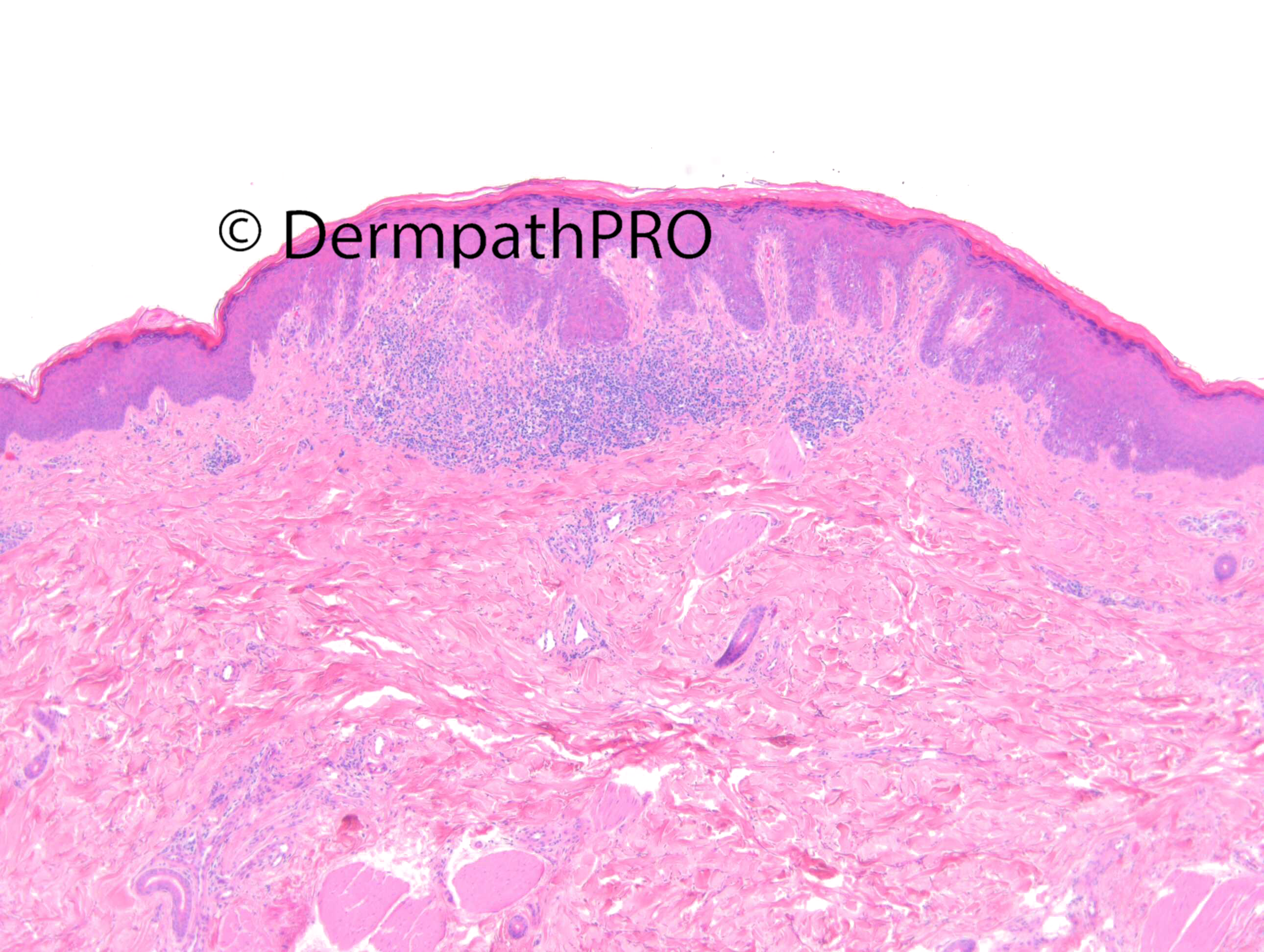
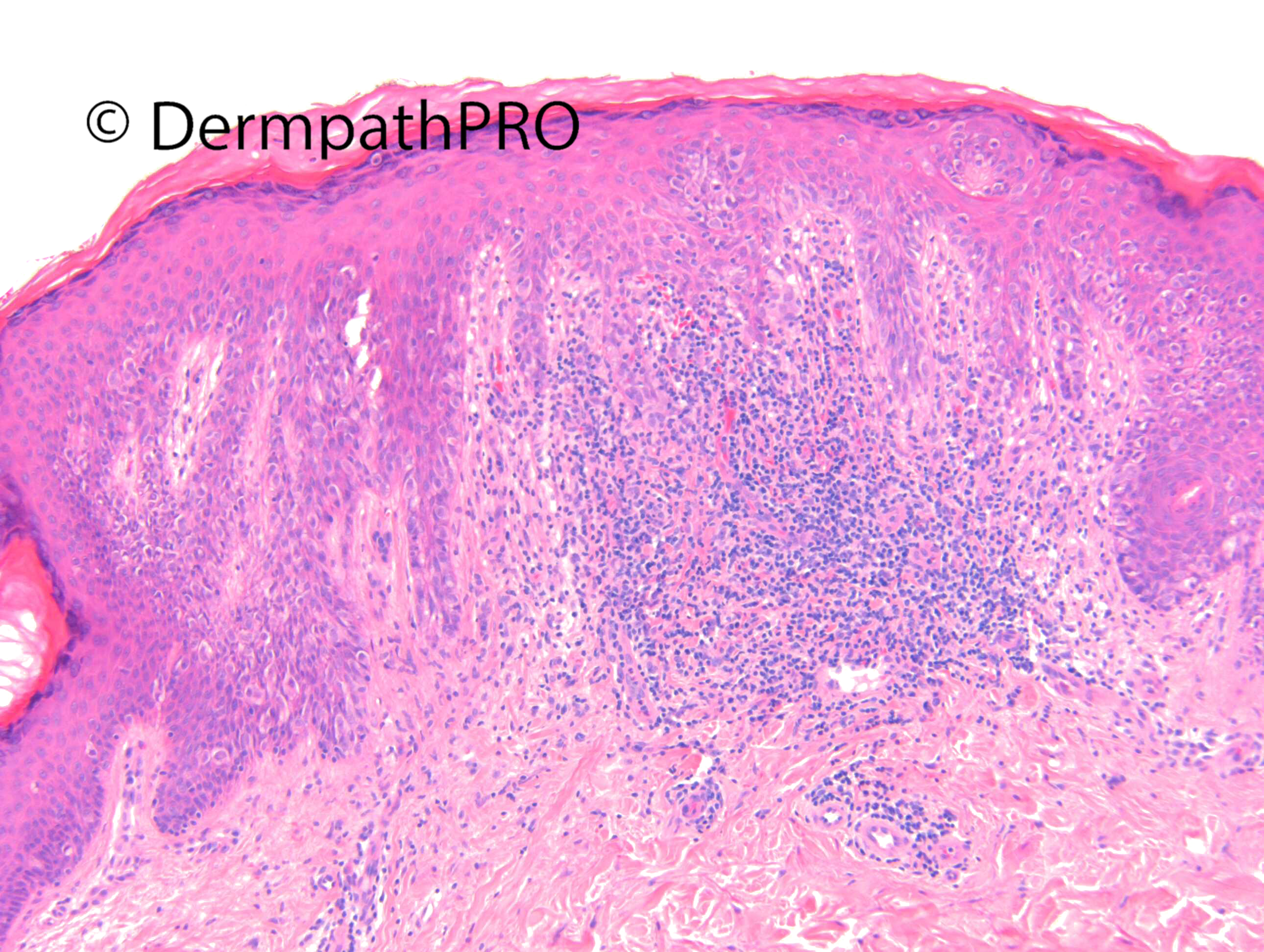
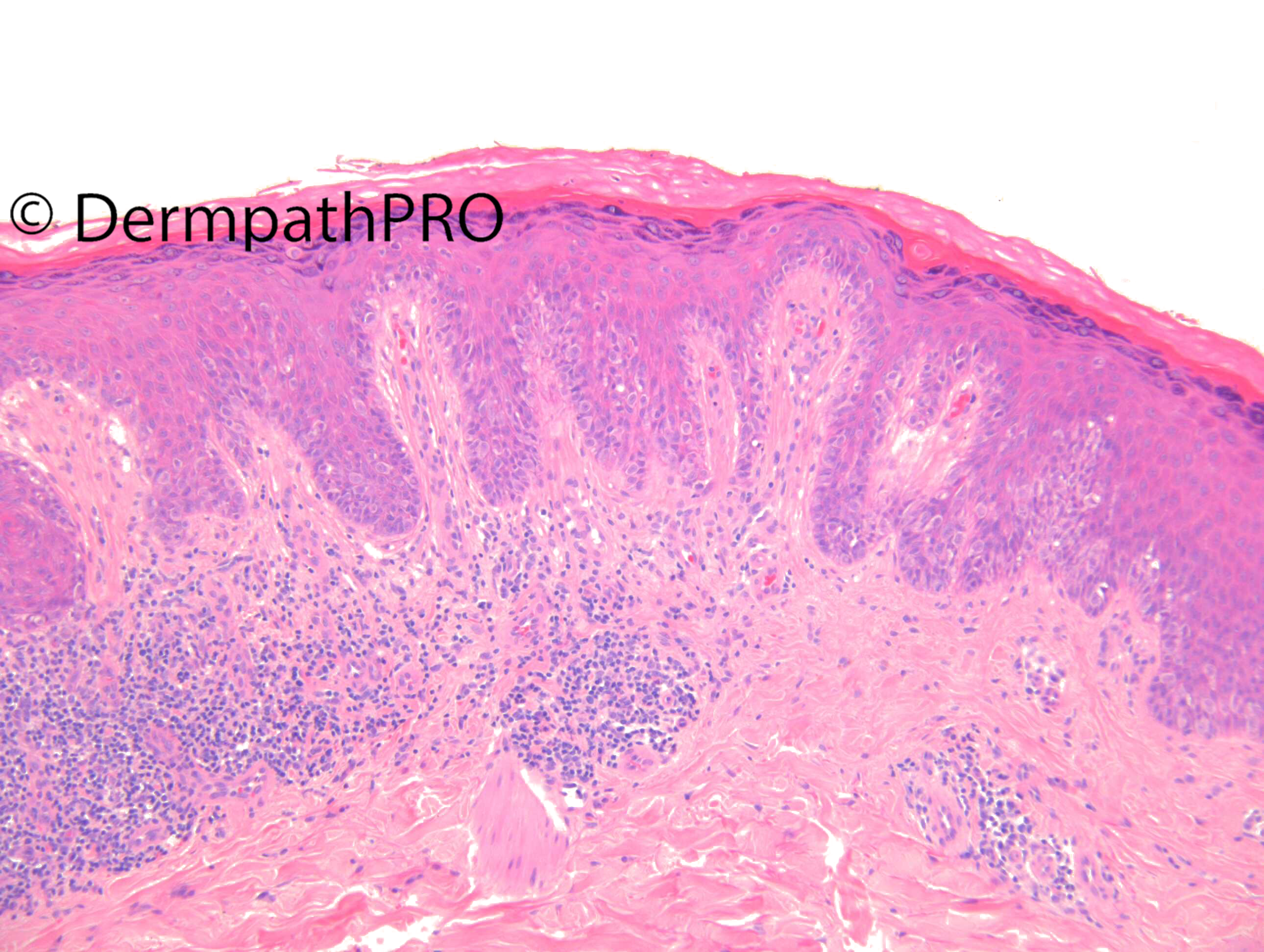
