-
 1
1
Case Number : Case 3016 - 27 January 2022 Posted By: Saleem Taibjee
Please read the clinical history and view the images by clicking on them before you proffer your diagnosis.
Submitted Date :
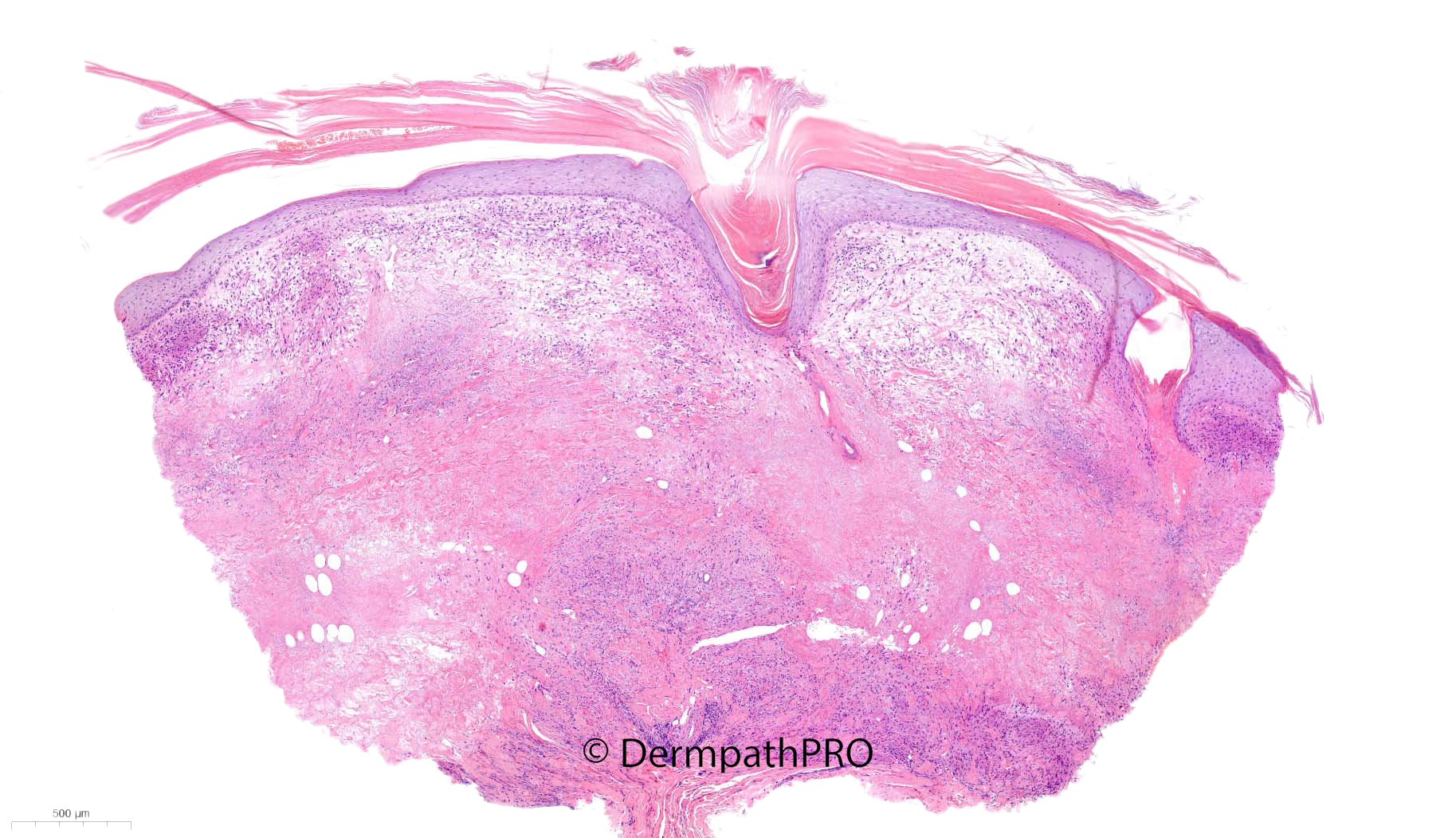
