-
 1
1
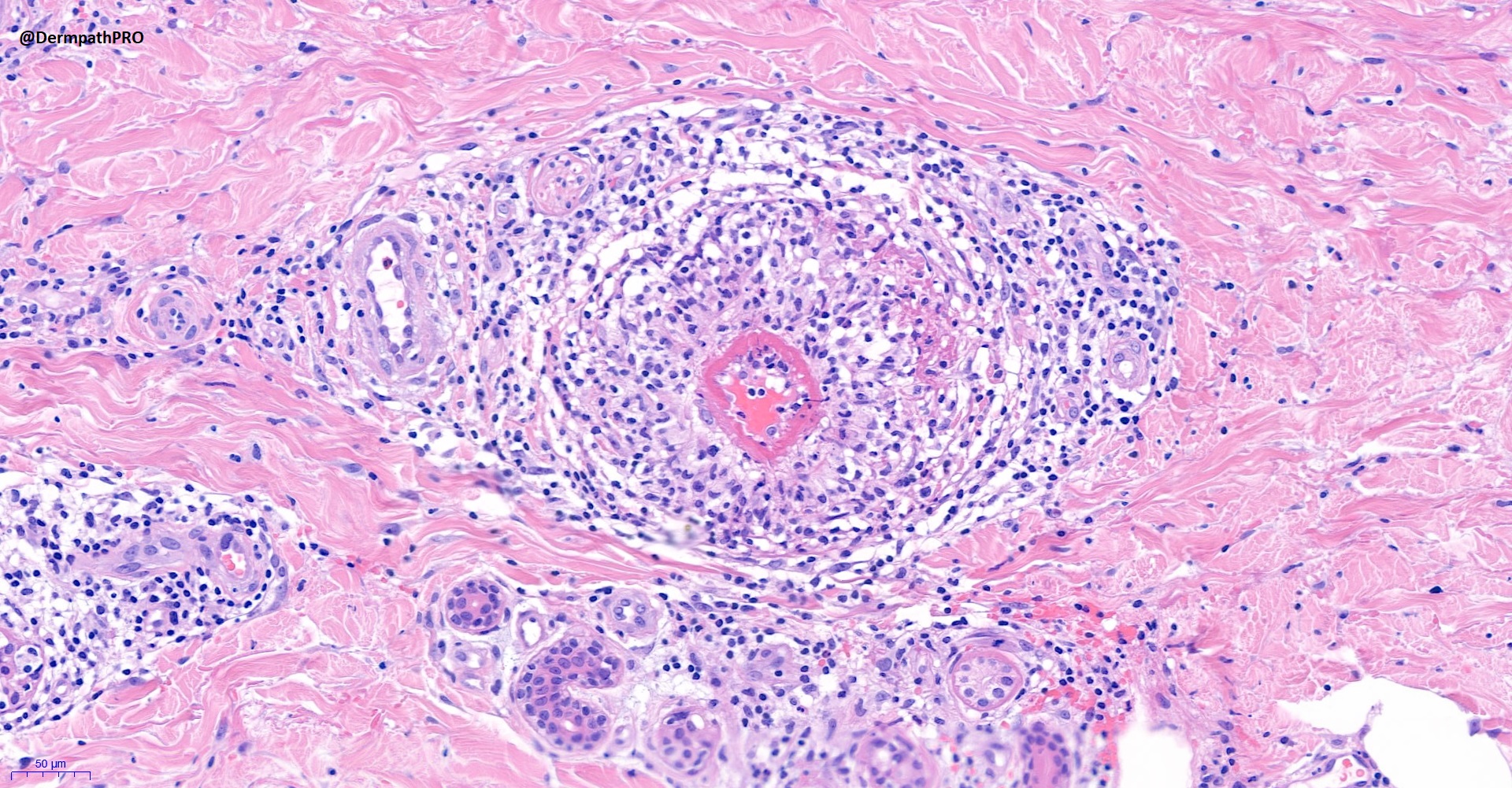
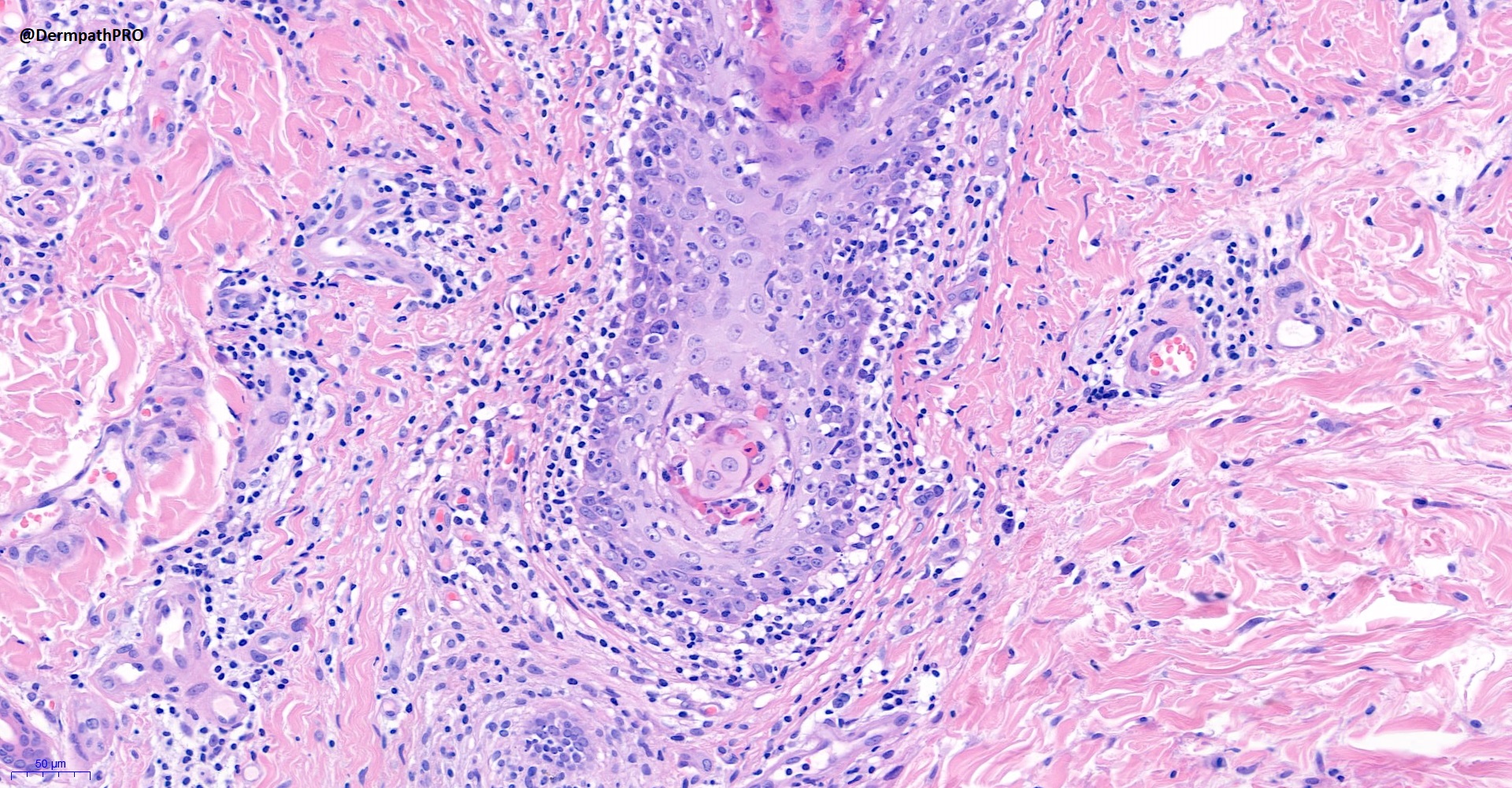