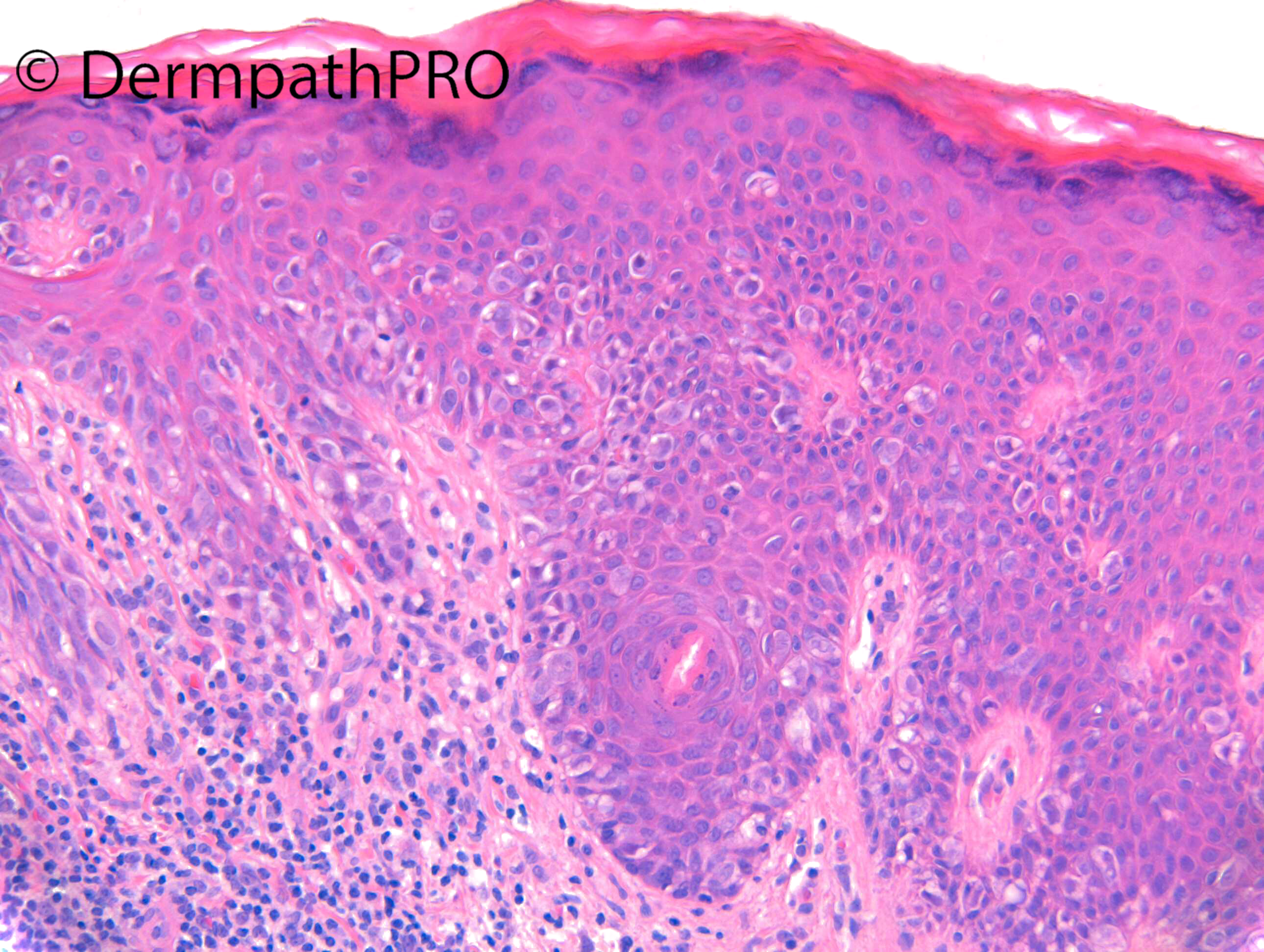
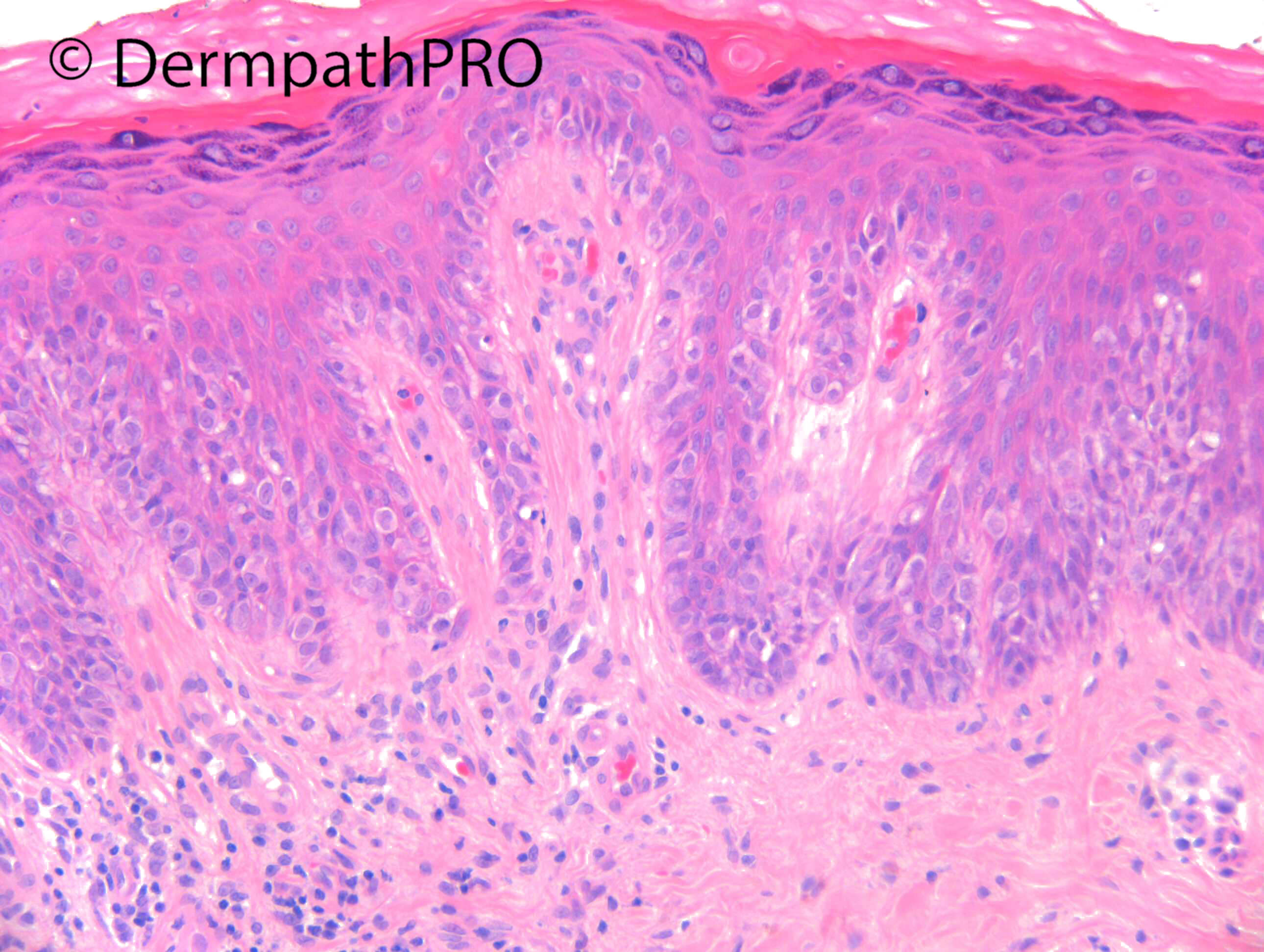
