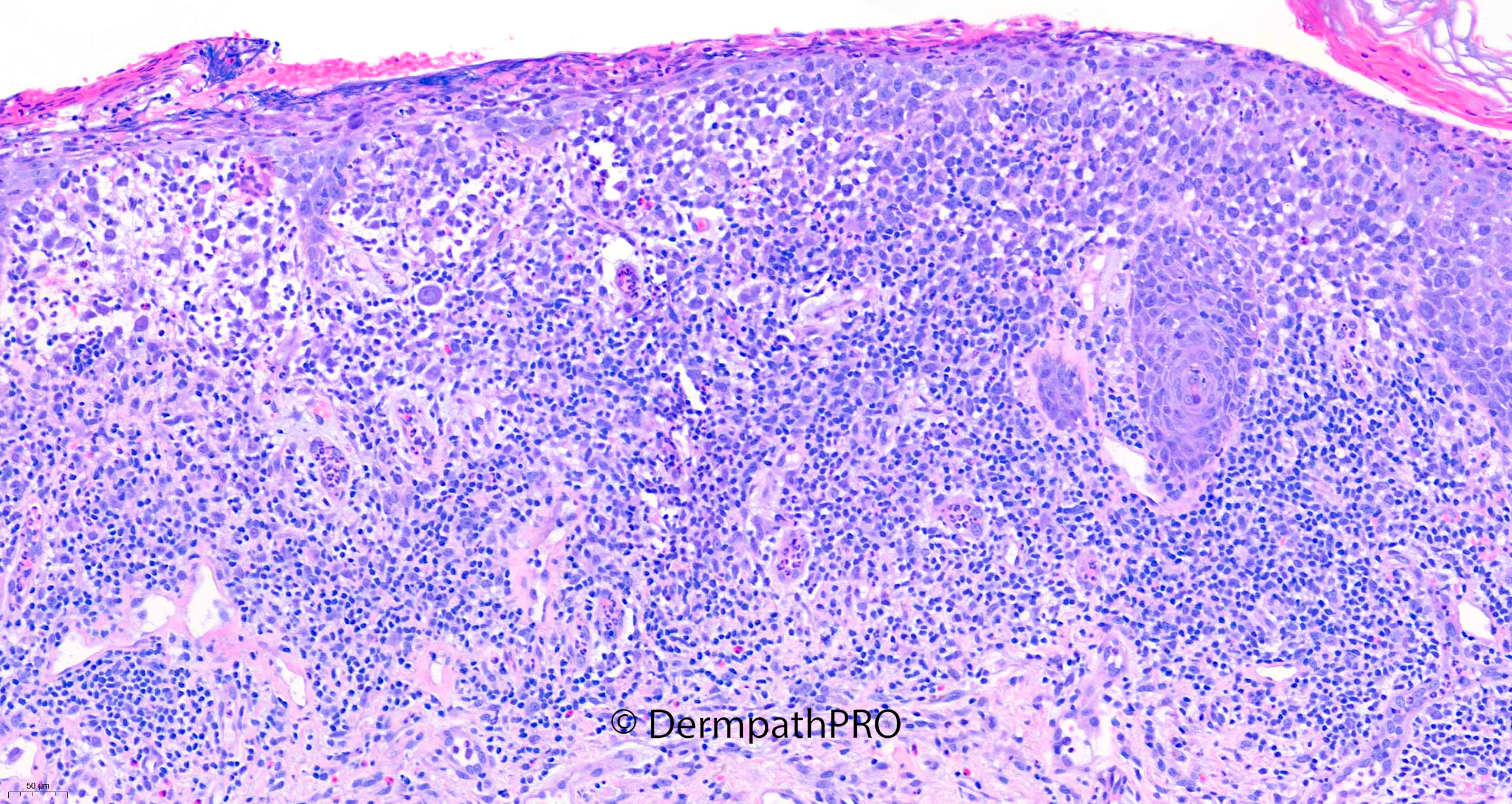
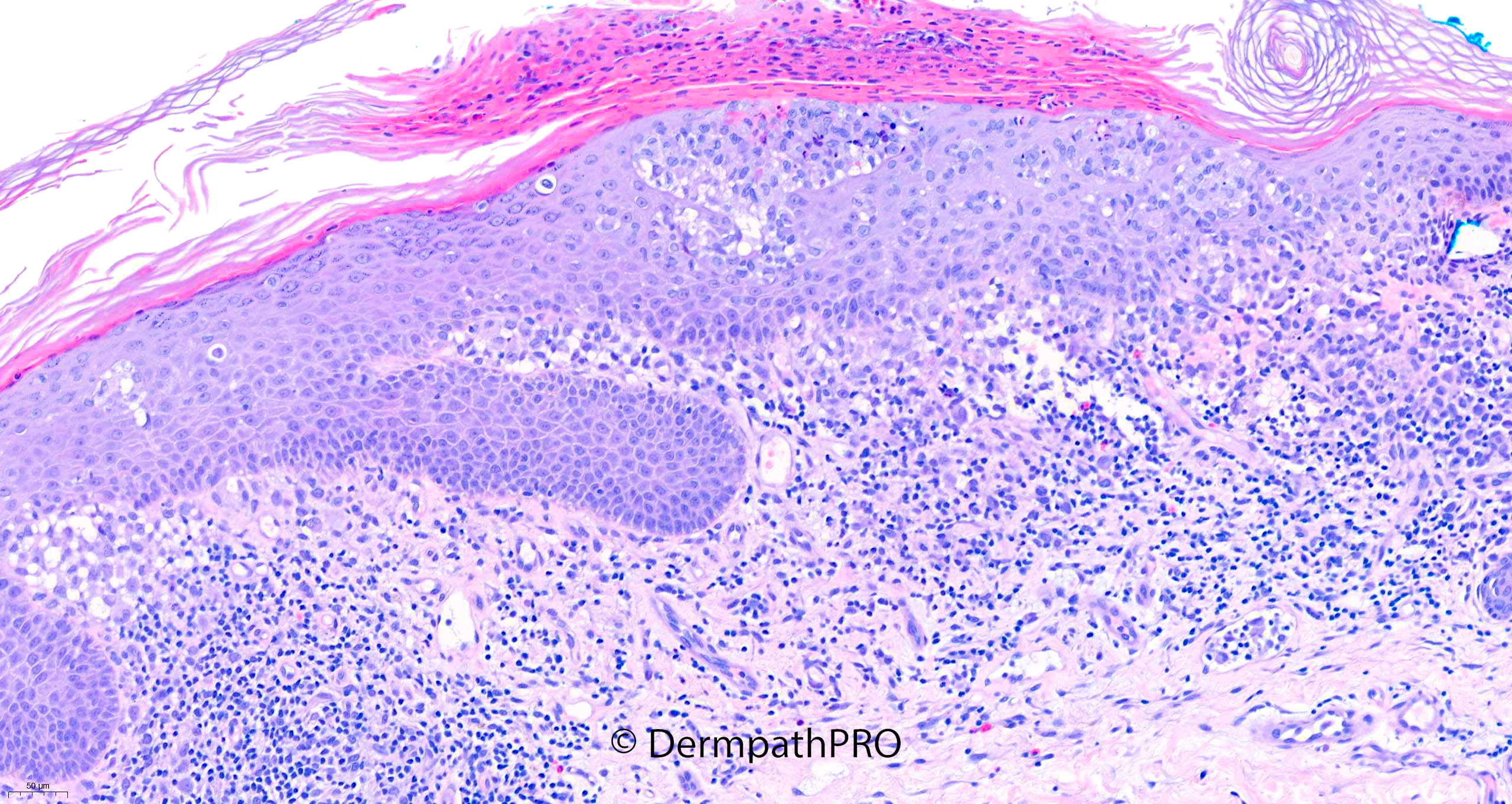