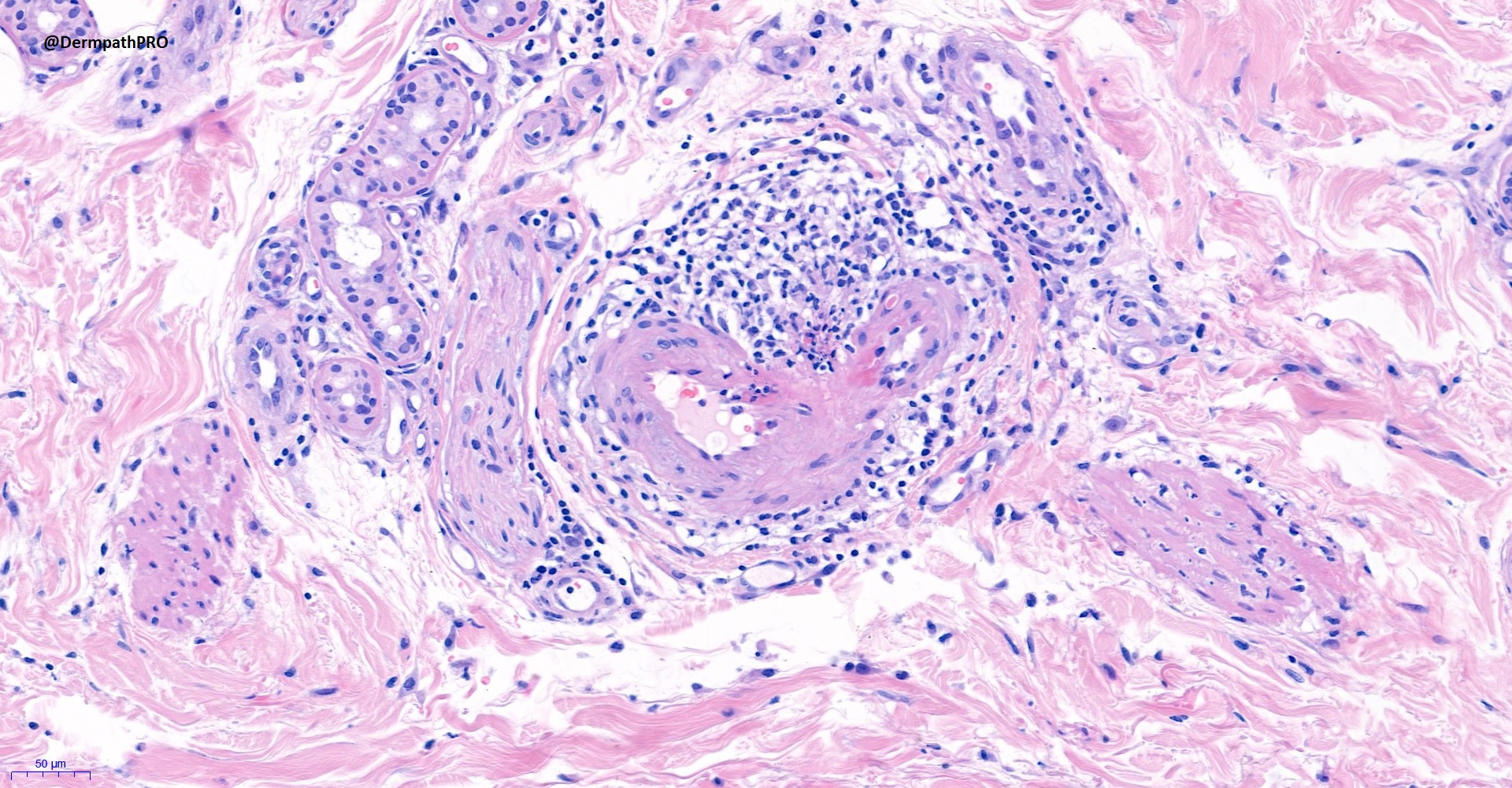