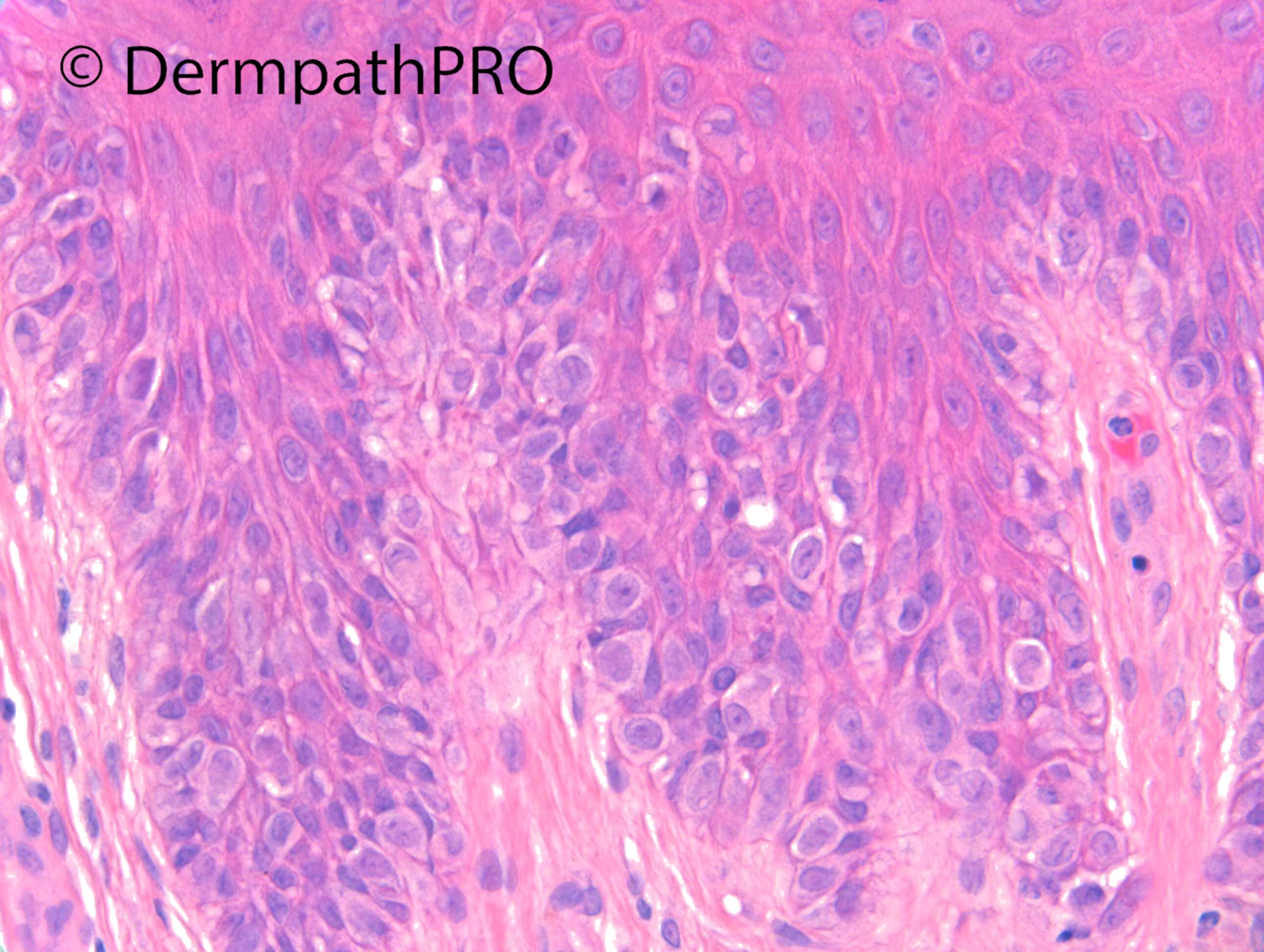
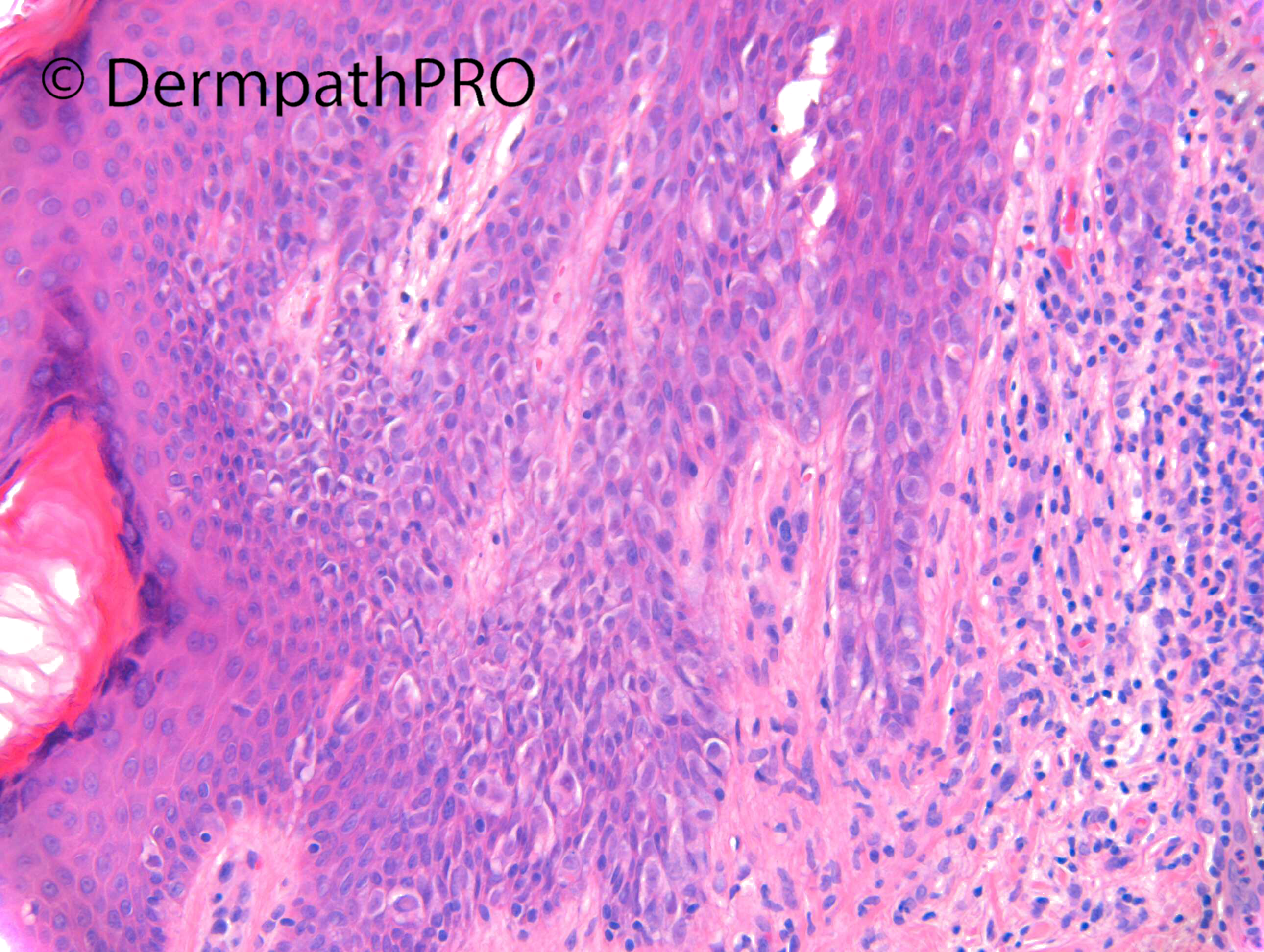
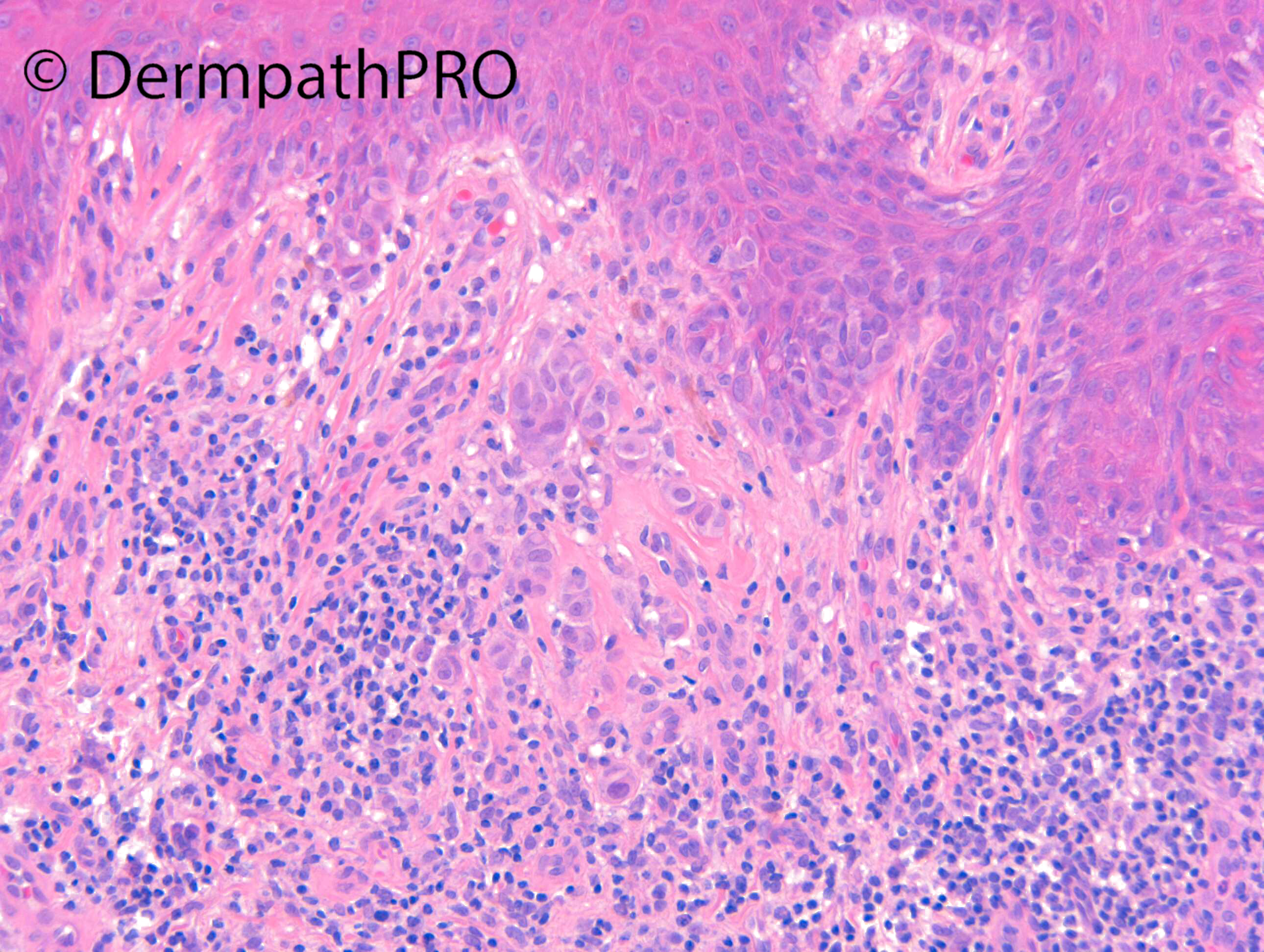