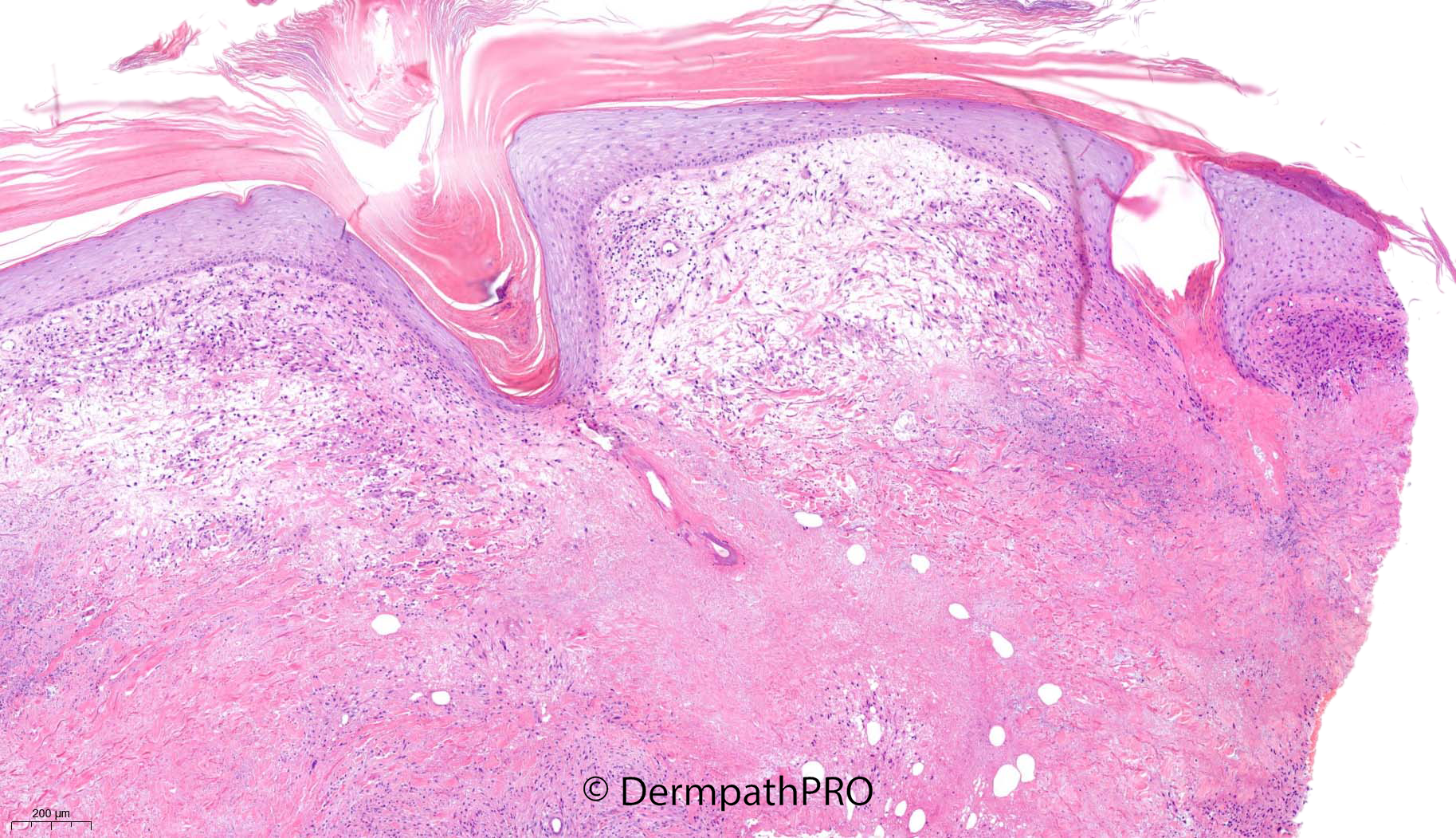
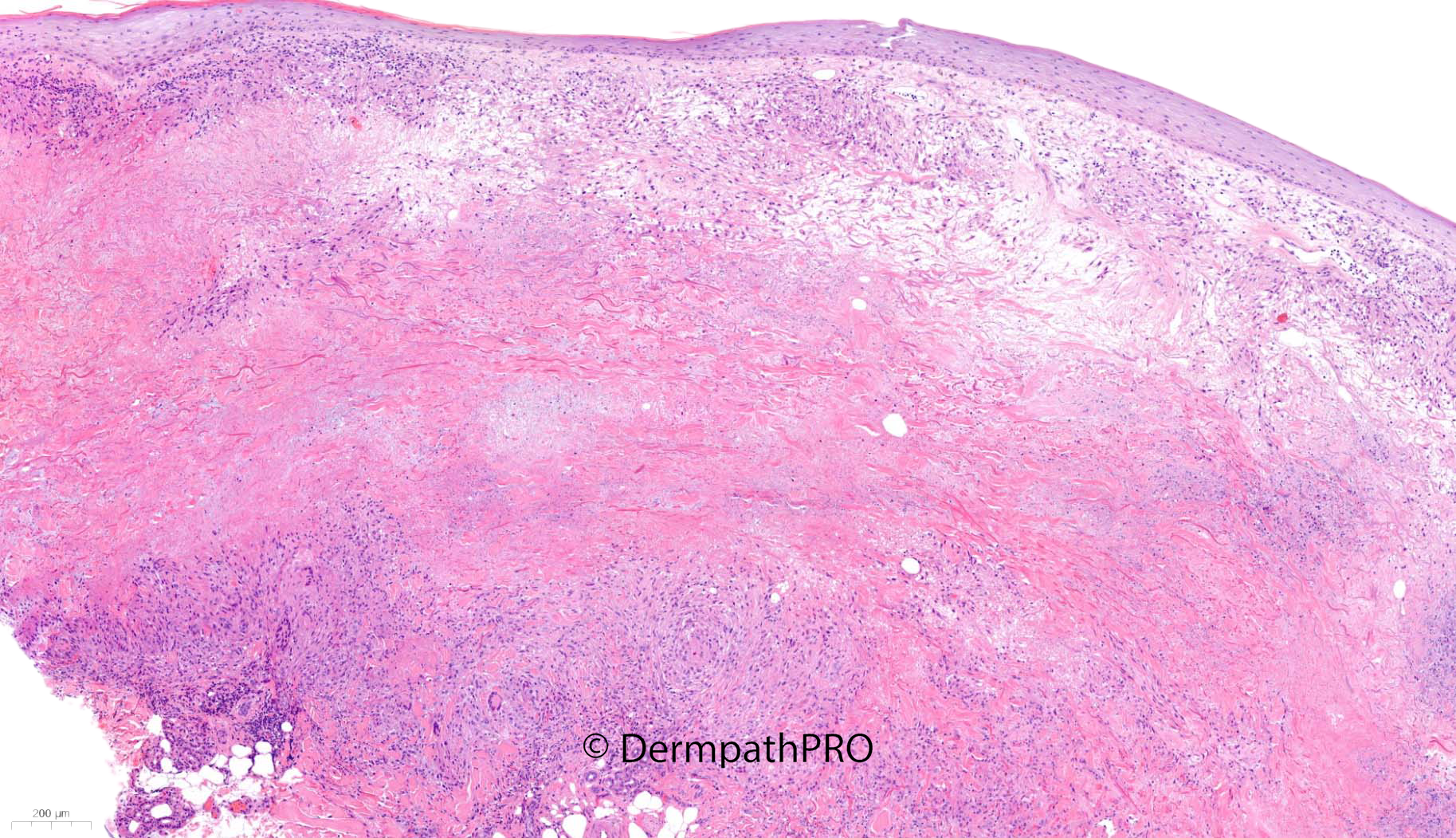
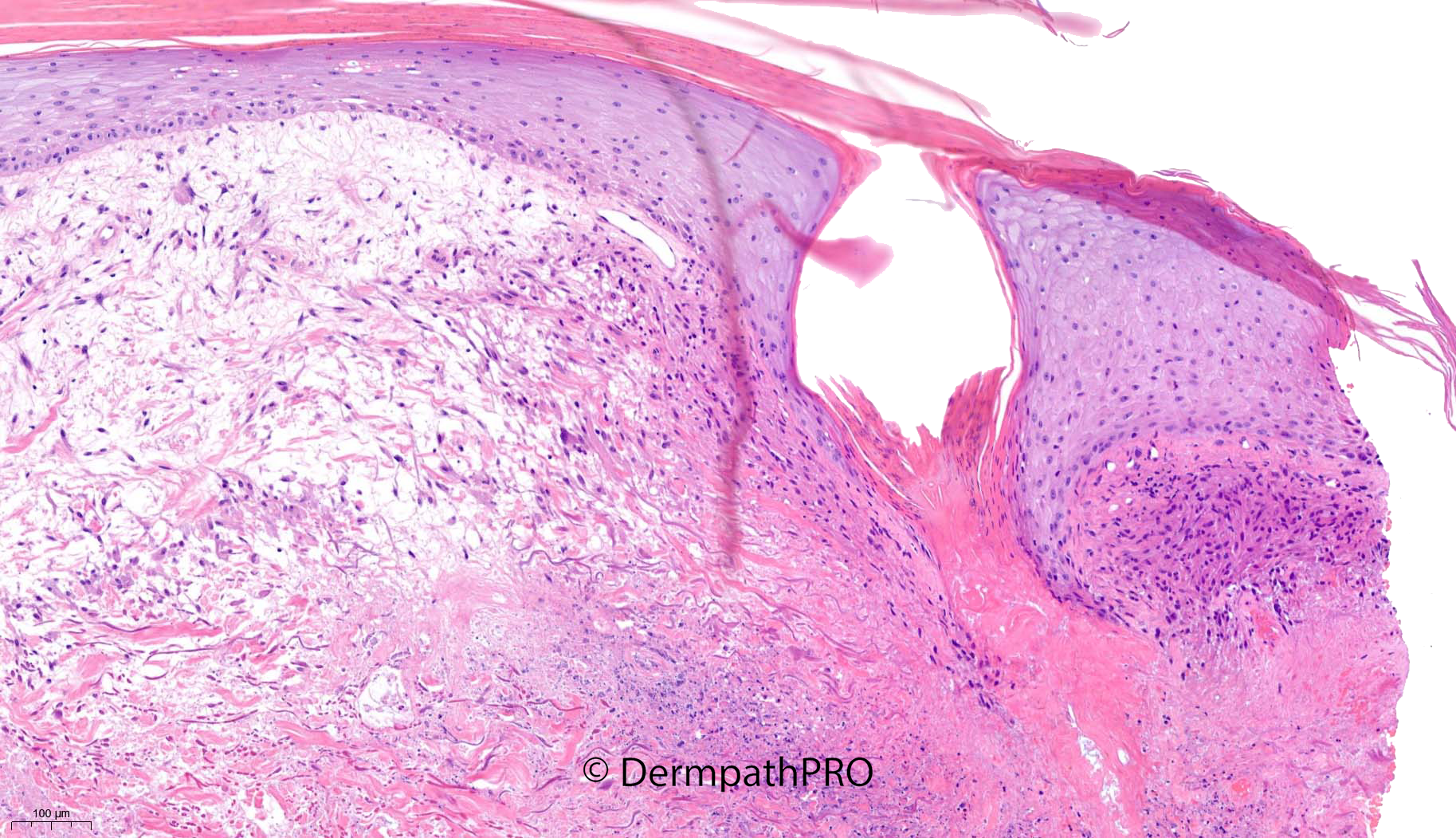
