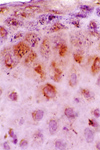
The guardians of the skin immune system
 It has been well established that the epithelia are major components of the immune system. Together with secondary lymphoid organs (ig. lymph nodes, Payer´s patch, etc.), they comprise the activation sites of the Skin and Mucosal Immune Systems, also known as Peripheral or Tegumentary Immune System. Therefore, the epidermis is an essential place for immunemodulation.
It has been well established that the epithelia are major components of the immune system. Together with secondary lymphoid organs (ig. lymph nodes, Payer´s patch, etc.), they comprise the activation sites of the Skin and Mucosal Immune Systems, also known as Peripheral or Tegumentary Immune System. Therefore, the epidermis is an essential place for immunemodulation. Base on a series of articles by [b]Ralf Paus[/b] and collaborators from the University of Hamburg in Germany, in relation to hair follicle as a zone of immune privilege, we now know that a series of molecules produced by keratinocytes may play a key role in controlling skin homeostasis. These molecules are bioactive peptides, such as alpha-MSH (alpha-melanocyte-stimulating hormone), IGF-1 (insulin-like growth factor 1), IL-10, IL-6 and TGF-beta1 (transforming growth factor-beta1). Paus considered these molecules the guardians of the immune homeostasis.
For example, the events that occur in wound-healing may place these ideas into context. Recent evidences suggest that the release of enzymes generates by trauma, such as tryptases, promote epithelial cell division and production of chemokines such as IL-8 and ICAM-1 that attract leukocytes to the injury site. Tryptases also activates mast cells and Langerhans cells, and generate kininogen and kinins that are important for the formation and remodeling of the intracellular matrix. In addition, these enzymes mediate PAR2 (protease-activated receptor 2) expression by endothelial cells, which promotes leukocyte recruitment. Essential factors such as IL-6, TGF-beta, platelet-activating endothelial factor (PAF), alpha-MSH and IGF-I are altered by the wound, enabling the recruitment of cells with active dermotropism.
Moreover, injury or any another antigenic stress increase the amount of CRH (corticotropin-releasing hormone) and NGF (nerve growth factor) in the skin, which may be secreted also by activated mast cells upon stimulation by them or by CGRP (calcitonin-gene related peptide) or NT (neurotensin). Concomitantly, tryptases produced by activated mast cells induce inflammatory neuropeptides, such as SP (substance P), via PAR2-dependent pathways, resulting in an autocrine and/or paracrine mechanism of mast-cell activation with subsequent NGF production besides other inflammatory cytokines.
It is important to keep an eye on these guardians of the immune homeostasis, more that in the inflammatory response, which most probably are an epiphenomenon.
[b]Recommended reading:[/b]
1. Namazi MR. Possible molecular mechanisms to account for the involvement of tryptase in the pathogenesis of psoriasis. Autoimmunity. 2005, 38:449-52.
2. Paus R, Nickoloff BJ, Ito T. A ‘hairy’ privilege. Trends Immunol. 2005, 26:32-40.
3. Paus, R, Ito, N, Takigawaw, M, Ito, T. The Hair Follicle and Immune Privilege.JID Symposium Proceedings 8:188 ^194, 2003
4. Paus R, Theoharides TC, Arck PC. Neuroimmunoendocrine circuitry of the 'brain-skin connection'. Trends Immunol. 2006 Jan;27(1):32-9.



2 Comments
Recommended Comments