Case Number : Case 2937 - 08 October 2021 Posted By: Dr. Richard Carr
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
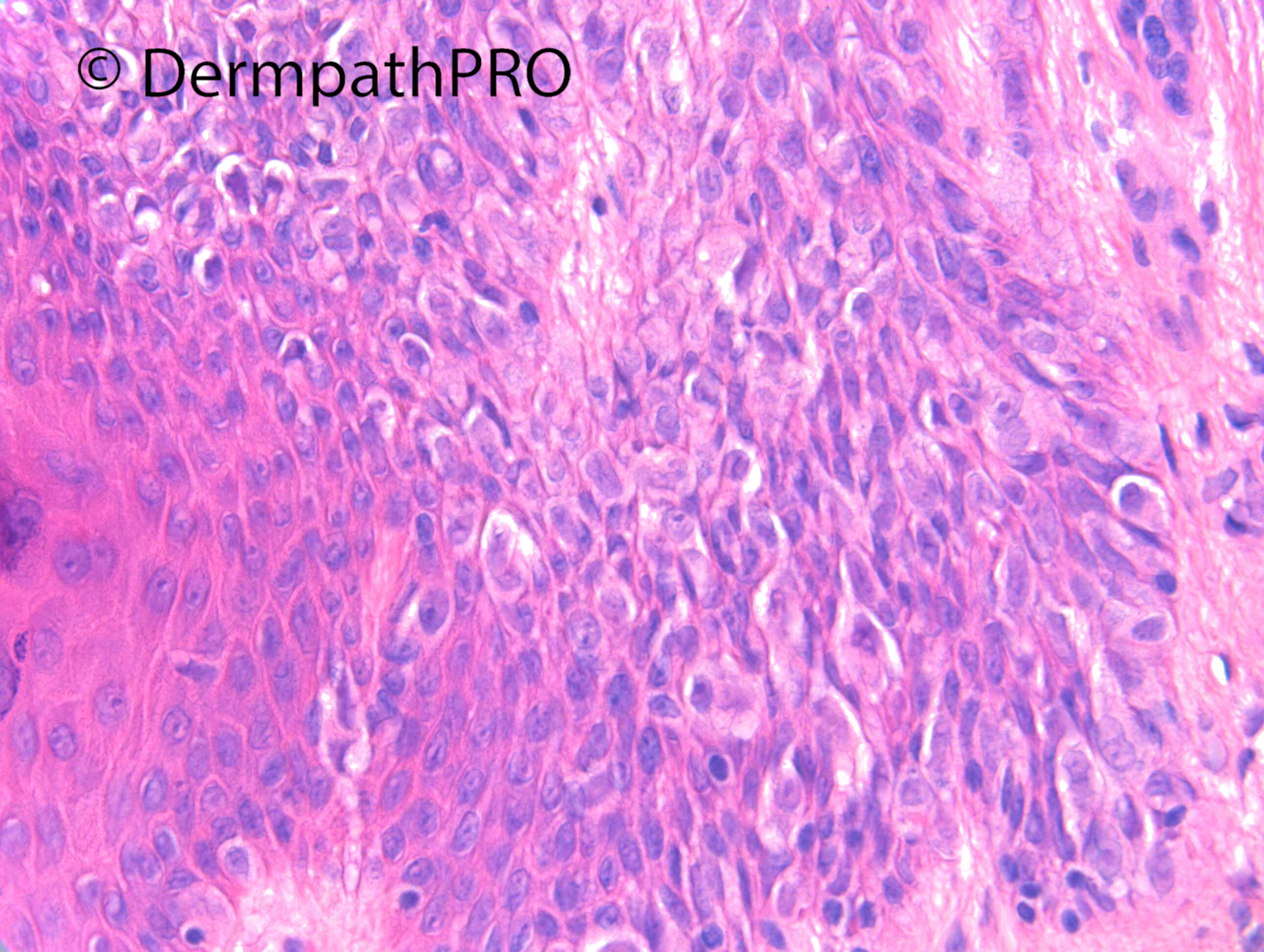
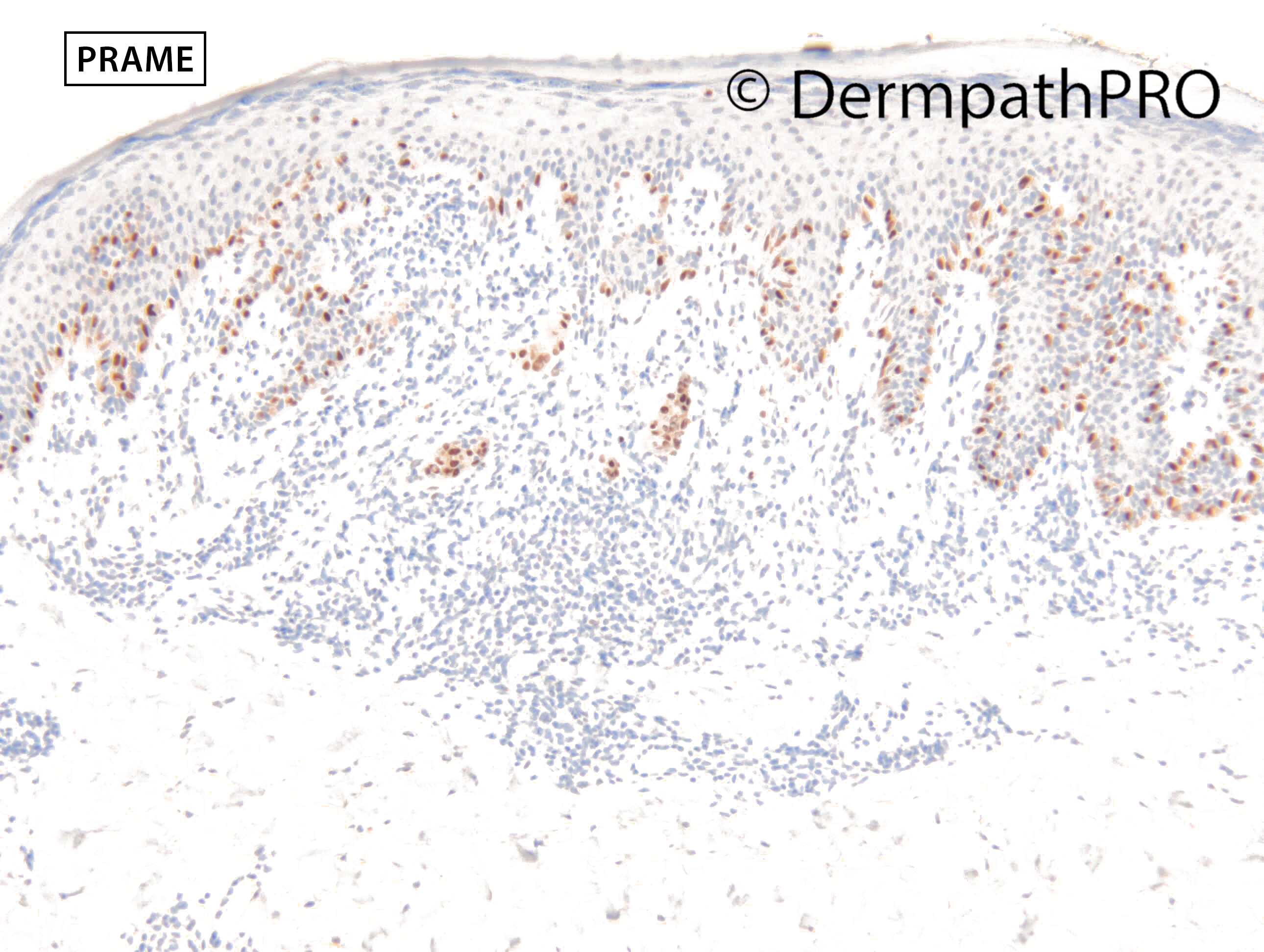