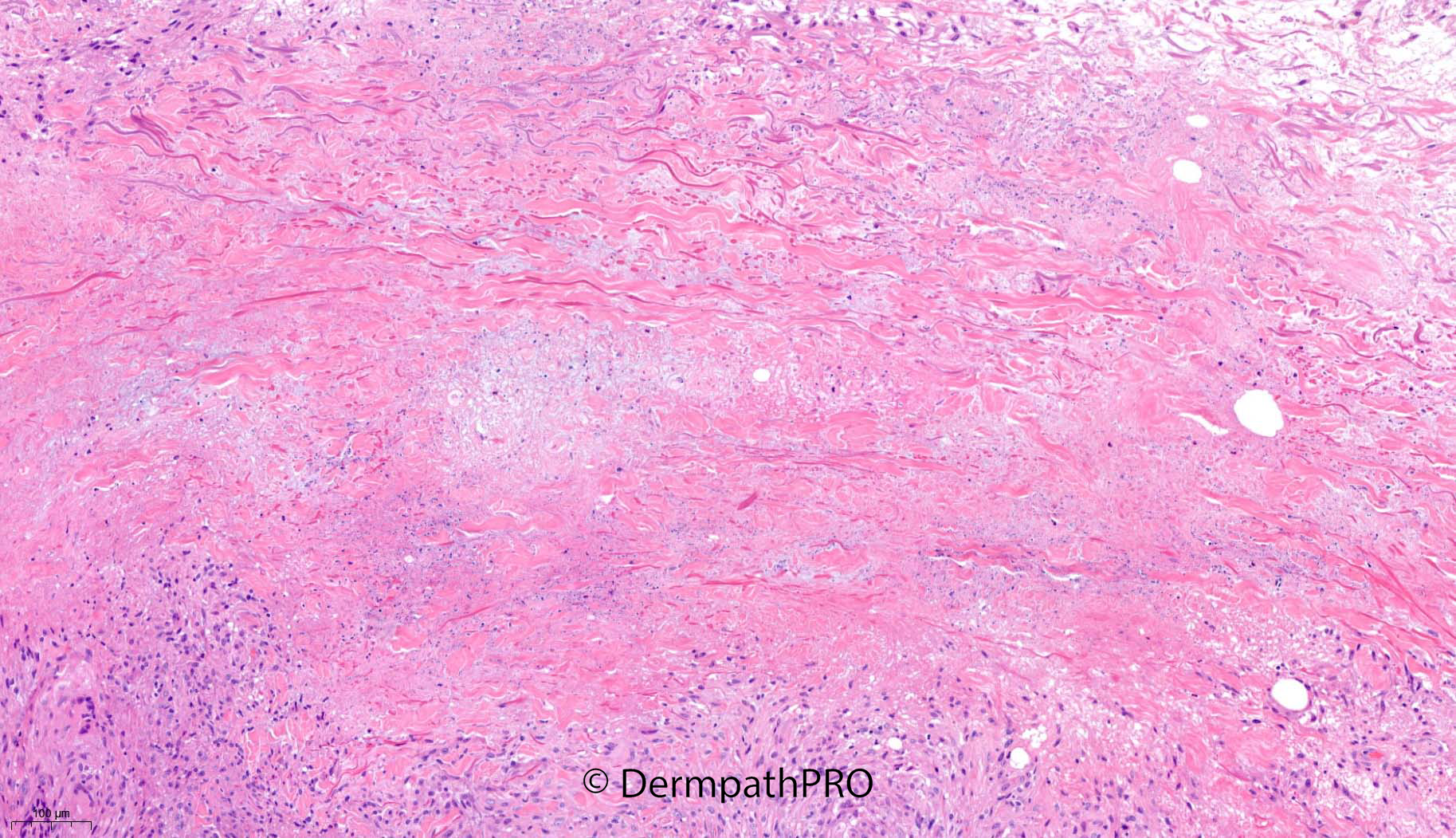
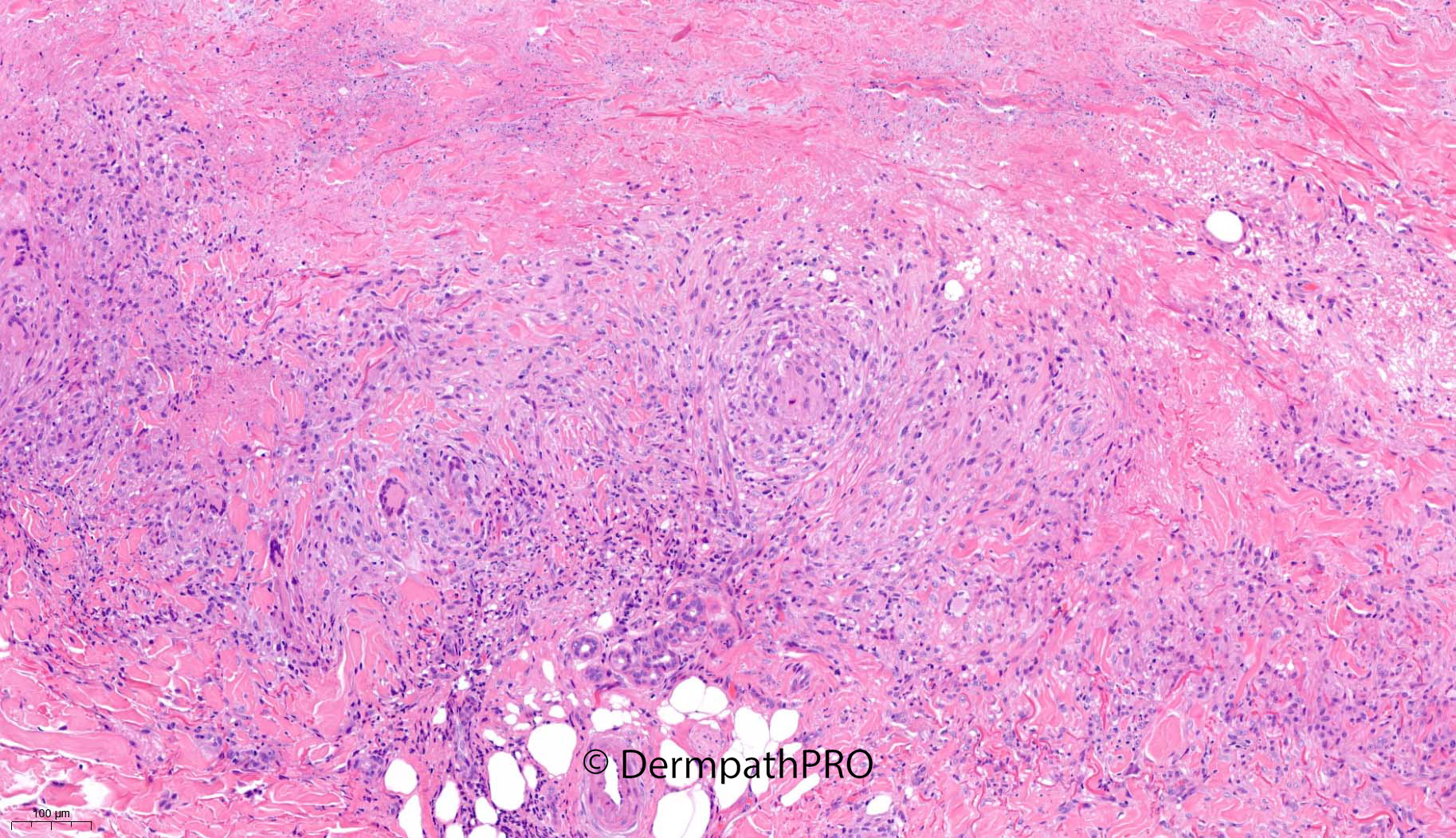