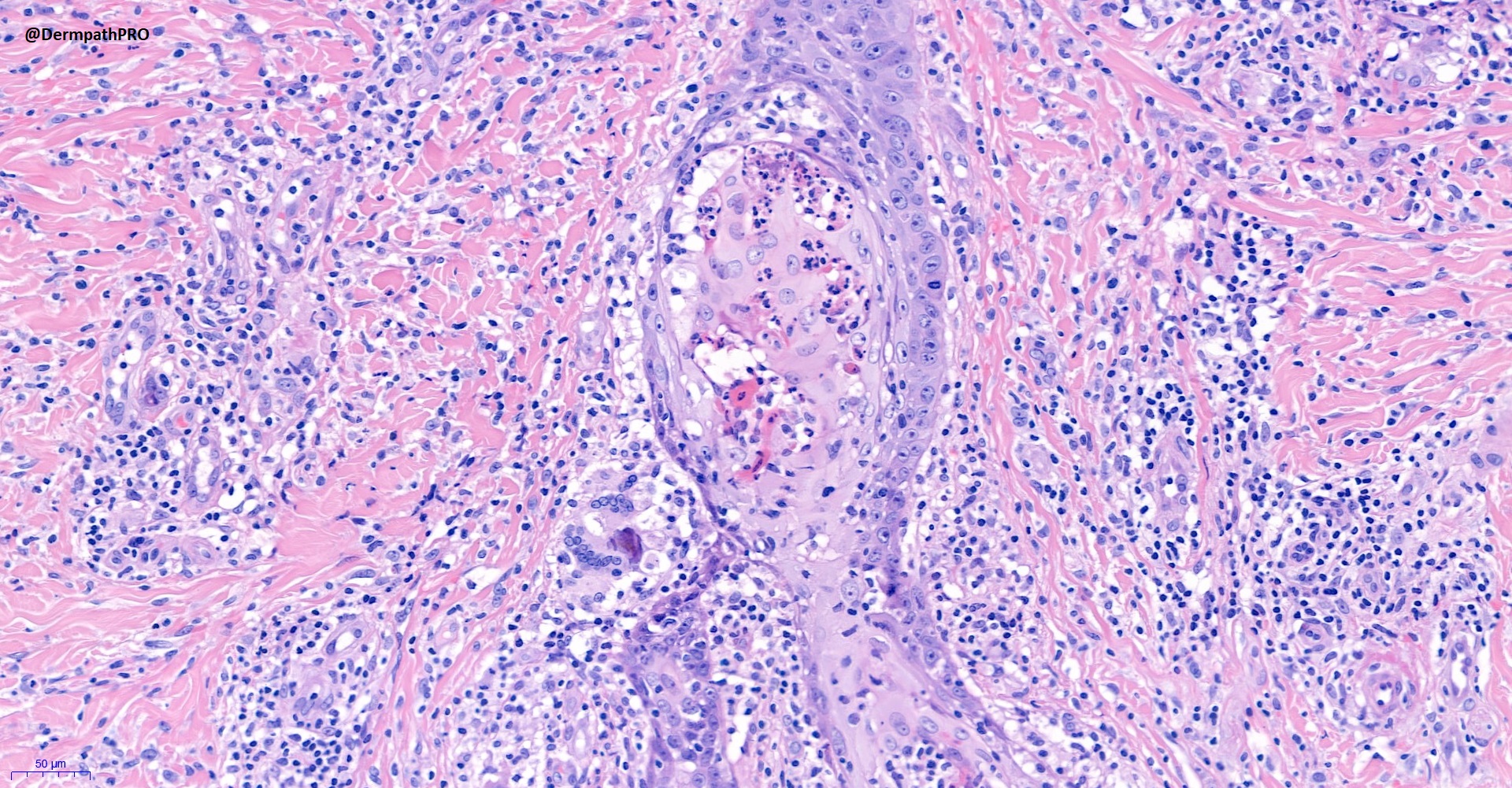
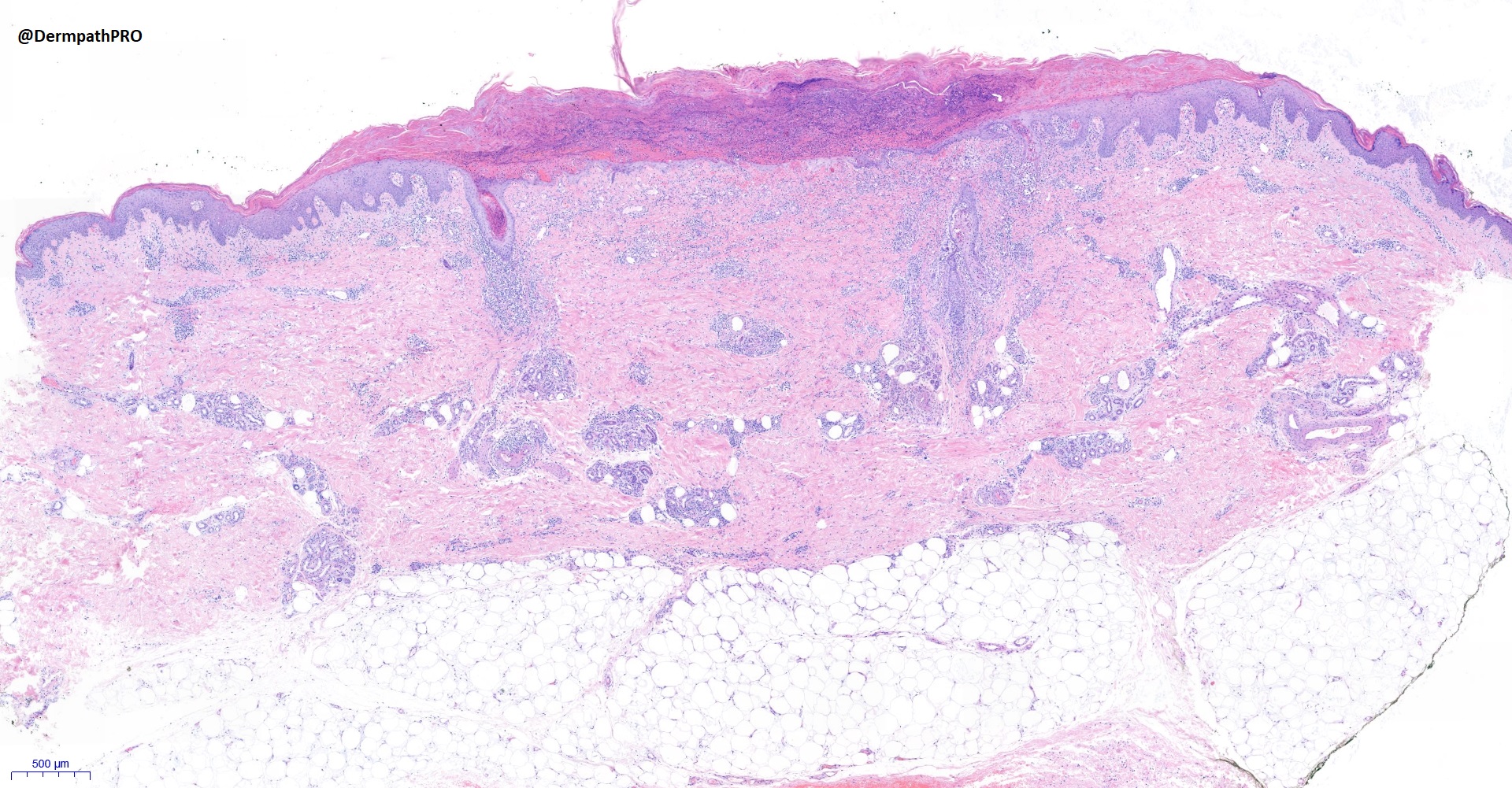