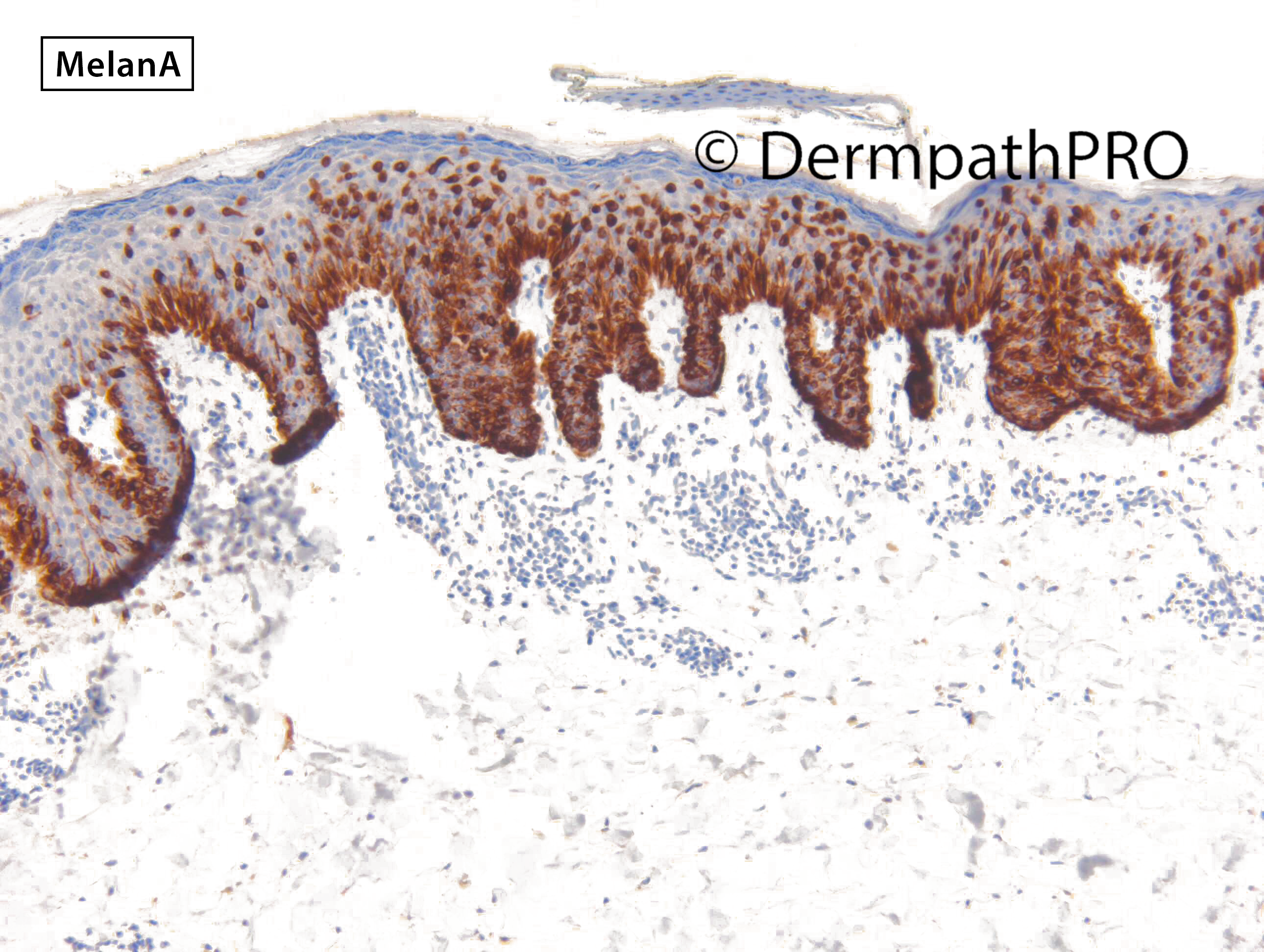
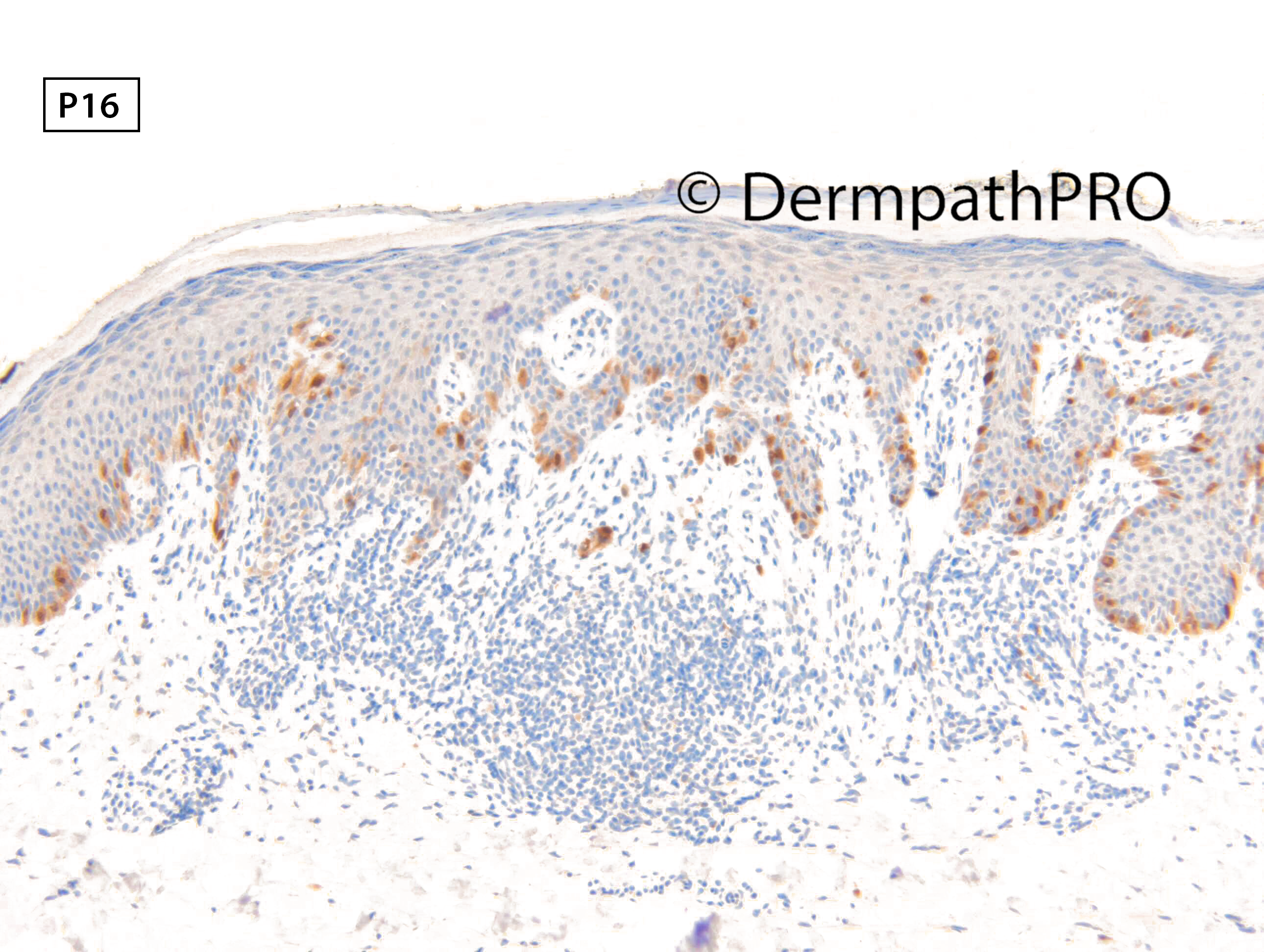