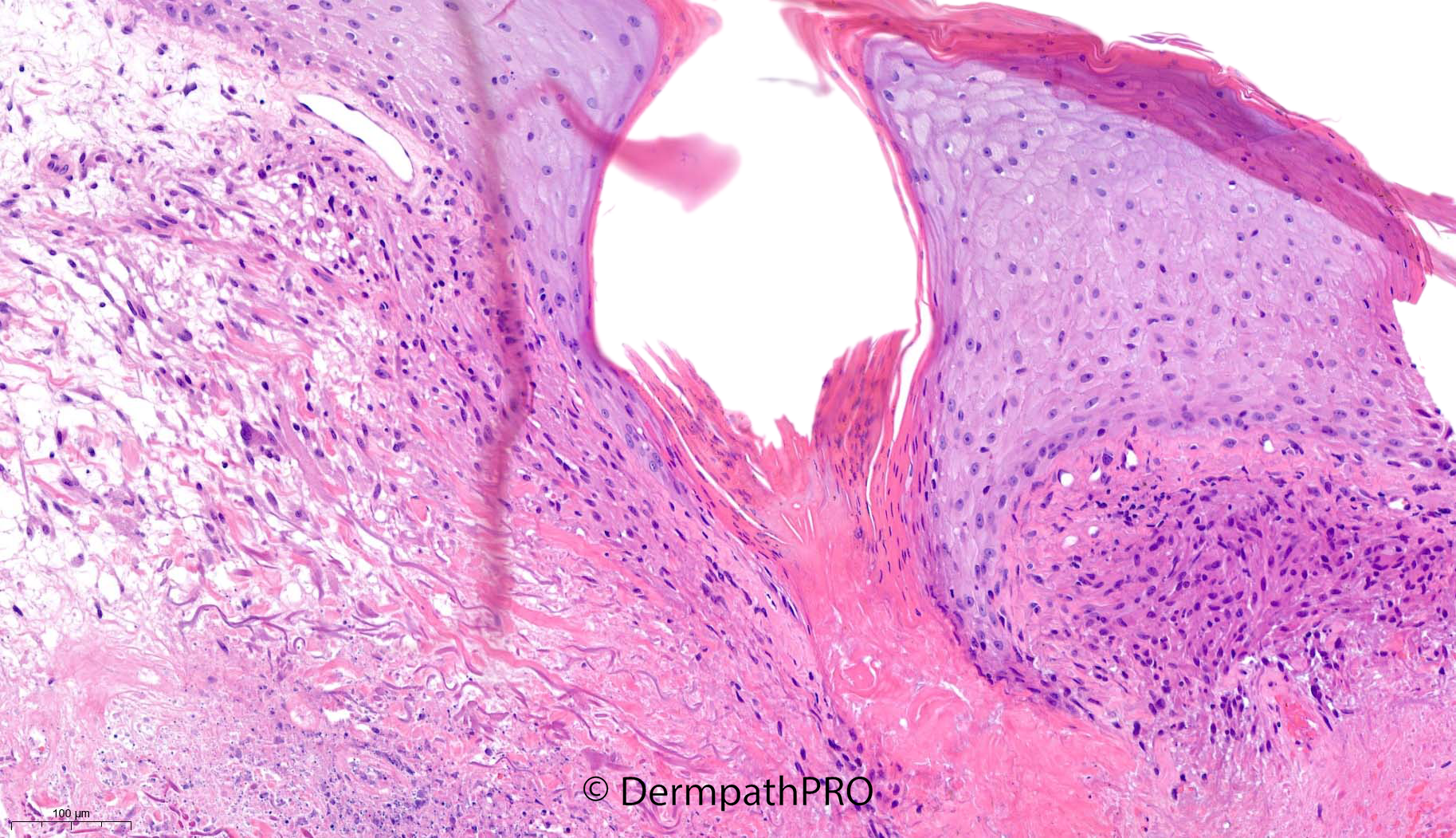
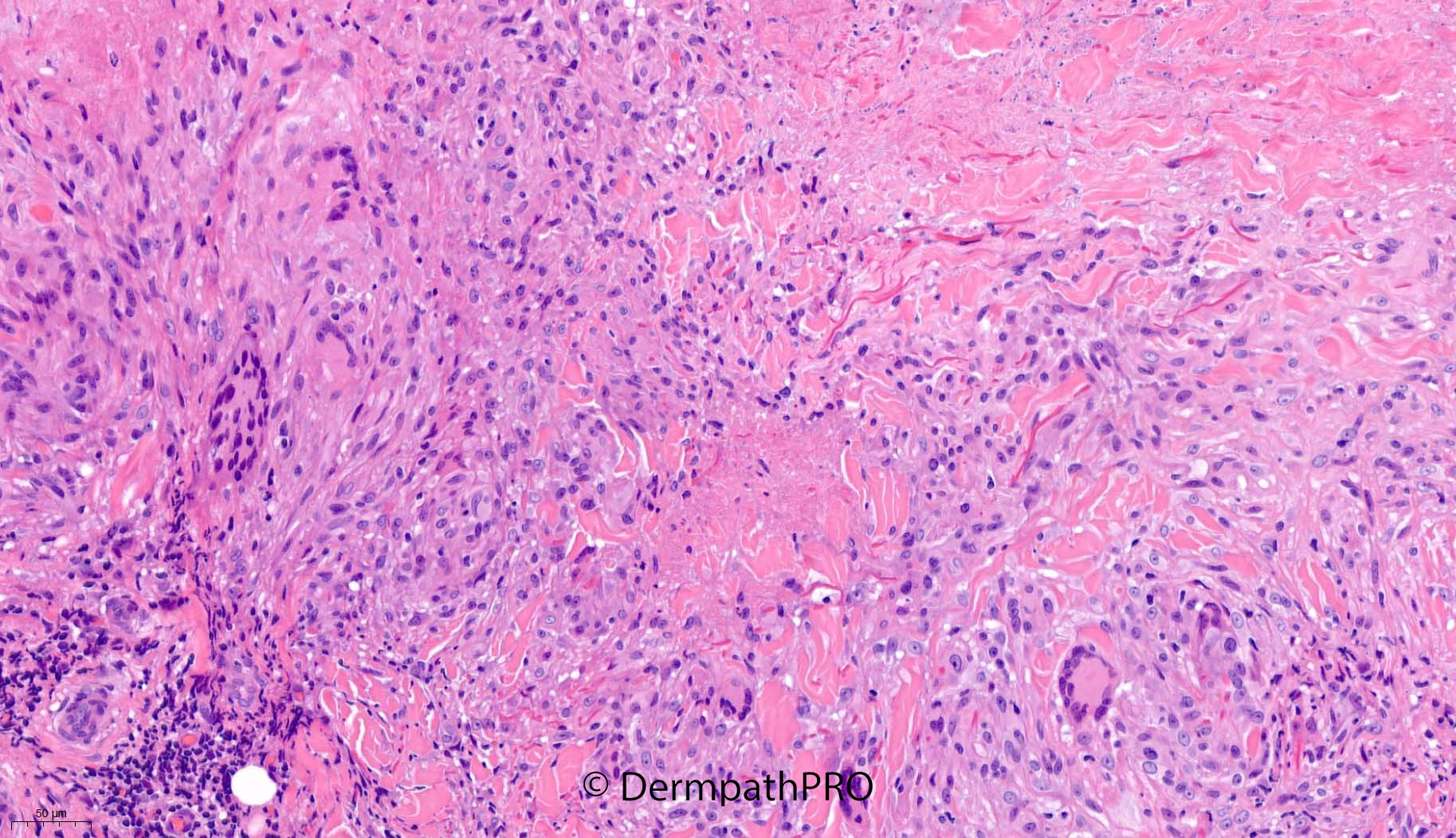