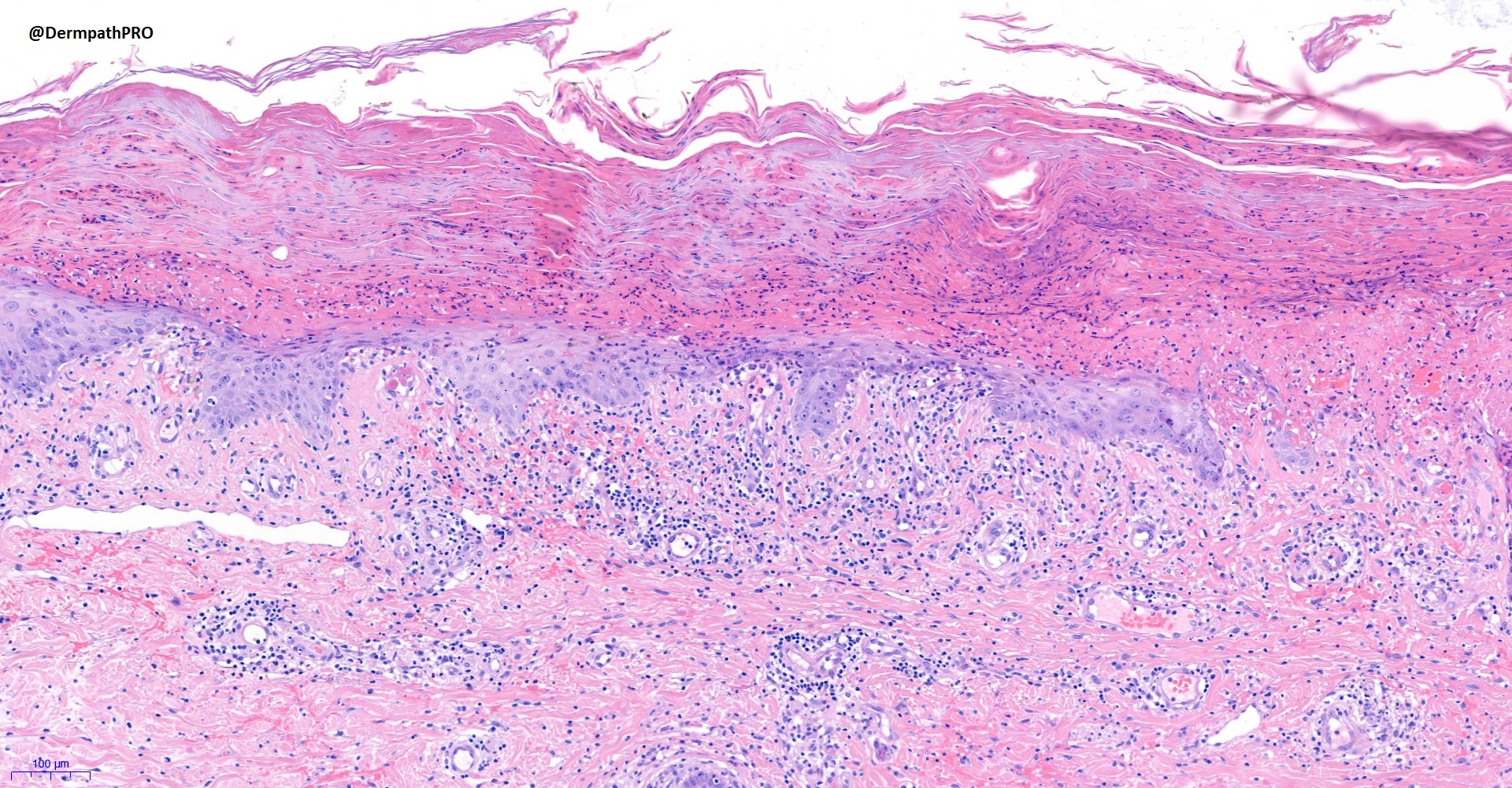
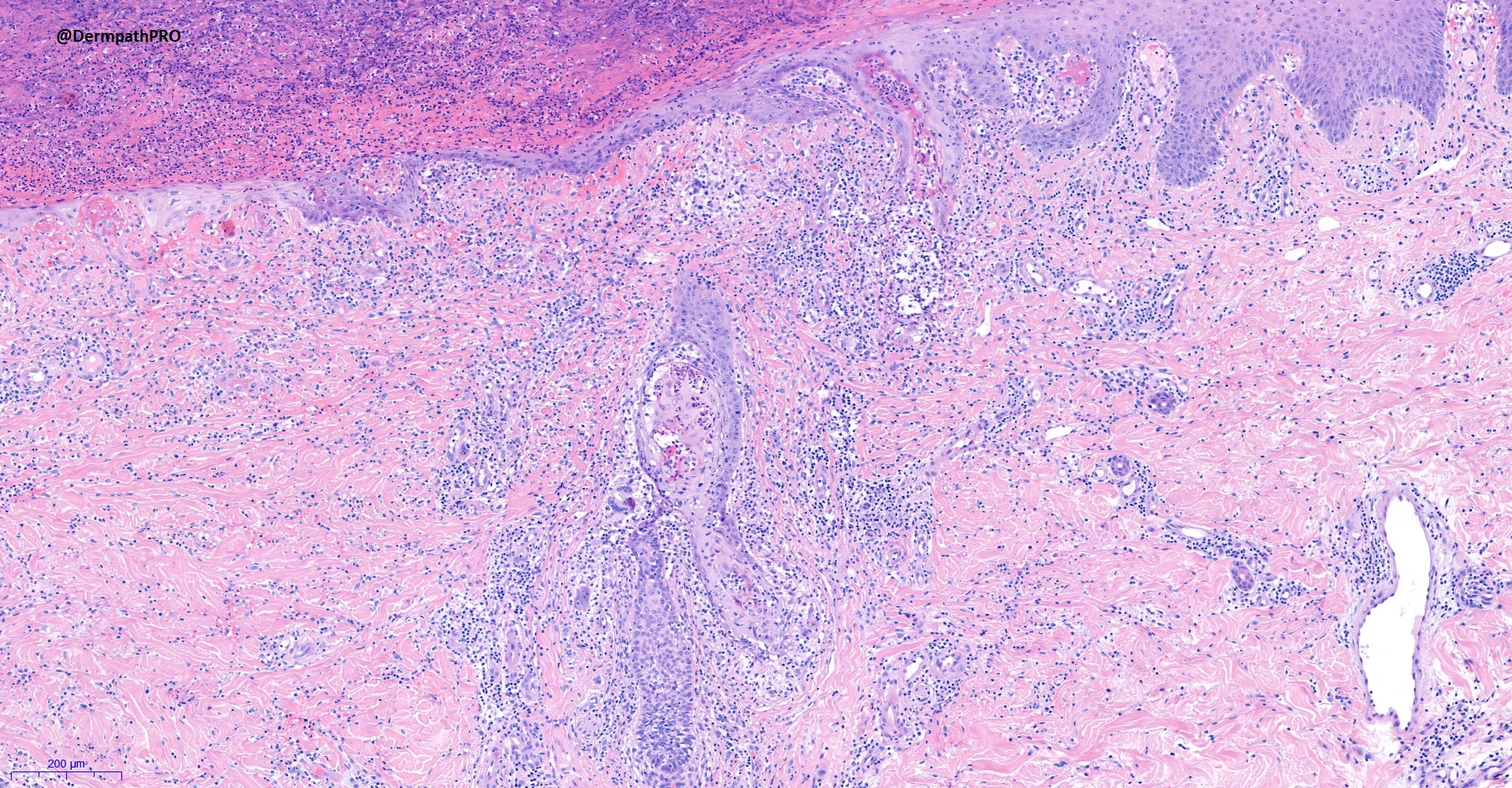