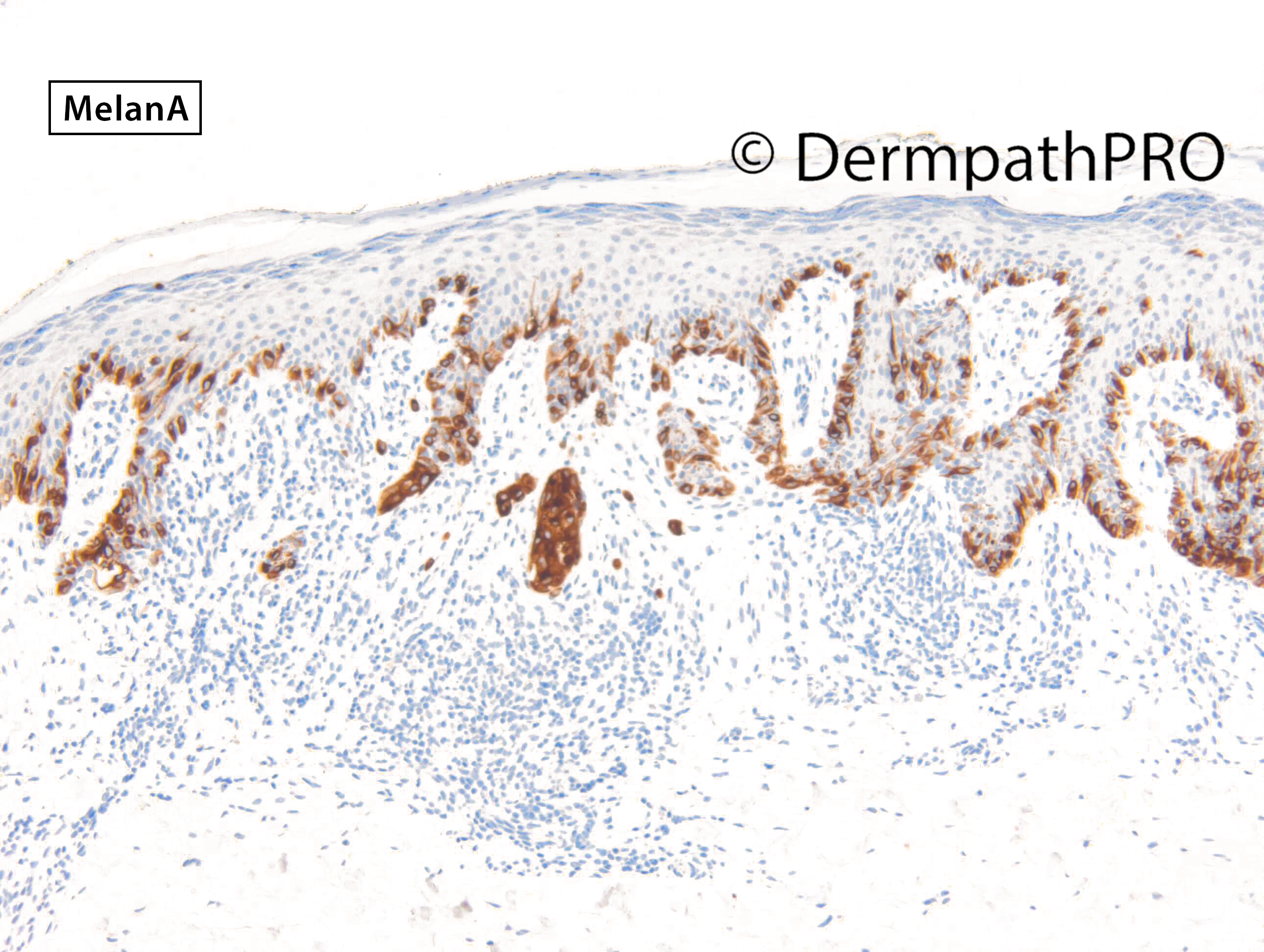
M34. Left thigh. Pink macule, changes 1/12 ago, become partially pigmented, increasing size. ?DN, ?MM, ?pigmented BCC

Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.