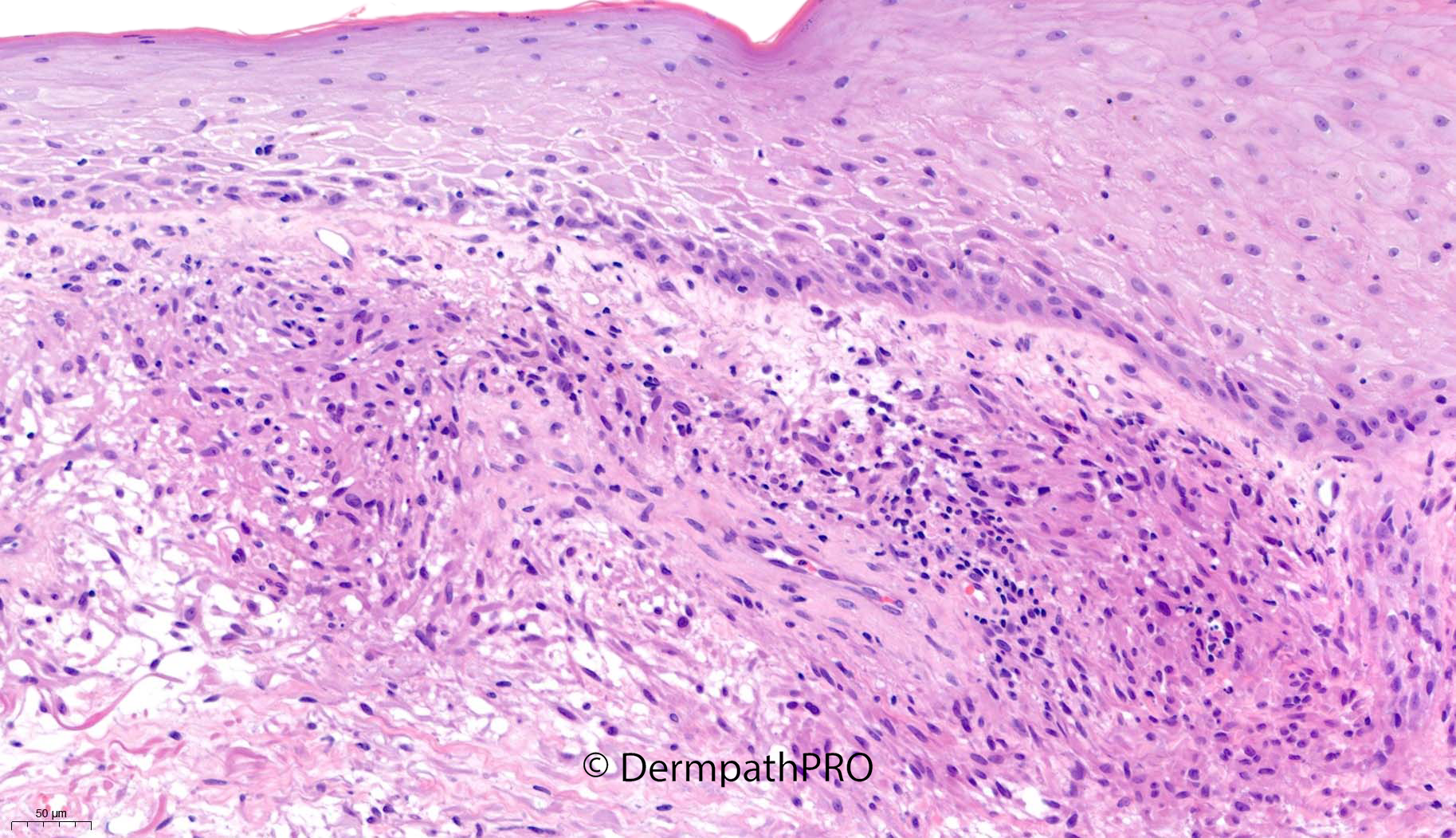
62F biopsy of rash right upper arm, previous history of breast cancer


Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.