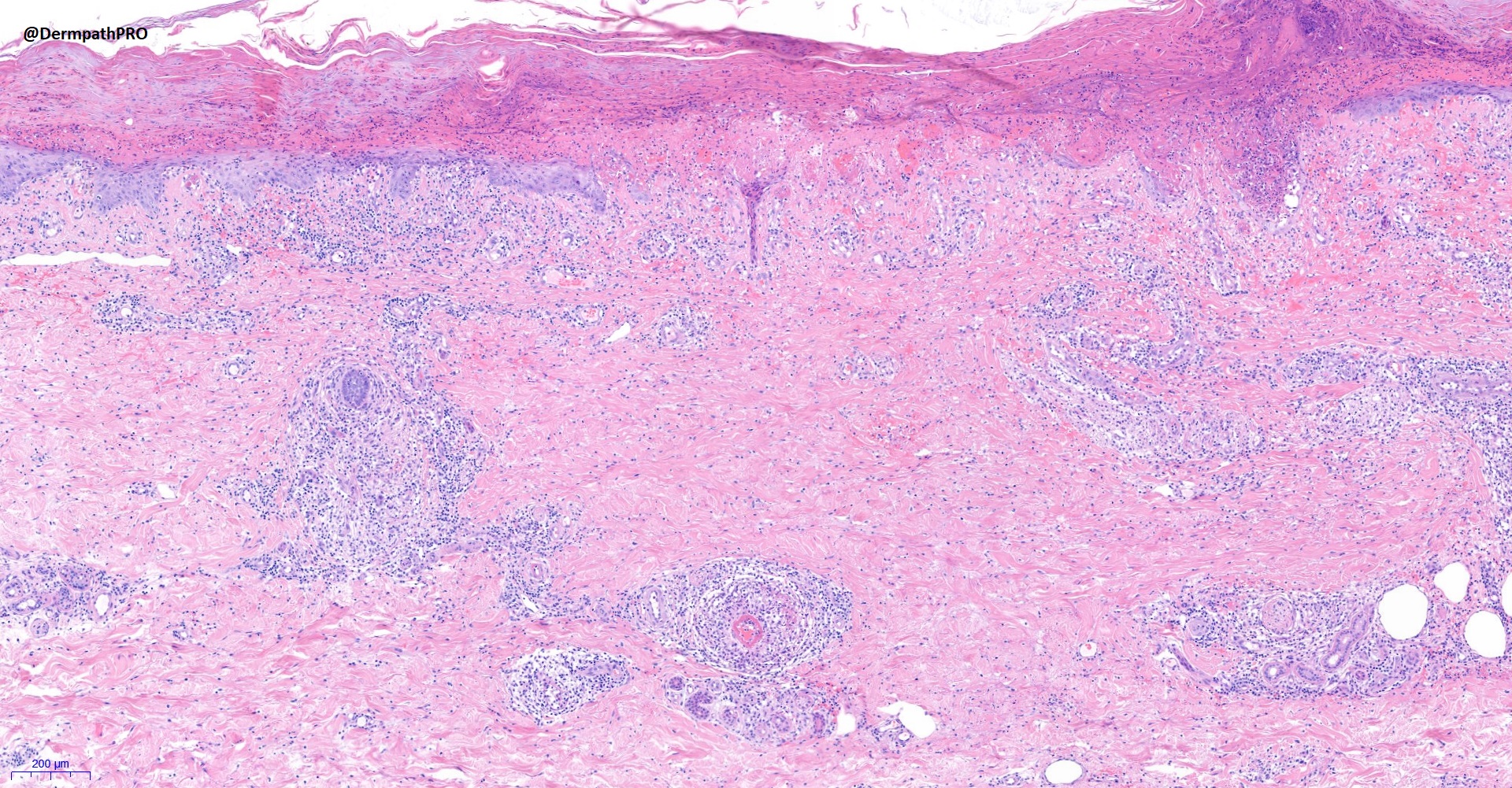
Case Number : Case 2755 - 27 January 