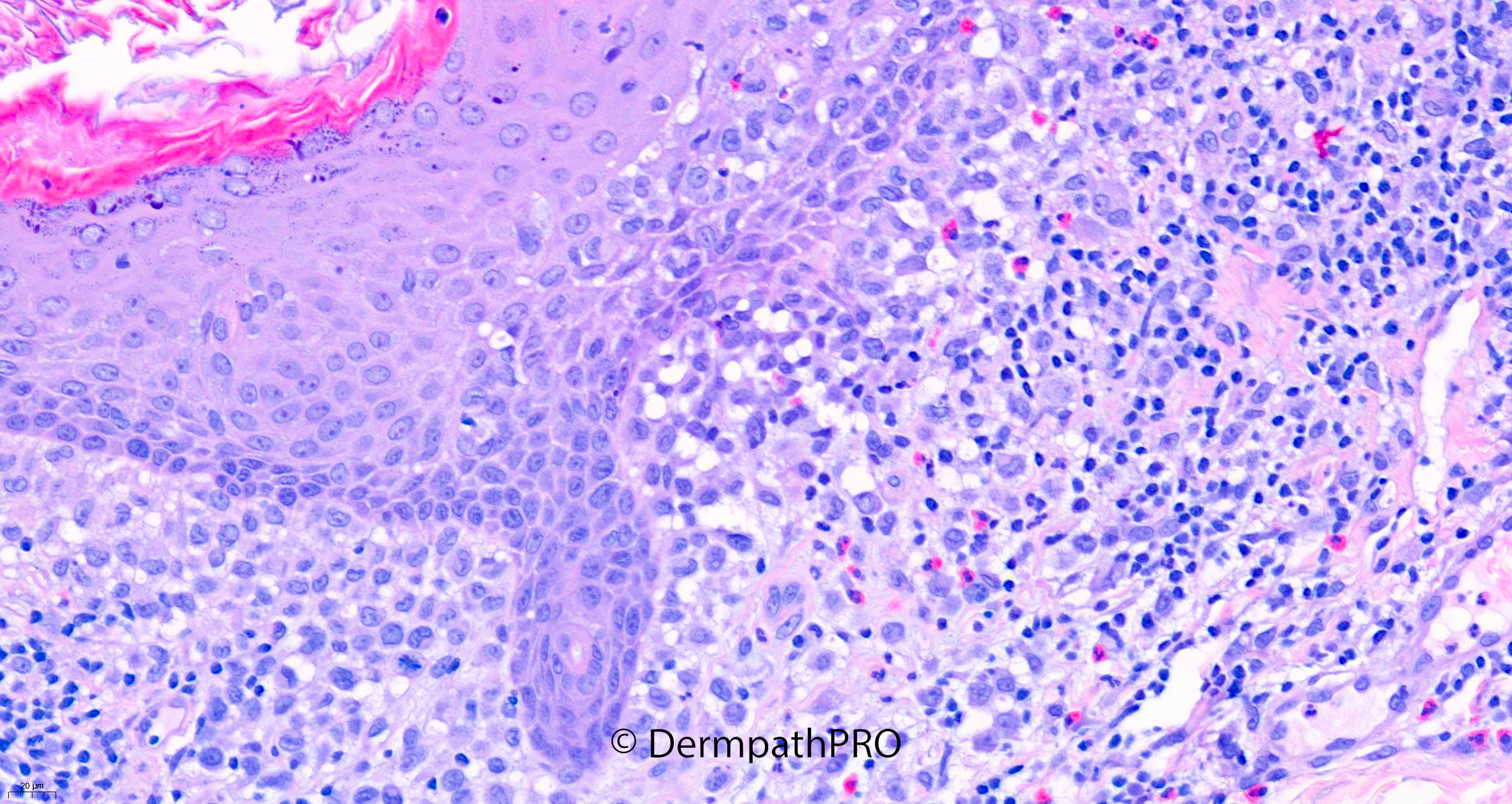
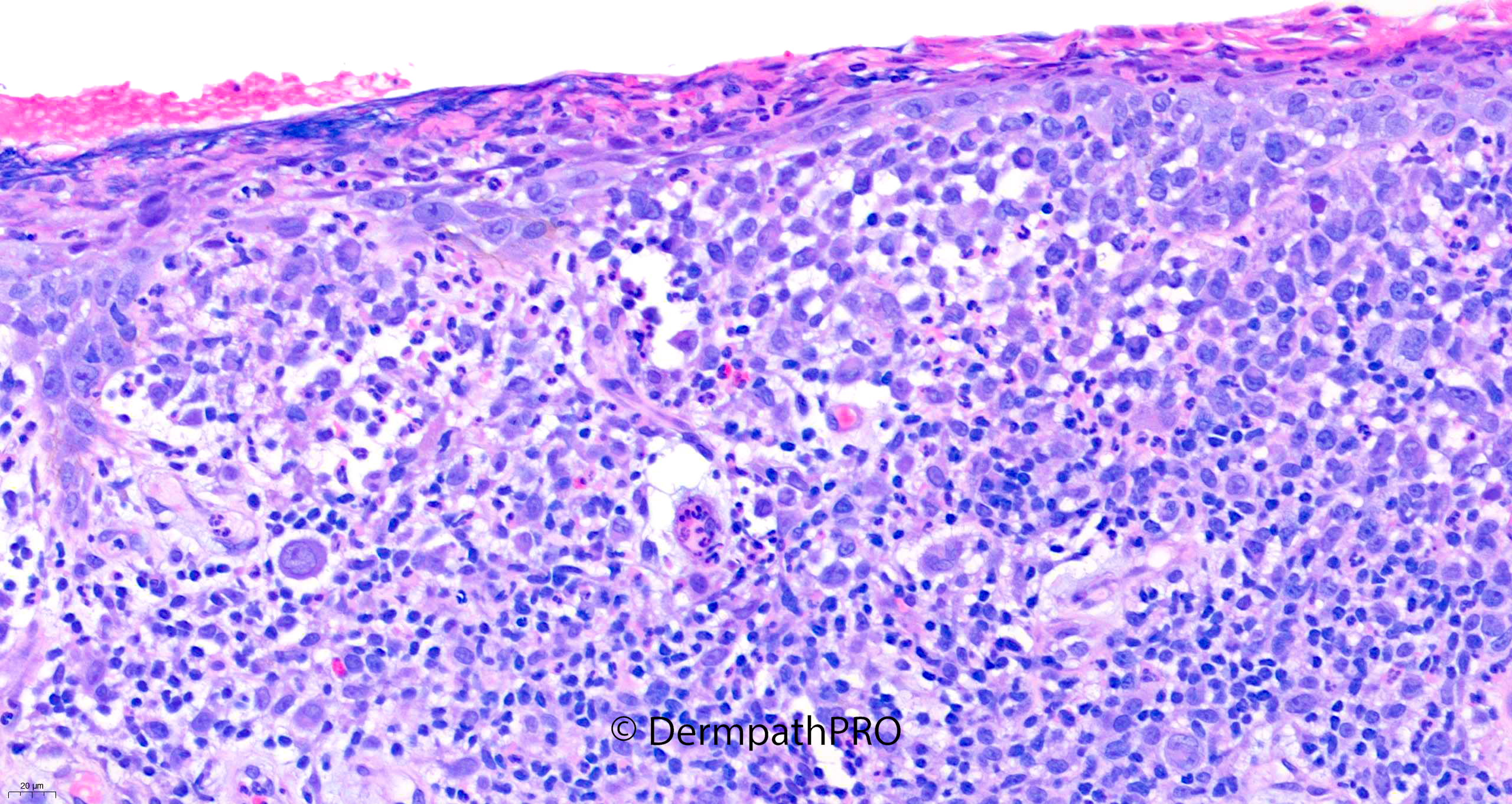