2021 Posted By: Saleem Taibjee
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
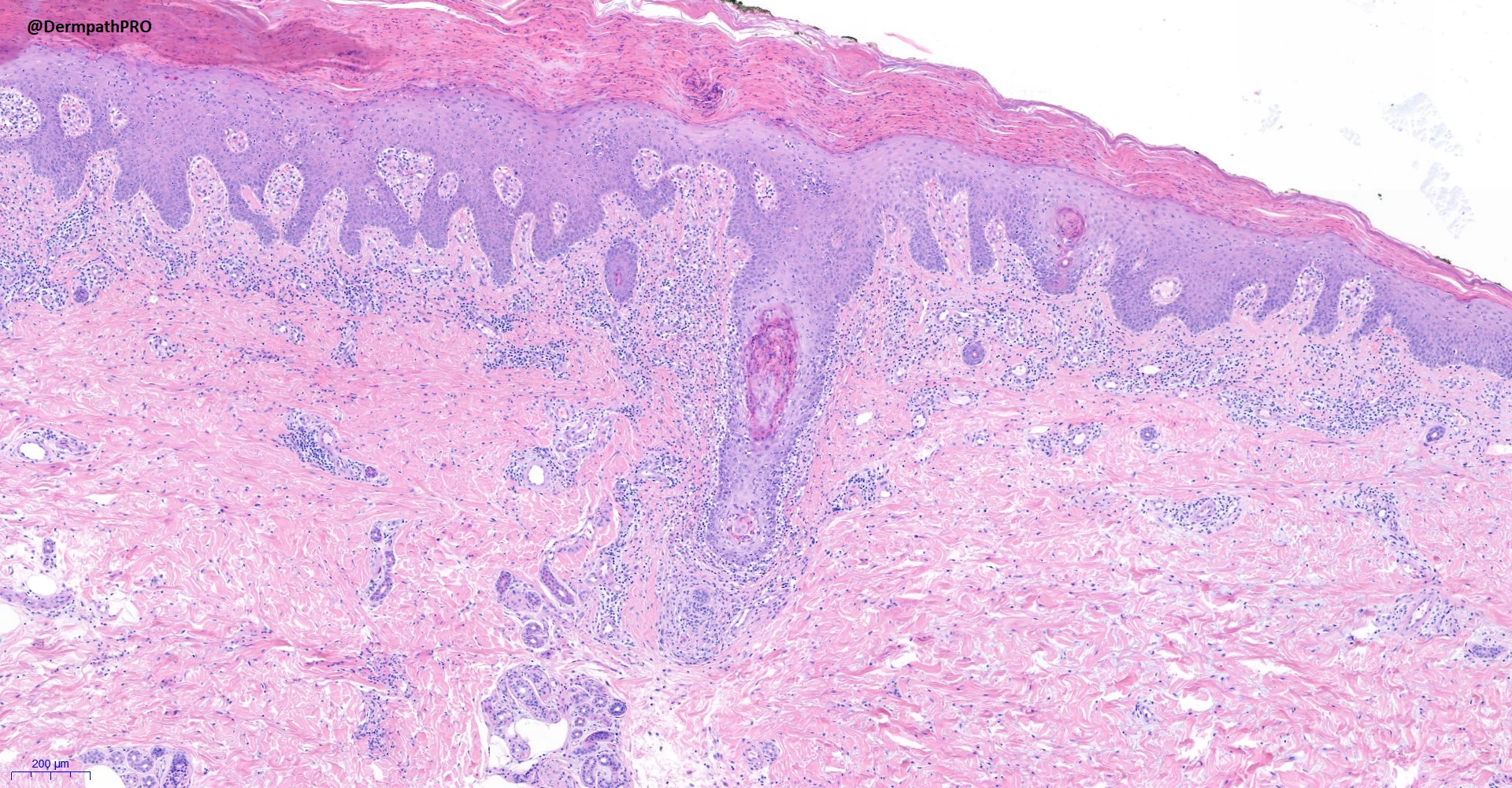
48F, widespread erythematous papules.

Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.