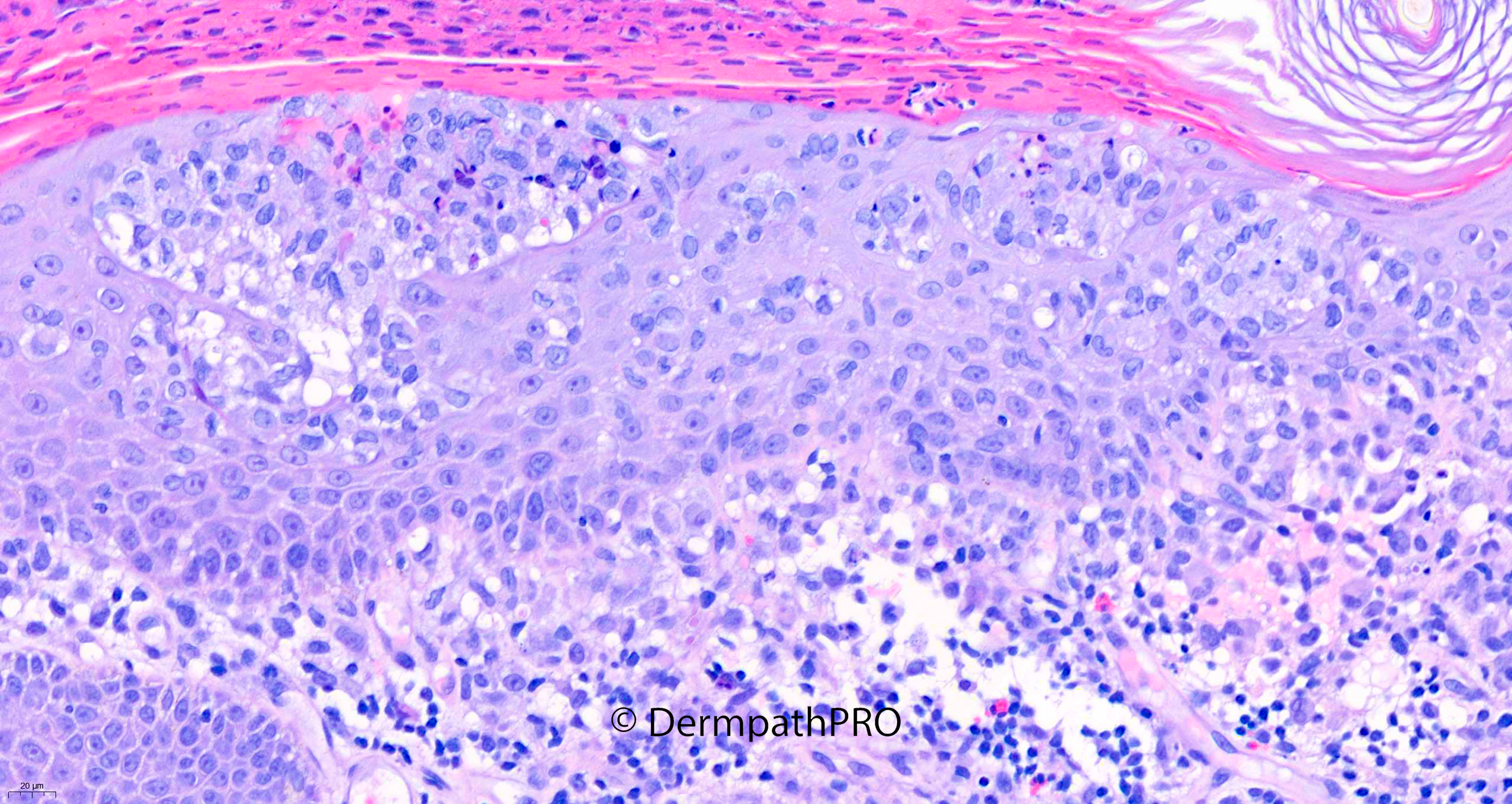
90F Incisional biopsy left submammary skin: suspected lichenoid inflammation, PMH: recent transformation of chronic myelomonocytic leukaemia



Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.